Volume 13, Number 3—March 2007
Research
Population-based Laboratory Surveillance for AmpC β-Lactamase–producing Escherichia coli, Calgary
Abstract
In the Calgary Health Region during 2000–2003, prospective, active, population-based laboratory surveillance for all cefoxitin-resistant Escherichia coli isolates was performed. Isolates were screened with an inhibitor-based disk test, and plasmid-mediated types were identified by multiplex PCR with sequencing. A total of 369 AmpC β-lactamase–producing E. coli isolates were identified; annual incidence rates were 1.7, 4.3, 11.2, and 15 per 100,000 residents for each year, respectively. AmpC β-lactamase–producing E. coli was 5× more likely to be isolated from female than male patients across all age groups except <1 year. Of these isolates, 83% were community onset, and urine was the principal site of isolation (90% of patients). PCR showed that 125 (34%) were positive for blacmy genes; sequencing identified these enzymes to be CMY-2. In this large Canadian region, AmpC β-lactamase–producing E. coli is an emerging community pathogen that commonly causes urinary tract infections in older women.
Organisms that produce plasmid-mediated AmpC β-lactamases were first reported in the 1980s (1). These β-lactamases are derivatives of the chromosomally encoded clavulanate-resistant AmpC cephalosporinases of bacteria such as Enterobacter spp., Citrobacter freundii, Morganella morganii, Aeromonas spp., and Hafnia alvei (2). These enzymes have been reported in Escherichia coli, Klebsiella pneumoniae, K. oxytoca, Salmonella spp., Enterobacter aerogenes, and Proteus mirabilis. Because the genes are typically encoded on large plasmids that contain additional antimicrobial resistance genes, therapeutic options are limited (3).
E. coli possess a chromosomal gene that encodes for an AmpC β-lactamase. Usually, low amounts of β-lactamases are produced because the AmpC gene is regulated by a weak promoter and a strong attenuator. These E. coli isolates are sensitive to the cephamycins (4). However, surveys of resistance mechanisms in cephamycin-resistant isolates have identified promoter or attenuator mutations that result in the upregulation of AmpC β-lactamase production; these isolates are referred to as AmpC hyperproducers (5). Occasionally, cephamycin-resistant strains produce plasmid-mediated β-lactamases such as CMY-2, which are derived from bacteria with chromosomally encoded AmpC cephalosporinases (3). In addition, altered expression of outer membrane proteins constituting porins can also contribute to cephamycin resistance (6).
Methods for detecting E. coli AmpC hyperproducers or isolates that produce plasmid-mediated cephalosporinases are technically demanding for clinical laboratories. Although nonsusceptibility to the cephamycins suggests increased production of AmpC β-lactamases, organisms that produce these types of enzymes often go undetected and have been responsible for several nosocomial outbreaks (2,7).
Surveillance studies of organisms that produce plasmid-mediated AmpC β-lactamases, especially among community isolates, are needed (8). We noticed an increase in cephamycin-resistant E. coli isolates in the Calgary Health Region (CHR) during 2002 and 2003 (from 0.1% of all E. coli isolated in 2000 to 1.3% in 2003). To our knowledge, no surveillance studies have investigated the population-based epidemiology of AmpC β-lactamase–producing E. coli (i.e., hyperproducers or plasmid-mediated enzymes), although studies have shown the widespread distribution of these isolates in Europe and North America (2,9–11). Our objectives were to define the population-based incidence of infections caused by E. coli that produce increased levels of AmpC β-lactamases in a large well-defined Canadian region and investigate whether plasmid-mediated types were present in this population.
