Volume 24, Number 4—April 2018
Research
Avirulent Bacillus anthracis Strain with Molecular Assay Targets as Surrogate for Irradiation-Inactivated Virulent Spores
Abstract
The revelation in May 2015 of the shipment of γ irradiation–inactivated wild-type Bacillus anthracis spore preparations containing a small number of live spores raised concern about the safety and security of these materials. The finding also raised doubts about the validity of the protocols and procedures used to prepare them. Such inactivated reference materials were used as positive controls in assays to detect suspected B. anthracis in samples because live agent cannot be shipped for use in field settings, in improvement of currently deployed detection methods or development of new methods, or for quality assurance and training activities. Hence, risk-mitigated B. anthracis strains are needed to fulfill these requirements. We constructed a genetically inactivated or attenuated strain containing relevant molecular assay targets and tested to compare assay performance using this strain to the historical data obtained using irradiation-inactivated virulent spores.
An effective and constant real-time surveillance capability is crucial for protecting the public from biological threats. Biological threats can be intentional (e.g., resulting from biowarfare or bioterrorism) or unintentional (e.g., resulting from accidental release or emerging infectious diseases) (1,2). Early detection of a biological threat is critical not only for identifying the threat organism but also for implementing appropriate countermeasures to save and protect the victims and prevent further infection and for decontaminating and reclamating the affected environment and infrastructures.
The bedrock of successful biodetection platforms and sensors is use of well-characterized molecular assays, immunoassays, or other types of detection assays. Any assay development effort requires testing, evaluation, and validation of the assays with live or inactivated spiking materials in appropriate matrices relevant to the environments in which the assays are intended to be used (e.g., aerosol collection filters, soils, or clinical matrices). Distribution and use of select agents and toxins are restricted to facilities that have appropriate approval for storage and use of such materials in containment suites and are regulated by the Federal Select Agent Program of the Centers for Disease Control and Prevention (CDC; Atlanta, GA, USA) and the US Department of Agriculture Animal and Plant Health Inspection Service (Riverdale, MD, USA). For other facilities, inactivated select agents, including inactivated spores, historically were the source of reference materials. Many private and academic organizations, government agencies, and foreign government partners have used these materials for various activities, including quality control exercises and medical countermeasure research.
In May 2015, previously shipped irradiation-inactivated B. anthracis spore reference materials were found to contain a small number of live spores (3,4). The incomplete inactivation of the spores raised concern about the safety and security of these materials and doubts about the validity of the protocols and procedures used to prepare them. After this revelation, the US Department of Defense (DoD) and Department of the Army took a series of measures that included review of existing processes and practices to prepare such reference materials (5); placement of a moratorium on shipping of inactivated B. anthracis and other select agents from DoD laboratories until further review (6); formation of an independent entity (BSAT Biorisk Program Office) to oversee all Biologic Select Agents and Toxins (BSAT) activities within DoD; and implementation of various recommendations of different committees established to evaluate BSAT risk mitigation strategies (5,7,8).
Currently, guidance for implementing the Secretary of the Army directive 2016-24 for the DoD BSAT biosafety program (7) has been drafted, with many new measures put in place for the safe handling of BSAT and BSAT-derived products within DoD laboratories and transfer and tracking of such materials across agencies and laboratories. One of the 3 key activities identified in this directive is to explore safer alternatives to BSAT, inactivated BSAT, and BSAT derivatives to reduce health and safety risks associated with BSAT production, handling, and distribution (7).
We describe the construction and characterization of a safer alternative to regulated B. anthracis: a genetically inactivated (rather than irradiation-inactivated) avirulent B. anthracis strain into which specific nucleic acid assay targets for pXO1 and pXO2 replicons have been introduced. The resulting recombinant strain substitutes for and reacts similarly to regulated B. anthracis in molecular testing, whereas currently excluded strains (such as Sterne) lack the pXO2 target (Technical Appendix Figure 1). The resulting recombinant strain can be used for testing PCRs used in many biodefense programs. Also, we demonstrate that these spores can be further inactivated by irradiation so they can be used even in a Biosafety Level (BSL) 1 setting.
