Volume 15, Number 2—February 2009
Dispatch
Effect of Free Treatment and Surveillance on HIV-Infected Persons Who Have Tuberculosis, Taiwan, 1993–2006
Abstract
In 1997, Taiwan made highly active antiretroviral therapy (HAART) available without cost to HIV-infected persons; in 2001, a national web-based surveillance system was implemented. Healthcare workers use the system to monitor patients' conditions and can intervene when necessary. Free HAART, coupled with the surveillance system, appears to have increased survival rates of HIV-infected persons with tuberculosis in Taiwan.
Most experts believe that complete and efficient surveillance is the top priority in detecting and preventing outbreaks of emerging infectious diseases, such as tuberculosis (TB) and HIV coinfection (1–3) or influenza virus A (H5N1). In Taiwan, a national web-based surveillance system established in July 2001 provides complete and efficient reporting and management of persons coinfected with HIV and TB and enables healthcare workers to identify noncompliance with therapy and to intervene when necessary. After highly active antiretroviral therapy (HAART) became available free of charge in Taiwan in April 1997, the death rate for HIV-infected persons decreased from 5.7% in 1997 to 1.8% in 2006. To determine whether implementation of the national surveillance system in combination with the availability of free HAART further increased survival rates of HIV-infected persons with TB, we compared their demographic, clinical, and behavioral characteristics during 3 periods: 1) before free HAART was available (1993–1996); 2) after free HAART was available but before the surveillance system was implemented (1998–2000); and 3) after both free HAART and the surveillance system were available (2002–2006).
We obtained data on persons with HIV/AIDS and TB from the national databank at the Centers for Disease Control (CDC Taiwan) of the Department of Health, Taiwan. Coinfection with HIV and TB was defined as HIV infection in persons in whom TB was later diagnosed. A total of 660 persons with both HIV and TB were reported during 1993–2006.
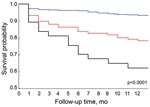
We used Microsoft Excel XP spreadsheet (Microsoft, Redmond, WA, USA) and SAS version 9.1 (SAS Institute Inc., Cary, NC, USA) for statistical analysis. The χ2 goodness-of-fit test with type I error = 0.05 was used to examine differences in demographic, clinical, and behavioral characteristics of persons with HIV and TB coinfection during 1993–2006. Multivariates for analysis were sex and age, results of sputum smear and sputum culture, pulmonary radiographic diagnosis, TB types (extrapulmonary and nonextrapulmonary), mode of HIV transmission, sexual behavior, compliance with HAART, and use of the surveillance system (Table 1). We used the Kaplan-Meier method (4) from SAS to evaluate and compare the effect on survival rates of different factors in persons coinfected with HIV and TB 1 year after reported TB diagnosis.
Kaplan-Meier analysis yielded the following results: 63% of persons coinfected with HIV and TB survived during 1993–1996; 78% survived during 1998–2000; and 93% survived during 2002–2006 (p<0.0001) (Figure). We then applied Cox proportional hazards modeling (5) to each variable to assess the effect on survival rates after implementation of HAART and the surveillance system. Age <45 years, negative sputum smear, availability of free HAART, and implementation of the national surveillance system substantially increased survival rates of persons coinfected with HIV and TB (Table 2).
Many factors can increase survival rates of HIV-infected persons, such as HAART (6–9), prevention of opportunistic infections, patient attitude, healthcare worker knowledge, and promotion of health education. Our data indicate that national web-based surveillance reporting and management, coupled with the availability of free HAART, increase survival rates of persons coinfected with HIV and TB (p<0.0001).
Taiwan’s national web-based surveillance system enables healthcare workers to follow, record, and understand the conditions of patients without geographic limitations. Physicians, public health nurses, health administrators, and other healthcare professionals in local through federal government agencies can use the system to follow up and manage the condition of persons coinfected with HIV and TB. For example, public health nurses from national healthcare centers visit such patients regularly, record treatments, and assess their conditions and compliance with therapy; staff from central health department monitor and supervise the condition of each patient through the system. In this way, the system may increase patients’ compliance and thus their survival rates (10–14).