Patient Population
CHR provides all publicly funded healthcare services to the >1 million persons residing in the cities of Calgary and Airdrie and numerous adjacent surrounding communities covering an area of 37,000 km2 (www.health.gov.ab.ca/regions/RHA_comm3.html). Acute care is provided mainly through 1 pediatric hospital and 3 large hospitals for adults. A centralized laboratory (Calgary Laboratory Services; CLS) performs the routine clinical microbiology services for the community, e.g., nursing homes, physicians’ offices, community collection sites (where outpatients submit specimens for investigation purposes), and hospital sites within the CHR. Our base study population consisted of all patients from whom cefoxitin-resistant E. coli was first identified by CLS from January 1, 2000, through December 31, 2003.
Population-based Surveillance.
Prospective, active, population-based, laboratory surveillance for all cefoxitin-resistant E. coli isolates was performed by CLS; all cefoxitin-resistant E. coli isolates were included in this study. We used the laboratory information system at CLS (PathNet Classic version 306, Cerner, Kansas City, MO, USA) to determine basic demographic information (age, sex, specimen submission site, date of hospital admission) and microbiologic data (location of isolate on patient and antimicrobial-susceptibility testing results) for all patients. Isolates were frozen and stored in batches for further analyses. Community-onset isolates were the first cultures obtained from outpatients or inpatients within 2 days of hospital admission. Hospital-onset isolates were the first cultures taken >2 days after admission to a hospital.
Clinical Microbiology and Molecular Laboratory Testing
We included consecutive nonduplicate isolates of E. coli that were intermediately resistant or resistant to cefoxitin (MIC>8 μg/mL) and that were collected at CLS during January 2000 through December 2003 and isolated from clinical specimens by standard microbiology techniques. During June 2001, we cultured urine samples that had positive screening results from an ATPase-luciferase assay and those specifically requested by a physician (12). Strains were identified to the species level by using Vitek (Vitek AMS; bioMérieux Vitek Systems Inc., Hazelwood, MO, USA.). MICs to the following drugs were determined by Vitek: imipenem, gentamicin, tobramycin, trimethoprim-sulfamethoxazole, and ciprofloxacin. Results were interpreted according to the Clinical and Laboratory Standards Institute criteria for broth dilution (13).
Clinical isolates of cefoxitin-resistant E. coli were tested for AmpC β-lactamases by using the combination of the AmpC β-lactamase inhibitor Syn 2190 and cefotetan disks as described (14). All isolates with an AmpC β-lactamase were further investigated for plasmid-mediated AmpC β-lactamase genes by using multiplex PCR conditions and primers as described (15). These included enzymes that originated from the chromosomally encoded AmpC cephalosporinases of bacteria. Genes of the CMY-positive isolates were identified by cycle sequencing the full-length amplified products with conditions and different primers as described (16).
Analysis
All analyses were performed by using Stata version 9.0 (Stata Corp., College Station, TX, USA). Variables were assessed before analysis by using histograms to identify underlying distribution. Means with standard deviations were used to describe normally or near normally distributed variables and were compared by using the Student t test. Medians with interquartile ranges (IQRs) were used to describe nonnormally distributed variables and were compared by using the Mann-Whitney U test. Differences in proportions were compared by using the Fisher exact test. Incidence rates (per 100,000 population per year) were calculated by using the annual number of new cases among CHR residents as the numerator and regional population estimates for each year from 2000 through 2003 (December 2003 boundaries) of the CHR as the denominator. Patients with Alberta healthcare numbers were considered CHR residents and were included; those with out-of-province healthcare numbers were excluded. Age- and sex-specific incidence rates were calculated by dividing the number of new cases within a subgroup by the population at risk. Risk ratios (RR) for incidence rates among demographic subgroups were calculated by dividing the incidence rate with the factor (as opposed to without) and were reported with 95% confidence intervals (CIs) as described (17).