Strains, Plasmids, and Primers
Escherichia coli and B. anthracis strains used in this study are listed in Table 1. The plasmids used in various cloning steps and the primers used for amplification, sequence verification, and diagnosis of constructs also are listed in Table 1.
Synthesis of a Recombinant Plasmid Carrying PCR Signatures
We synthesized the recombinant construct 4 cassette, containing 5 different PCR signatures, commercially (Blue Heron, LLC, Bothel, WA, USA) and cloned into pT7Blue (Novagen-MilliporeSigma, St. Louis, MO, USA). The cassette was sequence-verified and PCR-amplified from this plasmid. The PCR product and a lef deletion plasmid pRP1091 (11) were digested with XbaI, ligated, and transformed into TOP10 E. coli cells (Invitrogen). Successful cloning of the insert was confirmed by restriction enzyme digestion, PCR, and sequencing.
Construction of Tagged B. anthracis Sterne Triple Knockout Strain
We conducted transfer and integration of the cloned insert by allelic exchange as described previously (11) (Technical Appendix Figure 2). We designated the final construct recombinant B. anthracis Surrogate with Assay Targets (rBaSwAT-BAP708), hereafter referred to as BAP708.
PCRs
Verification of Toxin Gene Deletions and Presence of Synthetic Cassette
We resuspended single colonies of the strains in 50 μL of PCR-Lyse (Epicentre) or Y-PER (Thermo Fisher Scientific, Waltham, MA, USA), vortexed, and incubated them at 99°C for 15 min. Five μL of each lysate was used as a template for PCR (50 cycles), with 2.5 μL of each 10 μM primer and 0.5 μL of Phusion polymerase (Thermo Fisher Scientific) in 50-μL reactions. Annealing temperatures were 49°C (primers RP214/RP215 [lef] and SS2166/SS2167 [cya]), 54°C (primers SS2168/SS2169 [pagA]), and 59°C (primers SS2164/SS2165 [lef]) (Table 1). Five μL of each PCR product was run on a 0.8% ethidium bromide agarose gel.
Verification of PCR Signature Sequences
We streaked B. anthracis strains on tryptic soy agar plates for isolation and incubated them overnight at 37°C before inoculating a colony from each strain into 15 mL of 3% brain heart infusion and incubating cultures with shaking (100 rpm) for 24 h at 37°C. We then centrifuged the entire culture to pellet the cells (room temperature, 10 min, 2,000 × g) and extracted DNA using the MoBio Ultraclean Microbial DNA Isolation Kit (QIAGEN Inc., Germantown, MD, USA) according to the manufacturer’s recommended protocol; we eluted DNA in a volume of 200 μL. DNA concentration was determined using a NanoDrop (Thermo Fisher Scientific). We diluted extracts such that PCR reactions were performed starting with either 10 or 50 genomic copies. Various B. anthracis–specific PCRs were conducted on an ABI 7500 or 7900 instrument (12).
Animal Study to Evaluate Pathogenicity of the Recombinant Strain
We made spore preparations of various strains using published protocol (13,14). We infected female A/J mice (6–8 weeks old; Charles River, Frederick, MD, USA) subcutaneously with Sterne (34F2) and Sterne derivative spores and checked the mice daily for clinical signs. Animal research at the United States Army Medical Research Institute of Infectious Diseases was conducted under an animal use protocol approved by the Institute’s Institutional Animal Care and Use Committee in compliance with the Animal Welfare Act, Public Health Service Policy, and other federal statutes and regulations relating to animals and experiments involving animals. The facility where this research was conducted is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International and adheres to principles stated in the Guide for the Care and Use of Laboratory Animals (https://grants.nih.gov/grants/olaw/Guide-for-the-Care-and-use-of-laboratory-animals.pdf).
Large-Scale Spore Preparation
We produced BAP708 spores according to the protocol described (Technical Appendix) (15–19), and determined spore counts after heat inactivation to kill any viable vegetative bacteria. We assessed the quality of the spores (particle size and uniformity, diameter, and particle number) using a Coulter counter. In addition, we conducted phase contrast microscopy to examine the uniformity in size of spores and absence of spore clumps. Sporulation efficiency is the ratio of total CFUs before heat inactivation to CFUs after treating the culture at 65°C for 30 min.
