Volume 5, Number 2—April 1999
Perspective
International Editors:Emerging Infectious Diseases—United Kingdom
This review describes some of the most important new or reemerging infectious diseases in the United Kingdom in the past decade. Most of the statistics relate to England and Wales, where the surveillance system is operated by the Public Health Laboratory Service (PHLS), through its Communicable Disease Surveillance Centre (CDSC). The statistics come from three main sources and several more specialized ones. The most important is the laboratory-based surveillance system, started more than 50 years ago, to which the national network of 48 public health laboratories and the specialized reference microbiology laboratories of PHLS and more than 150 National Health Service laboratories contribute regularly. Most data collection is performed electronically, through a computerized system that allows laboratory data to be captured at the source, augmented with clinical or risk factor data, and transmitted both centrally to CDSC and locally to the responsible public health professionals. CDSC also runs, on behalf of the Office of National Statistics, the long-established statutory notification system, which is based on clinical reporting of a schedule of infectious and communicable diseases including food poisoning. The third system is a sentinel system based on general practice run by the Royal College of General Practitioners Research Unit. These three systems complement each other, and the data are collated, analyzed, and disseminated by CDSC and are then extensively used to inform both government policies and local activities for the prevention and control of communicable disease.
In addition to the "big three," the United Kingdom has several other more specific surveillance systems, in particular, confidential clinical reporting systems for AIDS and sexually transmitted diseases and serosurveillance (including unlinked anonymous) systems for HIV infection. In addition, active surveillance systems, developed jointly by PHLS and the relevant professional associations, capture clinical case reports of rare diseases, such as pediatric AIDS and Reye syndrome. These active systems are particularly suited to the surveillance of rare and emerging diseases, such as pediatric Creutzfeldt-Jakob (CJD) disease.
A growing number of disease-specific surveillance systems, operated on a Europe-wide basis, are increasingly attracting other international participants. CDSC coordinates Enter-Net, a Europe-wide scheme for surveillance of salmonella and Escherichia coli O157. This network, which comprises epidemiologists and reference microbiologists from each member state of the European Union plus Switzerland and Norway, has led to the successful detection and investigation of several international foodborne outbreaks. A similar network coordinated by CDSC exists for travel-associated Legionnaires' disease. A mainly European-based surveillance network for meningococcal disease is also working well.
One of the side-effects of an efficient surveillance system is that because new diseases or variants of diseases and outbreaks are detected earlier than in countries with less comprehensive systems, such diseases are often thought to have originated, or to predominate, in that country. This happened, for example, with Salmonella Enteritidis contamination of hens' eggs, which was, as it later became apparent, not confined to the United Kingdom but was widespread throughout Europe. However, one emerging disease that did have its origins in the United Kingdom is new variant (nv) CJD.
A previously undescribed encephalopathy in cows, bovine spongiform encephalopathy, with characteristic clinical and histologic features, was first identified in November 1986, although the first case may have occurred as early as April 1985. Since then, the number of cases reported in the United Kingdom has exceeded 166,000. However, the epidemic reached a peak in 1992–93. The number of cases recorded has been diminishing since, and the cattle epidemic, linked to the consumption of contaminated ruminant-derived meat and bone meal, is predicted to be over by 2001 (1). (The method of rendering protein changed shortly before the disease first appeared in cows.) Surveillance of CJD in humans began in 1990, when the National CJD Surveillance Unit was established in Edinburgh, Scotland.
The first human cases of nvCJD appeared in 1995, with onset dates from February 1994 (2) (Table). NvCJD was distinguished from classic CJD on clinical and histologic grounds and by the patients' young age. Although evidence is mounting that nvCJD is the human form of bovine spongiform encephalopathy (3,4), no direct association has yet been established between the development of nvCJD and the consumption of beef.
An estimated 25,000 persons in the United Kingdom are infected with HIV, an overall prevalence of approximately 45 per 100,000 population (5). At least 15,000 are receiving care. Disease prevalence varies considerably by geographic area, with most cases in London and the southeast of England. National prevalence is lower than in all but four countries of Western Europe. As in most countries of Northern Europe, sex between mens remains the predominant mode of HIV transmission. In the United Kingdom, heterosexually acquired cases are the second largest risk group. Most such infections are in persons from, or who have lived in, sub-Saharan Africa. Some heterosexually acquired cases originate in other higher prevalence areas of the world, as well as from within the United Kingdom, but numbers are currently fairly small. Apart from cities in Scotland, where outbreaks occurred in the mid-1980s, continuing HIV transmission among injecting drug users appears low. Needle exchange programs, which have contributed to limiting spread, have been in place in most urban areas of the United Kingdom since the late 1980s. In this country, HIV infection in pregnant women is still not adequately recognized, and thus steps to greatly reduce the chance of transmission of infection from mother to baby have not yet been taken. Recent guidance from the Department of Health concerning the need for HIV screening in pregnancy is intended to address this problem.