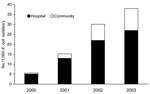
During the 4-year study period, 78,275 E. coli isolates were obtained from 51,735 patients; 72,756 (93%) isolates were classified as community onset and 5,519 (7%) as hospital onset. For 408 (0.7%) patients, a cefoxitin-resistant E. coli isolate was identified. The number of isolates (per first isolate per patient per year) increased significantly each year: 23 (0.1%) of 17,989 patients in 2000, 53 (0.3%) of 15,907 in 2001, 141 (1%) of 14,583 in 2002, and 191 (1.3%) of 14,319 in 2003 (p<0.0001 for 2000 compared with 2003). Of the 408 cefoxitin-resistant isolates, 384 (94%) were available for further analysis. Of these, 369 (96%) were positive for AmpC β-lactamases according to the Syn 2190 inhibitor disk screen test, and of the 369, 359 (97%) were from CHR residents. The number of isolates identified in CHR residents during 2000, 2001, 2002, and 2003 were 18, 46, 123, and 172, with annualized incidence rates of 1.7, 4.3, 11.2, and 15 per 100,000, respectively.
Seasonal variability in the occurrence of AmpC β-lactamase–producing E. coli isolates was moderate; the lowest rates of isolation were in early winter and spring, and the highest rates were in late summer and fall (Figure 1). Of the 369 isolates, 61 (17%) were classified as hospital onset. Of the 308 (83%) community-onset isolates, 54 were submitted from hospital emergency departments, 24 from inpatients within the first 2 days of admission, 20 from nursing home residents, and the rest from outpatients. While the number of hospital-onset AmpC β-lactamase–producing E. coli isolates increased gradually during 2000–2003 (5, 12, 20, 24 each year, respectively), the number of community-onset isolates increased dramatically (13, 35, 108, 152 each year, respectively). The increase among the acute care centers was not the result of clustering of patients in a specific acute care center. However, in relation to all first E. coli isolates per year per patient tested by CLS, AmpC β-lactamase–producing E. coli were proportionally more likely to be obtained as hospital-onset isolates (Figure 2).
The median age of the cohort was 51.1 (IQR 27.3–74.3) years; most (310; 84%) patients were female. Incidence of AmpC β-lactamase–producing E. coli significantly increased in association with increasing age (Figure 3). Risk for isolation of AmpC β-lactamase–producing E. coli was 5× higher for female than male residents (14.0 vs. 2.6 per 100,000 per year; RR 5.4; 95% CI 4.04–7.31; p<0.0001); this increased risk was observed across all age groups with the exception of the very young (< 1 year) (Figure 3).
Among the 369 AmpC β-lactamase–producing isolates, the principal site of isolation was the urinary tract for 333 (90%) patients, bloodstream for 20 (5%), respiratory tract for 8 (2%), soft tissue for 5 (1%), and abdomen for 3 (1%). Of these same 369 isolates, 73 (20%) were not susceptible to trimethoprim-sulfamethoxazole, 32 (9%) to tobramycin, 54 (14%) to gentamicin, and 33 (9%) to ciprofloxacin. No resistance to imipenem was detected.
Multiplex PCR amplified a 462-bp amplicon among 125 (34%) of the 369 AmpC β-lactamase–producing isolates that was consistent with the plasmid-encoded types of AmpC β-lactamases originating from the chromosomal gene of Citrobacter freundii (CMY types) (15). No other types of plasmid-mediated AmpC enzymes were present. Sequence analysis of full-length PCR products on 15 randomly selected isolates showed 100% identity to blaCMY-2 (18). The Table shows features of CMY-type and non–CMY-type AmpC β-lactamases. With the exception of a higher rate of gentamicin resistance among CMY-2–positive strains (Table), E. coli isolates that produced CMY-types and those that produced non-CMY types of AmpC β-lactamases did not differ according to year of study, principal site of isolation, or demographics.