Irradiation Inactivation of Spores and Postirradiation Sterility Testing
We irradiated 60 mL of the spores in a JL Shepperd-Model 109–68 Cobalt 60 instrument at a rate of 10,975 rads/min for a total of 456 min, with a final dose of ≈5 × 106 rads (50 KGreys). We tested complete inactivation and loss of viability of the spores using the recently established CDC-recommended protocol for select agent spores (20). We inoculated 6 mL (10%) of the inactivated spore preparation into 60 mL of Terrific broth and incubated at 37°C for 7 d, and plated 1.2 mL (200 μL × 6 plates; i.e., 2% of the culture volume) on Mueller-Hinton agar and incubated for an additional 7 d. No growth was found on any of the plates. We used positive (unirradiated BAP708) and negative (uninoculated broth of the same type and volume under test) controls to ensure the validity of the protocol.
Phage Sensitivity
We tested for phage sensitivity as described using the spot titer method (21). In brief, a bacterial lawn of test strains was prepared using log phase cultures and 10 μL of various dilutions of phages AP50 and γ were spotted on the lawn and incubated overnight at 37°C.
Comparison of Assay Performance of BAP708 Spores to Historical Data from Irradiation-Inactivated Select Agent B. anthracis Spores
We prepared liquid and filter extracted samples according to established protocols using 2 separate aliquots of live and irradiation-inactivated BAP708 spore preparations. We diluted spore stock (≈2.0 × 1010 CFU/mL) in 1× phosphate-buffered saline to a spiking concentration of 2.0 × 106 CFU/mL and either extracted the stock directly as liquid samples or spiked it onto quarter filters, allowed to it dry, and extracted it as filter samples. We used both clean and simulated dirty filters. We extracted samples in accordance with an established single-tube extraction protocol using Amicon Ultra −0.5 Centrifugal filter devices (MilliporeSigma). In brief, we extracted DNA by mechanical disruption using a bead beater (22) and size exclusion filtration and eluted results in a volume of 200 μL. We heat treated DNA extracts to inactivate any nuclease (65°C, 10 min) before use in PCR analysis. We used 5 μL of DNA in 5 different B. anthracis–specific real-time PCRs on the ABI 7500 or ABI 7900 platform (12).
Lateral Flow Immunoassay
We tested live and inactivated spores in a standard lateral flow immunoassay (LFI) that is designed to detect B. anthracis spores (S. Sozhamannan, unpub. data). We used 100 μL of spores in each test and quantified the intensities of test and control lines using a thin layer chromatography scanner and software for scanning LFIs (CAMAG-TLC-3). We plotted results as relative absorbance units versus concentration of spores, set the background threshold at 30 scanner units, and scored all results >30 units as positive. The measurements were done in quadruplicate, and the minimal spore concentration that crossed the threshold was reported as the limit of detection using each spore preparation.
Rationale for Construction of Recombinant Strains with Assay Targets
Mitigating the risk associated with irradiation-inactivated wild-type B. anthracis strains, such as Ames, required use of avirulent, excluded strains as reference materials for detection/diagnostic assay developmental efforts. However, assay targets for virulent strains most often are located in genes that are absent in the excluded strains. B. anthracis detection relies on 3 specific markers, 1 each on the chromosome and the pXO1 and pXO2 replicons. Strains containing plasmid pXO2 are classified as select agents (23), and Sterne lacking pXO2 but carrying pXO1 can be pathogenic for some mice strains because of the presence of the toxin genes (pagA, lef, and cya) on pXO1 (24). Strains lacking either pXO1 or pXO2 lack target(s) for the missing plasmid and hence are of limited utility as reference materials. Therefore, we decided to construct recombinant strains carrying all 3 assay targets in the background of a highly attenuated excluded strain. We chose a Sterne derivative, designated ΔSterne triple knockout strain (BAP417), in which all 3 toxin genes have been deleted (Technical Appendix Table) (11) and that lacks both pXO1 and pXO2 assay targets (Figure 1, panel A), as confirmed by whole-genome sequence analyses (Figure 2). In this strain, assay signatures for pXO1 and pXO2 plasmids were introduced into the ΔpXO1 backbone as described in Materials and Methods.