In spite of considerable efforts to reduce the spread of HIV in the United Kingdom, the number of newly diagnosed cases of HIV infection has been fairly constant in the 1990s. The rates among male homosexual attendees younger than 25 years of age at sexually transmitted disease clinics have shown no signs of decreasing, suggesting continued appreciable HIV incidence in men who have sex with men. Furthermore, the rates of acute sexually transmitted infections (markers of unsafe sex) in homosexual men have increased again after a decline in the mid-1980s.
The incidence of AIDS (but not the incidence of HIV infections) and the number of deaths have fallen dramatically in the last 2 years as a result of the introduction of highly active antiretroviral therapies. This decrease has been most marked in men who have acquired HIV through sex with men. A consequence of the falling death rate, with sustained rates of new diagnoses, is increasing prevalence of HIV infection.
After many years, tuberculosis is reemerging in this country as in many other countries of the world (6). In England and Wales the annual number of cases had been declining for over 150 years, reaching its lowest point of 5,085 reported cases (10.1 per 100,000 population) in 1987. Since then, the number of cases has remained at a plateau of 5,000 to 6,000 cases per year. However, increases were recorded in 3 recent consecutive years, 1995-1997. Moreover, within these bare statistics, there are some disturbing trends. Rates in certain ethnic groups have increased significantly, while those in Caucasians have continued to fall. Cases of tuberculosis in persons of black African origin accounted for 1% of all cases in 1988, and account for more than 10% now. Multidrug-resistant tuberculosis remains at a low level, although nosocomial transmission has been reported. An enhanced surveillance system and new technology for rapid resistance testing have been put in place.
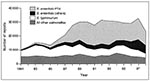
Extremely rare a decade ago, E. coli O157 infection is emerging as an important public health problem in the United Kingdom because of the severity of the illness it causes, even though the annual number of reported infections remains comparatively low (approximately 1,000). Undoubtedly the most important outbreak of E. coli O157 in the United Kingdom originated in a butcher's shop in Lanarkshire, Scotland, in November and December 1996 (7). Approximately 85 outlets in central Scotland stocked the butcher's products, which made the task of outbreak management and control extremely difficult. The date of onset of the first known case was November 15 and of the last confirmed case December 15. The number of cases escalated rapidly from November 15 and at the peak of the outbreak, November 25, reached more than 40 cases (Figure 1) in 1 day; 496 persons were affected, and 18 persons died. One of the features of the outbreak was the occurrence of several separate incidents, the largest of which was a birthday party for 100 persons in a church hall. All isolates of E. coli O157 belonged to phage type 25 and contained the verocytotoxin gene VT2. Pulsed-field gel electrophoresis showed that all 262 strains tested were indistinguishable. A group was convened by the Scottish Office to consider the circumstances that led to the outbreak and the implications for food safety. Among the many recommendations was the accelerated introduction of the Hazard Analysis/Critical Control Point (HACCP) system (8) for high-risk premises and the selective licensing of food premises.
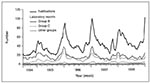
Although hardly an emerging disease, salmonella food poisoning has reemerged both in incidence and in importance in recent years (Figure 2). Much of this increase is attributable to S. Enteritidis, which has accounted for approximately 70% of all salmonella infections in recent years, with S. Enteritidis phage type 4 accounting for 45% of the total. These strains are closely associated with eggs and poultry. In addition, multidrug-resistant S. Typhimurium DT 104 has emerged as an important cause of food-poisoning outbreaks. In 1997, the highest number of salmonella infections was recorded (32,596), but in 1998 only 23,216 cases (provisional) were reported, a fall of about 30%. It is too soon to say if this decrease will be sustained and if it can be attributed to control measures. Campylobacter infections are the major cause of laboratory-confirmed bacterial gastrointestinal infections, while small-round structured viruses now account for more than 40% of reported pathogens associated with general outbreaks of infectious intestinal disease in England and Wales (9).