Limited data are available regarding hyperproduction of AmpC β-lactamases among E. coli in the United States and Canada. A study from Canada showed that most cephamycin-resistant E. coli from the Toronto area in 2001 had different promoter and attenuator mutations in the chromosomal AmpC cephalosporinases (5). Jacoby and colleagues found plasmid-mediated AmpC-type resistance in 7 of 75 of ceftazidime-resistant E. coli from 25 US states; 2 of these isolates produced CMY-2 (19). Mulvey and colleagues studied 232 cefoxitin-resistant E. coli from 12 hospitals in Canada and found that 25 (11%) strains contained CMY-2 and 51 (22%) had different promoter and attenuator mutations (20). E. coli that produce CMY-2 have also had been isolated from food-producing animals in Canada and the United States (21,22).
Laboratory tests that use inhibitors of AmpC β-lactamases in E. coli successfully distinguish between isolates that have altered expression of outer membrane proteins and isolates that produce increased levels of AmpC β-lactamases (23,24). Multiplex PCR that detects the different types of plasmid-mediated AmpC β-lactamases is the most practical way to differentiate between isolates with promoter or attenuator mutations and those with plasmid-mediated cephalosporinases (15). Our study screened all cefoxitin-resistant E. coli for AmpC β-lactamases and used multiplex PCR to identify plasmid-mediated types. However, the cephalosporinases that originated from H. alvei (e.g., ACC types) are not detected by our phenotypic method. In our study, >90% of cefoxitin-resistant strains produced increased levels of AmpC cephalosporinases; 125 (34%) of these 369 were positive for CMY-2, much higher than the 11% reported by Mulvey et al. (20). None of the other plasmid-mediated AmpC types were present in E. coli isolated from patients in the CHR.
Some studies have recognized a role of AmpC β-lactamase–producing E. coli in nosocomial infections (2,3,7); however, these studies were based at institutions and did not survey community-based laboratories. Because our surveillance included all clinical specimens from hospital and community sites, we are highly unlikely to have missed many isolates. We observed that in the CHR, AmpC β-lactamase–producing E. coli is predominantly a community-onset pathogen. The designs of other studies in the literature (19,20) make it unclear whether AmpC β-lactamase–producing E. coli is an important cause of community-onset infections elsewhere. A community outbreak in CHR during 2002 resulted from CMY-2–producing Salmonella enterica serotype Newport associated with the handling of pet treats (25). A previous study from our center has shown that these salmonella isolates share similar-size plasmids with CMY-2–producing E. coli of multiple pulsed-field gel electrophoresis types identified in our study (D.B. Gregson, unpub. data). Thus, E. coli and Salmonella spp. may share similar plasmids.
Several investigations have shown that animals may represent a source for dissemination of AmpC-encoding genes from E. coli to humans. Evidence of CMY-2–producing isolates in cattle (26), pork (27), poultry (21,28), and dogs and cats (29) is of concern because food-producing animals and domestic pets may act as reservoirs for resistant organisms. Therefore, factors that lead to the high rate of isolation of AmpC β-lactamase–producing E. coli in patients from the community require further exploration.
Ours is the first report of the population epidemiology of AmpC β-lactamase–producing E. coli. We restricted our study to E. coli because other plasmid-mediated AmpC-producing organisms are rare in our region (only 17 patients infected with AmpC-producing K. pneumoniae and 12 with AmpC-producing Salmonella spp. were identified at CLS during this study period). We determined demographic risk factors associated with the isolation of AmpC β-lactamase–producing E. coli by comparing patient demographic characteristics with our well-defined base population. In these analyses, female and older patients were at much higher risk than male and younger patients (Figure 3). These results are similar to those we obtained in a previous study from CHR that investigated the population epidemiology of infections caused by extended-spectrum β-lactamase (ESBL)–producing E. coli during 2000–2002 (30). Incidence of ESBL-producing isolates was stable for the 3 years; incidence rates in 2000, 2001, and 2002 were 5.0, 5.6, and 5.7 per 100,000, respectively. These rates differ from those for AmpC β-lactamase–producing E. coli in this study, which had rates of 1.7, 4.3, and 11.2 per 100,000 for these 3 years, respectively. Our previous study also showed that most ESBL-producing E. coli from our region isolated during the same period were resistant to gentamicin and ciprofloxacin (30); in our current study, only 14% and 9% of AmpC β-lactamase–producing isolates were resistant to gentamicin and ciprofloxacin, respectively. Thus, susceptibility patterns differ between ESBL- and AmpC β-lactamase–producing E. coli from the CHR isolates during the same period.