Synthesis of Assay Target Cassette and Transfer of the Cassette into B. anthracis
Of 4 constructs made, in synthetic construct 4 described here, 5 signatures (PCR targets; i.e., amplicon sequences, including primer and probe sequences) and 2 bar codes were embedded. The bar codes are unique for each construct and can be used to track the strain and distinguish it from the wild type. In addition, stop codons in all 3 open reading frames were placed on the 5′ and 3′ ends of the cassette to prevent any fortuitous translation of the inserts from read-through from neighboring transcriptional signals (Figure 1, panel C).
We conducted transfer of the cassettes onto B. anthracis ΔpXO1 as described previously (11). We determined the characteristics and predicted phenotypic properties of the resulting final scarless construct (Table 2). The deletion-insertion was verified by PCR (Figure 1, panels A,C) and further confirmed by whole-genome sequence analyses (Figure 2).
Characterization of the Recombinant Strain
We conducted a comprehensive phenotypic and genotypic characterization of the recombinant strain, BAP708, to establish its avirulent phenotype and the presence of assay targets for both molecular and immunoassays (Table 3). The characterization included basic microbiological tests, such as colony morphology on selective agar plates; biochemical and phage sensitivity tests; molecular assays, such as PCR; immunoassays, such as LFI; whole-genome sequencing; and animal lethality.
PCR Analyses of Toxin Gene Deletions and Presence of the Cloned Cassettes
We conducted PCRs to confirm the toxin gene deletions and the presence of the cassette in BAP708. We used primers flanking the toxin genes as well as the insertion site (11) to amplify the region. The double (pagA) and triple knockout strains showed the expected deletions, and BAP708 showed an increase in fragment size corresponding to cassette insertion at the expected location (lef) (Figure 1, panels A, B). PCR products of expected sizes were obtained using DNA from the regulated strain B. anthracis Ames, whereas no products were obtained using DNA from B. thuringiensis Al Hakam, indicating absence of the toxin genes. In addition, a real-time PCR designed to distinguish this strain from wild-type virulent strains, such as Ames, detected BAP708 exclusively (data not shown).
Whole-Genome Sequencing and Analysis
We used Illumina next-generation sequencing technology to produce whole-genome sequences of various strains. Whole-genome sequences of the 3 parental strains have been deposited in GenBank under accession nos. BA500-NRIZ00000000, BA482-NRJA00000000, and BA417-NRJB00000000 (27). Analysis of the ΔpXO1 toxin region indicated that the triple knockout strain (BAP417) and its derivative (BAP708) lacked the pagA, lef, and cya genes that encode the 3 anthrax toxin subunits (Figure 2).
Sporulation
The infective form of B. anthracis is the spore, not the vegetative cell. Many detection/diagnostic assays target spore antigens (28). For immunoassays, the antigenic epitopes are most likely spore coat proteins, although there are immunoassays against anthrax toxin, which is produced by vegetative cells and secreted into the extracellular milieu (29). For nucleic acid–based tests, DNA extracted from spores is used as template to detect B. anthracis. Therefore, we assessed the spore-forming ability of BAP708. 34F2 and its derivative BAP708 produced spores efficiently (efficiencies ≈100% [Table 3]). The final titer for the BAP708 spore preparation was ≈1.5 × 1010 spores/mL, and the particle size was 1.153 ± 0.122 μm. Sporulation results for regulated B. anthracis Ames strain and the negative control B. thuringiensis Al Hakam strain have been published and were normal (16,25).
Phage Sensitivity
One diagnostic test recommended by CDC for the suspected presence of B. anthracis in a sample is sensitivity of the bacterial isolate from the sample to γ phage. AP50c is another phage that can be used to verify B. anthracis (30). The recombinant strain, BAP708, exhibited sensitivity to both phages, as did the parent strains (Table 3), although they were less sensitive than other strains, such as Sterne 7702 (data not shown). In addition, bacteria in log phase were much more sensitive to infection by AP50c than were stationary phase cells (data not shown), which may be due to phase-dependent expression of the AP50c phage receptor, Sap (31,32). Regulated B. anthracis Ames strain was sensitive to both phages, and the negative control B. thuringiensis Al Hakam strain was resistant to both phages.