Cryptosporidium has emerged as a cause of waterborne outbreaks since the 1980s. The problem was considered serious enough for the government to convene an expert group, which reported in 1990. An outbreak in the north Thames area of England in 1997 had 345 confirmed cases and probably many others, and 746,000 persons were advised to boil water before consumption (10). This outbreak resulted from contamination of a filtered borehole-derived public water supply. A period of heavy rainfall following the driest spell for at least 200 years may have contributed. Cryptosporidial oocysts need to be filtered out of water as they are not affected by normal concentrations of chlorine, and the oocyst load was probably too great for the filters at various times during this unusual weather spell. This was the first reported cryptosporidiosis outbreak in the United Kingdom caused by filtered borehole water and the third involving groundwater supplies. It also resulted in the reconvening of the expert group by the government. Mandatory continuous sampling for Cryptosporidium in supplies at risk is under consideration (11).
In an important advance, PHLS researchers have recently demonstrated the existence of at least two genotypes of C. parvum. Evidence so far (12) suggests that whereas human infections are associated with both genotypes, livestock animal infections are associated with one genotype only. If confirmed, these preliminary findings should make an important contribution to elucidating the epidemiology of this still-emerging infection.
Meningococcal infection has produced a sustained and somewhat baffling rise in incidence in the 1990s (Figure 3), with an even greater-than-expected increase in the first few weeks of 1999. Although serogroup B disease continues to predominate, the epidemiology is changing; the proportion of infections caused by serogroup C is increasing, and these infections show an increasing tendency to cause clusters and outbreaks in teenagers and young adults. Conjugated vaccines against serogroup C are under evaluation in the United Kingdom by PHLS and others.
In recent years, the public health importance of C. trachomatis infection has been increasingly recognized. Reported rates of infection exceed 100 per 1,000,000 population in those ages 15 to 59 years, making it the most common bacterial cause of sexually transmitted disease. It is estimated that only 10% of cases are identified. Chlamydia is an important cause of pelvic inflammatory disease and infertility in untreated women. Targeted screening in groups at high risk is under consideration.
On average, 3,000 new cases and 1,000 late cases of syphilis are reported each year in England and Wales. Approximately half of the laboratory-confirmed cases appear to be indigenous infections; the remainder are acquired abroad (13). A recent increase in infections contracted in Russia has been noted. However, a large, prolonged outbreak of indigenous syphilis occurred in Bristol in England between January 1997 and May 1998. Forty-five persons were infectedthe expected number was one or two cases only. This was a heterosexually transmitted outbreak, and, unusually, women outnumbered men by 26 to 19. An urgent coordinated public health response identified many cases, but a number of sexual contacts were untraceable, and the potential for ongoing transmission remains (14).
Very few confirmed cases of infection with toxigenic Corynebacterium diphtheriae are reported in the United Kingdom associated with travel to disease-endemic areas. However, in recent years, cases of nontoxigenic C. diphtheriae var gravis have emerged. In the wider European context, diphtheria has reemerged as a major public health problem in the countries of the former Soviet Union.
Levels of antimicrobial resistance, although lower than in many other countries in Europe and elsewhere, are an increasing cause for concern. For example, the numbers and geographic distribution of reported bloodstream infections with methicillin-resistant Staphylococcus aureus have escalated. Almost 32% of staphylococcal septicemias in 1997 were caused by methicillin-resistant S. aureus, compared with only 2% in 1992. Antimicrobial resistance has been the subject of two recent national reports (15,16), and a comprehensive strategy is being developed to address the problem (17).
"For the community as a whole, hepatitis C is a viral time-bomb which is slowly destroying the health of large numbers of the world population" (18). In England and Wales, only 57% of reported patients have known risk factors. Of these, approximately 80% identified injecting drug use as the main route of transmission, and 2.9% reported sexual exposure. Blood or blood product recipients accounted for 7.2% of the cohort of cases diagnosed between 1992 and 1996; this proportion is rapidly diminishing (19) as a result of the screening of blood donors and the use of treated blood products.
Surveillance of influenza in England and Wales has reached a high level of sophistication, with many sources of data now available, covering clinical reports, reports of deaths from several different respiratory conditions, and virus isolation and subtyping reports (20). In 1998, in the face of concern that influenza might be reemerging because of the occurrence in Hong Kong of 18 cases of infection (with 6 deaths) from a new influenza subtype of avian origin, A(H5N1), PHLS activated the first phase of its pandemic influenza plan. The chicken-related strain proved poorly transmissible to humans, but the episode provided a useful practice run for the contingency plan.
Given the existence of an effective vaccine against measles, mumps, and rubella and a comprehensive immunization program, there might seem little prospect of measles emerging once again as a serious public health problem in the United Kingdom. However, vaccine coverage has fallen recently, coinciding with adverse publicity over an alleged link between the vaccine and both Crohn disease and autism (21). This illustrates the ever-present potential for infections, even those close to elimination, to regain the upper hand if preventive measures are disrupted.