The population-based design has some methodologic limitations. First, because this was a laboratory-based study, detailed clinical information (e.g., prior receipt of antimicrobial drugs, travel, exposure to food and water, underlying concurrent conditions) was not available. We were therefore unable to determine whether the isolates in this study truly caused infection. The lack of detailed clinical information is an inherent limitation to all laboratory-based studies. Second, isolates were defined as either community- or hospital-onset on the basis of their location of submission. Although this may in part reflect where these organisms were acquired, some isolates classified as community onset may have been associated with healthcare (31). Third, incidence rates were based on the assumption that all persons with Alberta healthcare numbers were CHR residents. We estimate that 10%–15% of patients in this study may have resided within other health regions in Alberta rather than within CHR. As a result, our incidence rates may be slightly higher than the true values.
In conclusion, this study demonstrates that AmpC β-lactamase–hyperproducing E. coli is an emerging community pathogen in the CHR with public health implications. Our results warrant increased efforts at surveillance for and the study of risk factors associated with the acquisition of these isolates in order to guide future prevention and control measures
Dr Pitout is an associate professor in the Department of Pathology and Laboratory Medicine and the Department of Microbiology and Infectious Diseases, University of Calgary, and a medical microbiologist in the Division of Microbiology, Calgary Laboratory Services. His major research and teaching interests are resistance mechanisms of antimicrobial drugs, especially newer types of β-lactamases, in gram-negative bacteria and susceptibility testing in the clinical laboratory.
Acknowledgments
We thank Wanda Weisser for her technical support and Terry Ross for database management.
This study was funded by a grant from the Calgary Laboratory Services (# 73-1357).
References
- Papanicolaou GA, Medeiros AA, Jacoby GA. Novel plasmid-mediated β-lactamase (MIR-1) conferring resistance to oxyimino- and alpha-methoxy β-lactams in clinical isolates of Klebsiella pneumoniae.Antimicrob Agents Chemother. 1990;34:2200–9.PubMedGoogle Scholar
- Philippon A, Arlet G, Jacoby GA. Plasmid-determined AmpC-type β-lactamases.Antimicrob Agents Chemother. 2002;46:1–11. DOIPubMedGoogle Scholar
- Jacoby GA, Munoz-Price LS. The new β-lactamases.N Engl J Med. 2005;352:380–91. DOIPubMedGoogle Scholar
- Olsson O, Bergstrom S, Normark S. Identification of a novel ampC β-lactamase promoter in a clinical isolate of Escherichia coli.EMBO J. 1982;1:1411–6.PubMedGoogle Scholar
- Forward KR, Willey BM, Low DE, McGeer A, Kapala MA, Kapala MM, Molecular mechanisms of cefoxitin resistance in Escherichia coli from the Toronto area hospitals.Diagn Microbiol Infect Dis. 2001;41:57–63. DOIPubMedGoogle Scholar
- Clarke B, Hiltz M, Musgrave H, Forward KR. Cephamycin resistance in clinical isolates and laboratory-derived strains of Escherichia coli, Nova Scotia, Canada.Emerg Infect Dis. 2003;9:1254–9.PubMedGoogle Scholar