Molecular Assays
We assessed the performance of BAP708 in molecular assays (Table 4). Real-time PCRs using BAP708 and B. anthracis Ames produced expected results in accordance with the assay targets present or introduced into the strain, whereas assays using the negative control B. thuringiensis Al Hakam strain did not produce a positive amplification.
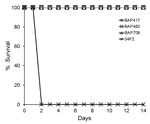
Validation of Avirulent Nature of Recombinant Strain
We inoculated female A/J mice (6–8 weeks old) subcutaneously with spores of Sterne (34F2) or its derivative. The 50% lethal dose (LD50) in this model is 1.1 × 103 B. anthracis Sterne (pXO1+/pXO2−) spores (33), and the LD50 of fully virulent strains, such as Ames, and other species of Bacillus, such as B. cereus G9241, have been reported (26,33,34). The calculated delivered LD50 equivalents are as follows: BAP417, 109.7; BAP482, 152.7; BAP708, 106.1; and 34F2, 164.8. The animals were monitored daily for clinical signs for up to 14 days. Only the mice challenged with 34F2 showed any signs of disease; these mice succumbed to the infection or were euthanized after meeting early-endpoint criteria within 48 h (Figure 3). All animals in the other groups showed no signs of disease, indicating the avirulent nature of the toxin gene deletion derivatives.
Comparisons of Assay Performance of Recombinant Strain to Wild-Type and Inactivated Wild-Type Spores
We tested live and inactivated BAP708 spores for performance in immunoassays and PCRs to evaluate the effect of irradiation on assay targets. Unlike the near neighbor B. thuringiensis Al Hakam, BAP708 spores reacted positively in LFI, albeit weakly compared with historical reference materials, such as inactivated B. anthracis Ames (data not shown). PCR was done on DNA extracted in 2 different formats: liquid and spiked filter. All extracts reacted as expected in PCRs. These results were comparable to historical data obtained using irradiation-inactivated Ames spores. The inactivated B. thuringiensis Al Hakam spores treated and extracted similarly did not yield any positive results (Table 4).
There are multiple instances of poor biosafety/biosecurity measures or laboratory accidents resulting in the release of harmful pathogens (4,35–37). These incidents underscore the lack of knowledge about factors influencing environmental survival of biological agents, the steps needed to ensure that established biosafety methods continue to work and meet expectations, and the need to acquire knowledge about how to recognize early any failure in established laboratory methods over time (1). We demonstrated an alternate approach that can potentially minimize risks associated with using BSATs and perhaps eliminate their use in some applications.
The need for BSATs and their derivatives for research and countermeasure development is inevitable. Guaranteeing inactivation of BSATs, especially spores, without adversely affecting their diagnostic and therapeutic targets can be problematic. However, the strategy described here of genetically inactivating the organism to mitigate the risk is a safer approach. In this study, we chose a B. anthracis strain that carries one of the virulence plasmids (pXO1) and removed the toxin genes from that plasmid to make it completely avirulent. Another option would have been to introduce pXO1 and pXO2 assay targets into the chromosome in a pXO1− and pXO2− background. However, the copy numbers of pXO1 and pXO2 have been determined to be slightly higher than that of the chromosome (1, 2, and 4 copies for the chromosome, pXO2, and pXO1 respectively) (38). To maintain a slightly higher copy number of the introduced plasmid assay targets, we introduced the assay targets into the ΔpXO1 backbone rather than into the chromosome in a strain lacking both pXO1 and pXO2. This way, assay results would be comparable in terms of copy numbers and cycle threshold values to historical assay data produced from a strain such as Ames.
In introducing the assay targets, neither full-length genes nor any antibacterial drug marker were introduced. Moreover, the surrogate strain is similar to virulent B. anthracis with respect to its utility as a reference material, except that it is risk-mitigated. In addition, unique bar codes have been introduced to distinguish the surrogate from the wild-type virulent agent and for forensic purposes.
The approach we describe can be easily adapted for other assay targets and applications. For example, genes encoding vaccine antigens, such as nonlethal variants of toxin genes, could be cloned and expressed in the recombinant strain. Because it is a platform technology, it would be relatively easy to construct strains for other assays by exchanging assay targets, which would also be safer and more cost-effective than handling BSATs and their derivatives. Noninfectious virus-like particles carrying assay targets could be created for BSL3 and BSL4 viral agents (39,40). The major disadvantage to this approach is that for every new assay signature/target, a new strain needs to be constructed, which may entail initial investment of time and funds to create the framework. Another disadvantage is that not all applications can be fulfilled by any 1 strain.