Dr Tseng is the deputy director of the Division of Surveillance and Nosocomial Infection Control at the Taiwan CDC. Her research interest focuses on coinfection of HIV and TB.
Acknowledgments
We sincerely thank all the medical and public health staff in both local and federal authority to report HIV and TB cases to the Taiwan CDC’s surveillance system and close follow-up of the HIV and TB patients.
This study was supported by the Taiwan CDC.
References
- World Health Organization. Global tuberculosis control, 2008. Surveillance, planning, financing. Geneva: The Organization; 2008 [cited 24 Mar 2008]. Available from http://www.who.int/tb/publications/global_report/2008/download_centre/en/index.html
- Nunn P, Williams B, Floyd K, Dye C, Elzinga G, Raviglione M. Tuberculosis control in the era of HIV. Nat Rev Immunol. 2005;5:819–26. DOIPubMedGoogle Scholar
- Nunn P, Brindle R, Carpenter L, Odhiambo J, Wasunna K, Newnham R, Cohort study of human immunodeficiency virus infection in patients with tuberculosis in Nairobi, Kenya. Analysis of early (6-month) mortality. Am Rev Respir Dis. 1992;146:849–54.PubMedGoogle Scholar
- Kaplan E, Meier P. Non-parametric estimation from incomplete observation. J Am Stat Assoc. 1958;53:457–81. DOIGoogle Scholar
- Cox DR, Oakes D. Analysis of survival data. London: Chapman & Hall; 1984.
- Lim HJ, Okwera A, Mayanja-Kizza H, Ellner JJ, Mugerwa RD, Whalen CC. Effect of tuberculosis preventive therapy on HIV disease progression and survival in HIV-infected adults. HIV Clin Trials. 2006;7:172–83. DOIPubMedGoogle Scholar
- Muga R, Ferreros I, Langohr K, de Olalla PG, Del Romero J, Quintana M, Changes in the incidence of tuberculosis in a cohort of HIV-seroconverters before and after the introduction of HAART. AIDS. 2007;21:2521–7.PubMedGoogle Scholar
- Girardi E, Sabin CA, d'Arminio Monforte A, Hogg B, Phillips AN, Gill MJ, Incidence of tuberculosis among HIV-infected patients receiving highly active antiretroviral therapy in Europe and North America. Clin Infect Dis. 2005;41:1772–82. DOIPubMedGoogle Scholar
- Girardi E, Palmieri F, Cingolani A, Ammassari A, Petrosillo N, Gillini L, Changing clinical presentation and survival in HIV-associated tuberculosis after highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;26:326–31.PubMedGoogle Scholar
- Lew WJ, Lee EG, Bai JY, Kim HJ, Bai GH, Ahn DI, An Internet-based surveillance system for tuberculosis in Korea. Int J Tuberc Lung Dis. 2006;10:1241–7.PubMedGoogle Scholar
- Snodgrass I, Chew SK. A national computer-based surveillance system for tuberculosis notification in Singapore. Tuber Lung Dis. 1995;76:264–70. DOIPubMedGoogle Scholar
- Chew SK, Snodgrass I. A computer-based surveillance system for human immunodeficiency virus infection in Singapore. Singapore Med J. 1995;36:147–51.PubMedGoogle Scholar
- Lenglet A, Hernandez Pezzi G. Comparison of the European Union Disease Surveillance Networks' websites. Euro Surveill. 2006;11:119–22.PubMedGoogle Scholar
- Rolfhamre P, Janson A, Arneborn M, Ekdahl K. SmiNet-2: Description of an internet-based surveillance system for communicable diseases in Sweden. Euro Surveill. 2006;11:103–7.PubMedGoogle Scholar
Figure
Tables
Cite This ArticleTable of Contents – Volume 15, Number 2—February 2009
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Kao-Pin Hwang, Department of Pediatrics, Chang Gung Memorial Hospital—Kaohsiung Medical Center, No.123, Ta-Pei Rd., Niao-Sung Hsiang, Kaohsiung County, 833, Taiwan;
Top