References
- Maxwell RJ. An unplayable hand? BSE, CJD and the British Government. London: King's Fund Publishing; 1997.
- Will RG, Ironside JW, Zeidler M, Cousens SN, Estibeiro K, Alperovitch A, A new variant of Creutzfeldt-Jakob disease in the UK. Lancet. 1996;347:921–5. DOIPubMedGoogle Scholar
- Hill AF, Desbruslais M, Joiner S, Sidle KCL, Gowland I, Collinge J. The same prion strain causes vCJD and BSE. Nature. 1997;389:448–50. DOIPubMedGoogle Scholar
- Bruce ME, Will RG, Ironside JW, McConnell I, Drummon D, Suttie A, Transmissions to mice indicate that "new variant" CJD is caused by the BSE agent. Nature. 1997;389:489–501. DOIPubMedGoogle Scholar
- Communicable Disease Surveillance Centre. The global HIV epidemic. Commun Dis Rep CDR Wkly. 1998;8:227.
- Communicable Disease Surveillance Centre. Tuberculosis remains "the captain of all these men of death.". Commun Dis Rep CDR Rev. 1997;7:R105–l6.PubMedGoogle Scholar
- The Pennington Group. Report on the circumstances leading to the 1996 outbreak of infection with E. coli O157 in Central Scotland, the implications for food safety and the lessons to be learned. Edinburgh: The Stationery Office; 1997.
- FAO/WHO. Introducing the Hazard Analysis Critical Control Point system. Geneva: The Organization; 1997. Report: WHO/FSF/FOS/97.2.
- Evans HS, Madden P, Douglas C, Adak GK, O'Brien SJ, Djuretic T, General outbreaks of infectious gastrointestinal disease in Scotland and Wales: 1995 and 1996. Commun Dis Public Health. 1998;1:165–71.PubMedGoogle Scholar
- Willcocks L, Crampin A, Milne L, Seng C, Susman M, Gair R, A large outbreak of cryptosporidiosis associated with a public water supply from a deep chalk borehole. Commun Dis Public Health. 1998;1:239–43.PubMedGoogle Scholar
- Casemore D. Cryptosporidium and the safety of our water supplies. Commun Dis Public Health. 1998;1:218–9.PubMedGoogle Scholar
- Patel S, Pedraza-Diaz S, McLauchlin J, Casemore D. Molecular characterisation of Cryptosporidium parvum from two large suspected waterborne outbreaks. Commun Dis Public Health. 1998;1:231–3.PubMedGoogle Scholar
- Ratcliffe L, Nicoll A, Carrington D, Wong H, Egglestone SI, Lightfoot NF, Reference Laboratory Surveillance of syphilis in England and Wales, 1994 to 1996. Commun Dis Public Health. 1998;1:14–21.PubMedGoogle Scholar
- Communicable Disease Surveillance Centre. Syphilis in Bristol 1997-8: an update. Commun Dis Rep CDR Wkly. 1998;8:413.PubMedGoogle Scholar
- House of Lords Select Committee on Science and Technology. Resistance to antibiotics and other antimicrobials. Session l997-98,7th report. London: The Stationery Office; 1998.
- Standing Medical Advisory Committee Sub-Group on Antimicrobial Resistance. The path of least resistance. Department of Health, 1998.
- Government response to the House of Lords Select Committee on Science and Technology Report: Resistance to antibiotics and other antimicrobial agents. London: The Stationery Office; 1998.
- English R, Foster G. Living with hepatitis C. London: Robinson; 1997.
- Ramsay ME, Balogun MA, Collins M, Balraj V. Laboratory surveillance of hepatitis C virus infection in England and Wales: 1992 to 1996. Commun Dis Public Health. 1998;1:89–94.PubMedGoogle Scholar
- Dedman DJ, Zambon M, Van Buynder P, Fleming DM, Watson JM, Joseph CA. Influenza surveillance in England and Wales: October 1997 to June 1998. Commun Dis Public Health. 1998;1:244–51.PubMedGoogle Scholar
- Communicable Disease Surveillance Centre. MMR vaccine coverage falls after adverse publicity. Commun Dis Rep CDR Wkly. 1998;8:41.PubMedGoogle Scholar
Figures
Table
Cite This ArticleTable of Contents – Volume 5, Number 2—April 1999
| EID Search Options |
|---|
|
|
|
|
|
|