- M'Zali FH, Heritage J, Gascoyne-Binzi DM, Denton M, Todd NJ, Hawkey PM. Transcontinental importation into the UK of Escherichia coli expressing a plasmid-mediated AmpC-type β-lactamase exposed during an outbreak of SHV-5 extended-spectrum β-lactamase in a Leeds hospital.J Antimicrob Chemother. 1997;40:823–31. DOIPubMedGoogle Scholar
- Hanson ND. AmpC β-lactamases: What do we need to know for the future?J Antimicrob Chemother. 2003;52:2–4. DOIPubMedGoogle Scholar
- Brinas L, Lantero M. de D, I, Alvarez M, Zarazaga M, and Torres C. Mechanisms of resistance to expanded-spectrum cephalosporins in Escherichia coli isolates recovered in a Spanish hospital.J Antimicrob Chemother. 2005;56:1107–10. DOIPubMedGoogle Scholar
- Goossens H, Grabein B. Prevalence and antimicrobial susceptibility data for extended-spectrum b-lactamase- and AmpC-producing Enterobacteriaceae from the MYSTIC Program in Europe and the United States (1997–2004).Diagn Microbiol Infect Dis. 2005;53:257–64. DOIPubMedGoogle Scholar
- Kaye KS, Gold HS, Schwaber MJ, Venkataraman L, Qi Y, De Girolami PC, Variety of β-lactamases produced by amoxicillin-clavulanate-resistant Escherichia coli isolated in the northeastern United States.Antimicrob Agents Chemother. 2004;48:1520–5. DOIPubMedGoogle Scholar
- Semeniuk H, Noonan J, Gill H, Church DL. Evaluation of the Coral UTI Screen system for rapid automated screening of significant bacteriuria in a regional centralized laboratory.Diagn Microbiol Infect Dis. 2002;44:7–10. DOIPubMedGoogle Scholar
- National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing; fourteenth informational supplement M100-S14. Wayne (PA): The Committee; 2004.
- Black JA, Thomson KS, Buynak JD, Pitout JD. Evaluation of β-lactamase inhibitors in disk tests for detection of plasmid-mediated AmpC β-lactamases in well-characterized clinical strains of Klebsiella spp.J Clin Microbiol. 2005;43:4168–71. DOIPubMedGoogle Scholar
- Perez-Perez FJ, Hanson ND. Detection of plasmid-mediated AmpC β-lactamase genes in clinical isolates by using multiplex PCR.J Clin Microbiol. 2002;40:2153–62. DOIPubMedGoogle Scholar
- Hanson ND, Moland ES, Hossain A, Neville SA, Gosbell IB, Thomson KS. Unusual Salmonella enterica serotype Typhimurium isolate producing CMY-7, SHV-9 and OXA-30 β-lactamases.J Antimicrob Chemother. 2002;49:1011–4. DOIPubMedGoogle Scholar
- Laupland KB, Church DL, Mucenski M, Sutherland LR, Davies HD. Population-based study of the epidemiology of and the risk factors for invasive Staphylococcus aureus infections.J Infect Dis. 2003;187:1452–9. DOIPubMedGoogle Scholar
- Bauernfeind A, Stemplinger I, Jungwirth R, Giamarellou H. Characterization of the plasmidic β-lactamase CMY-2, which is responsible for cephamycin resistance.Antimicrob Agents Chemother. 1996;40:221–4.PubMedGoogle Scholar
- Alvarez M, Tran JH, Chow N, Jacoby GA. Epidemiology of conjugative plasmid-mediated AmpC β-lactamases in the United States.Antimicrob Agents Chemother. 2004;48:533–7. DOIPubMedGoogle Scholar
- Mulvey MR, Bryce E, Boyd DA, Ofner-Agostini M, Land AM, Simor AE, Molecular characterization of cefoxitin-resistant Escherichia coli from Canadian hospitals.Antimicrob Agents Chemother. 2005;49:358–65. DOIPubMedGoogle Scholar
- Poppe C, Martin LC, Gyles CL, Reid-Smith R, Boerlin P, McEwen SA, Acquisition of resistance to extended-spectrum cephalosporins by Salmonella enterica subsp. enterica serovar Newport and Escherichia coli in the turkey poult intestinal tract.Appl Environ Microbiol. 2005;71:1184–92. DOIPubMedGoogle Scholar