BSATs and inactivated BSATs pose risk and cost with respect to safety and security in production, validation, and shipping. Genetically inactivated and modified organisms provide almost the same level of assay capabilities as BSAT agents but with greatly reduced risk and cost. In addition, the recombinant construct described here is excluded from any regulatory concerns, such as need for exclusion from CDC select agent experiments, recombinant DNA advisory committee guidelines, or International Biological Weapons Convention regulations. Therefore, development of risk-mitigated solutions, such as the one we describe, can help minimize and perhaps prevent mishaps, such as the incident that came to light in 2015.
Dr. Plaut is a staff scientist at the Food and Drug Administration in Silver Spring, Maryland. His research interests include genetic regulation of virulence mechanisms of bacterial pathogens, such as Staphylococcus aureus and Bacillus anthracis, and development of allelic exchange systems for gram-positive bacteria.
Acknowledgments
We thank Amanda Horstman-Smith for many useful comments that improved the manuscript immensely, Carcie Graves for performing the LFI, and Tara Harvey and Jody Gostomski for help with PCRs.
The work was supported by funds from the Joint Program Executive Office for Chemical and Biological Defense.
References
- Lieberman J, Ridge T, Shalala D, Daschle T, Greenwood J, Wainstein K. Blue Ribbon Study Panel on Biodefense Report: a national blueprint for biodefense: leadership and major reform needed to optimize efforts [cited 2015 Oct 28]. http://potomacinstitute.org/featured-news/1819-biodefense-blueprint-2
- Imperiale MJ, Casadevall A. Bioterrorism: lessons learned since the anthrax mailings. MBio. 2011;2:e00232–11. DOIPubMedGoogle Scholar
- Sozhamannan S, Smith M, Setlow P, Hanna PC. On the origin of live spores in gamma irradiated spore preparations a perfect example of Poisson distribution. ASM Microbe. 2016 Jan:4–5.
- US Department of Defense. DoD launches review of lab procedures involving anthrax [cited 2015 May 29]. https://www.defense.gov/News/Article/Article/604749
- US Department of Defense. Committee for Comprehensive Review of DoD Laboratory Procedures, Processes, and Protocols Associated with Inactivating Bacillus anthracis Spores. Review committee report: inadvertent shipment of live Bacillus anthracis spores by DoD [cited 2017 Aug 26]. https://www.defense.gov/Portals/1/features/2015/0615_lab-stats/Review-Committee-Report-Final.pdf
- Secretary of the Army. Memorandum: immediate safety review and extension of moratorium. 2015 Sep 2 [cited 2017 Aug 26]. https://www.defense.gov/Portals/1/Documents/BSAT_Safety_Review_directive.pdf
- Secretary of the Army. Memorandum: Army Directive 2016-24 (Department of Defense Biological Select Agent and Toxins Biosafety Program). 2016 Jul 25 [cited 2017 Aug 26]. http://armypubs.army.mil/epubs/DR_pubs/DR_a/pdf/web/Army%20Directive%202016-24%20Final.pdf
- Deputy Secretary of Defense. Implementation of the recommendations in the comprehensive review report: inadvertent shipment of live Bacillus anthracis (anthrax) spores by Department of Defense. 2015 Jul 23 [cited 2017 Aug 26]. https://www.defense.gov/Portals/1/features/2015/0615_lab-stats/docs/DSD-Memo-Implementation-of-Recommendations-in-Comprehensive-Review-Report.pdf
- Simon R, Priefer U, Puhler A. A broad host range mobilization system for in vivo genetic-engineering: transposon mutagenesis in gram-negative bacteria. Nat Biotechnol. 1983;1:784–91. DOIGoogle Scholar
- Stibitz S, Carbonetti NH. Hfr mapping of mutations in Bordetella pertussis that define a genetic locus involved in virulence gene regulation. J Bacteriol. 1994;176:7260–6. DOIPubMedGoogle Scholar
- Plaut RD, Stibitz S. Improvements to a markerless allelic exchange system for Bacillus anthracis. PLoS One. 2015;10:e0142758. DOIPubMedGoogle Scholar
- Hoffmaster AR, Meyer RF, Bowen MD, Marston CK, Weyant RS, Thurman K, et al. Evaluation and validation of a real-time polymerase chain reaction assay for rapid identification of Bacillus anthracis. Emerg Infect Dis. 2002;8:1178–82. DOIPubMedGoogle Scholar
- Nicholson W, Setlow P. Molecular biological methods for Bacillus. New York: John Wiley; 1990.
- Thomas D, Naughton J, Cote C, Welkos S, Manchester M, Young JA. Delayed toxicity associated with soluble anthrax toxin receptor decoy-Ig fusion protein treatment. PLoS One. 2012;7:e34611. DOIPubMedGoogle Scholar
- Atrih A, Foster SJ. Analysis of the role of bacterial endospore cortex structure in resistance properties and demonstration of its conservation amongst species. J Appl Microbiol. 2001;91:364–72. DOIPubMedGoogle Scholar
- Buhr TL, Young AA, Minter ZA, Wells CM, McPherson DC, Hooban CL, et al. Test method development to evaluate hot, humid air decontamination of materials contaminated with Bacillus anthracis ∆Sterne and B. thuringiensis Al Hakam spores. J Appl Microbiol. 2012;113:1037–51. DOIPubMedGoogle Scholar
- Gladstone GP, Fildes P. A simple culture medium for general use without meat extract or peptone. Br J Exp Pathol. 1940;21:161–73.
- Camp DW, Montgomery NK. How good labs can get wrong results—keys to accurate and reproducible quantitation of Bacillus anthracis spore sampling or extraction efficiency. Presented at: Third National Conference on Environmental Sampling and Detection for Biol-Threat Agents. Las Vegas, NV, USA; 2008 Dec 2–4.
- Buhr TL, Wells CM, Young AA, Minter ZA, Johnson CA, Payne AN, et al. Decontamination of materials contaminated with Bacillus anthracis and Bacillus thuringiensis Al Hakam spores using PES-Solid, a solid source of peracetic acid. J Appl Microbiol. 2013;115:398–408. DOIPubMedGoogle Scholar
- Federal Select Agent Program. Revised FSAP policy statement: inactivated Bacillus anthracis and Bacillus cereus biovar anthracis. August 14, 2017 [cited 2017 Aug 26]. https://www.selectagents.gov/policystatement_bacillus.html
- Bishop-Lilly KA, Plaut RD, Chen PE, Akmal A, Willner KM, Butani A, et al. Whole genome sequencing of phage resistant Bacillus anthracis mutants reveals an essential role for cell surface anchoring protein CsaB in phage AP50c adsorption. Virol J. 2012;9:246. DOIPubMedGoogle Scholar
- BSP- Biol Spec products. Mini-Bead Beater-8- Preparation of sample [cited 2017 Nov 21]. https://biospec.com/instructions/minibeadbeater_8
- Centers for Disease Control and Prevention. Federal Select Agent Program: select agents and toxins list. 2017 [cited 2017 Aug 24]. https://www.selectagents.gov/SelectAgentsandToxinsList.html
- Loving CL, Khurana T, Osorio M, Lee GM, Kelly VK, Stibitz S, et al. Role of anthrax toxins in dissemination, disease progression, and induction of protective adaptive immunity in the mouse aerosol challenge model. Infect Immun. 2009;77:255–65. DOIPubMedGoogle Scholar
- Buhr TL, Young AA, Minter ZA, Wells CM, Shegogue DA. Decontamination of a hard surface contaminated with Bacillus anthracisΔSterne and B. anthracis Ames spores using electrochemically generated liquid-phase chlorine dioxide (eClO2). J Appl Microbiol. 2011;111:1057–64. DOIPubMedGoogle Scholar
- Lyons CR, Lovchik J, Hutt J, Lipscomb MF, Wang E, Heninger S, et al. Murine model of pulmonary anthrax: kinetics of dissemination, histopathology, and mouse strain susceptibility. Infect Immun. 2004;72:4801–9. DOIPubMedGoogle Scholar
- Staab A, Plaut RD, Pratt C, Lovett SP, Wiley MR, Biggs TD, et al. Whole-genome sequences of variants of Bacillus anthracis Sterne and their toxin gene deletion mutants. Genome Announc. 2017;5:e01231–17. DOIPubMedGoogle Scholar