- Winokur PL, Vonstein DL, Hoffman LJ, Uhlenhopp EK, Doern GV. Evidence for transfer of CMY-2 AmpC β-lactamase plasmids between Escherichia coli and Salmonella isolates from food animals and humans.Antimicrob Agents Chemother. 2001;45:2716–22. DOIPubMedGoogle Scholar
- Black JA, Thomson KS, Pitout JD. Use of β-lactamase inhibitors in disk tests to detect plasmid-mediated AmpC β-lactamases.J Clin Microbiol. 2004;42:2203–6. DOIPubMedGoogle Scholar
- Coudron PE. Inhibitor-based methods for detection of plasmid-mediated AmpC β-lactamases in Klebsiella spp., Escherichia coli, and Proteus mirabilis.J Clin Microbiol. 2005;43:4163–7. DOIPubMedGoogle Scholar
- Pitout JD, Reisbig MD, Mulvey M, Chui L, Louie M, Crowe L, Association between handling of pet treats and infection with Salmonella enterica serotype Newport expressing the AmpC β-lactamase, CMY-2.J Clin Microbiol. 2003;41:4578–82. DOIPubMedGoogle Scholar
- Batchelor M, Clifton-Hadley FA, Stallwood AD, Paiba GA, Davies RH, Liebana E. Detection of multiple cephalosporin-resistant Escherichia coli from a cattle fecal sample in Great Britain.Microb Drug Resist. 2005;11:58–61. DOIPubMedGoogle Scholar
- Yan JJ, Hong CY, Ko WC, Chen YJ, Tsai SH, Chuang CL, Dissemination of blaCMY-2 among Escherichia coli isolates from food animals, retail ground meats, and humans in southern Taiwan.Antimicrob Agents Chemother. 2004;48:1353–6. DOIPubMedGoogle Scholar
- Liebana E, Gibbs M, Clouting C, Barker L, Clifton-Hadley FA, Pleydell E, Characterization of β-lactamases responsible for resistance to extended-spectrum cephalosporins in Escherichia coli and Salmonella enterica strains from food-producing animals in the United Kingdom.Microb Drug Resist. 2004;10:1–9. DOIPubMedGoogle Scholar
- Carattoli A, Lovari S, Franco A, Cordaro G, Di Matteo P, Battisti A. Extended-spectrum β-lactamases in Escherichia coli isolated from dogs and cats in Rome, Italy, from 2001 to 2003.Antimicrob Agents Chemother. 2005;49:833–5. DOIPubMedGoogle Scholar
- Pitout JD, Hanson ND, Church DL, Laupland KB. Population-based laboratory surveillance for Escherichia coli–producing extended-spectrum beta-lactamases: importance of community isolates with blaCTX-M genes.Clin Infect Dis. 2004;38:1736–41. DOIPubMedGoogle Scholar
- Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Health care–associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections.Ann Intern Med. 2002;137:791–7.PubMedGoogle Scholar
Figures
Table
Cite This ArticleTable of Contents – Volume 13, Number 3—March 2007
| EID Search Options |
|---|
|
|
|
|
|
|
![Thumbnail of AmpC β-lactamase–producing Escherichia coli isolates per 1,000 E. coli isolates, Calgary Health Region, 2000–2003. Data are averaged over the 4-year period. The presence of plasmid-mediated AmpC β-lactamase genes was determined using multiplex PCR conditions and primers as described [8]. CMY; isolates positive for chromosomal gene of Citrobacter freundii; non-CMY; isolates negative by multiplex PCR.](/eid/images/06-0447-F1-tn.jpg)

Please use the form below to submit correspondence to the authors or contact them at the following address:
Johann D. D. Pitout, Division of Microbiology, Calgary Laboratory Services #9, 3535 Research Rd NW, Calgary, Alberta, Canada T2L 2K8;
Top