- Waller DF, Hew BE, Holdaway C, Jen M, Peckham GD. Rapid detection of Bacillus anthracis spores using immunomagnetic separation and amperometry. Biosensors (Basel). 2016;6:E61. DOIPubMedGoogle Scholar
- Biagini RE, Sammons DL, Smith JP, MacKenzie BA, Striley CA, Snawder JE, et al. Rapid, sensitive, and specific lateral-flow immunochromatographic device to measure anti-anthrax protective antigen immunoglobulin g in serum and whole blood. Clin Vaccine Immunol. 2006;13:541–6. DOIPubMedGoogle Scholar
- Sozhamannan S, McKinstry M, Lentz SM, Jalasvuori M, McAfee F, Smith A, et al. Molecular characterization of a variant of Bacillus anthracis-specific phage AP50 with improved bacteriolytic activity. Appl Environ Microbiol. 2008;74:6792–6. DOIPubMedGoogle Scholar
- Mignot T, Mesnage S, Couture-Tosi E, Mock M, Fouet A. Developmental switch of S-layer protein synthesis in Bacillus anthracis. Mol Microbiol. 2002;43:1615–27. DOIPubMedGoogle Scholar
- Plaut RD, Beaber JW, Zemansky J, Kaur AP, George M, Biswas B, et al. Genetic evidence for the involvement of the S-layer protein gene sap and the sporulation genes spo0A, spo0B, and spo0F in Phage AP50c infection of Bacillus anthracis. J Bacteriol. 2014;196:1143–54. DOIPubMedGoogle Scholar
- Welkos SL, Keener TJ, Gibbs PH. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect Immun. 1986;51:795–800.PubMedGoogle Scholar
- Wilson MK, Vergis JM, Alem F, Palmer JR, Keane-Myers AM, Brahmbhatt TN, et al. Bacillus cereus G9241 makes anthrax toxin and capsule like highly virulent B. anthracis Ames but behaves like attenuated toxigenic nonencapsulated B. anthracis Sterne in rabbits and mice. Infect Immun. 2011;79:3012–9. DOIPubMedGoogle Scholar
- Meselson M, Guillemin J, Hugh-Jones M, Langmuir A, Popova I, Shelokov A, et al. The Sverdlovsk anthrax outbreak of 1979. Science. 1994;266:1202–8. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Conclusion of select agent inquiry into Burkholderia pseudomallei release at Tulane National Primate Research Center. 2015 Mar 13 [cited 2017 Aug 26]. http://www.cdc.gov/media/releases/2015/s0313-burkholderia-pseudomallei.html
- US Department of Justice. Amerithrax investigative summary. 2010 Feb 19 [cited 2017 Aug 26]. www.justice.gov/amerithrax/docs/amx-investigative-summary.pdf
- Straub T, Baird C, Bartholomew RA, Colburn H, Seiner D, Victry K, et al. Estimated copy number of Bacillus anthracis plasmids pXO1 and pXO2 using digital PCR. J Microbiol Methods. 2013;92:9–10. DOIPubMedGoogle Scholar
- Noda T, Sagara H, Suzuki E, Takada A, Kida H, Kawaoka Y. Ebola virus VP40 drives the formation of virus-like filamentous particles along with GP. J Virol. 2002;76:4855–65. DOIPubMedGoogle Scholar
- Warfield KL, Swenson DL, Demmin G, Bavari S. Filovirus-like particles as vaccines and discovery tools. Expert Rev Vaccines. 2005;4:429–40. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleTable of Contents – Volume 24, Number 4—April 2018
| EID Search Options |
|---|
|
|
|
|
|
|


Please use the form below to submit correspondence to the authors or contact them at the following address:
Shanmuga Sozhamannan, The Tauri Group Supporting Defense Biological Product Assurance Office JPM Guardian, 110 Thomas Johnson Dr, Ste 250, Frederick, MD 21702, USA
Top