Mexico
CDC Yellow Book 2024
Popular ItinerariesDestination Overview
Mexico, the second most populous country in Latin America (population >120 million), is the country most often visited by US tourists. Many US residents, particularly in the border region, frequent Mexico to visit friends and relatives, contributing to the nearly 200 million US–Mexico land border crossings annually. The capital, Mexico City, is one of the world’s largest cities (population >20 million) and is a popular destination for business and mass gathering events.
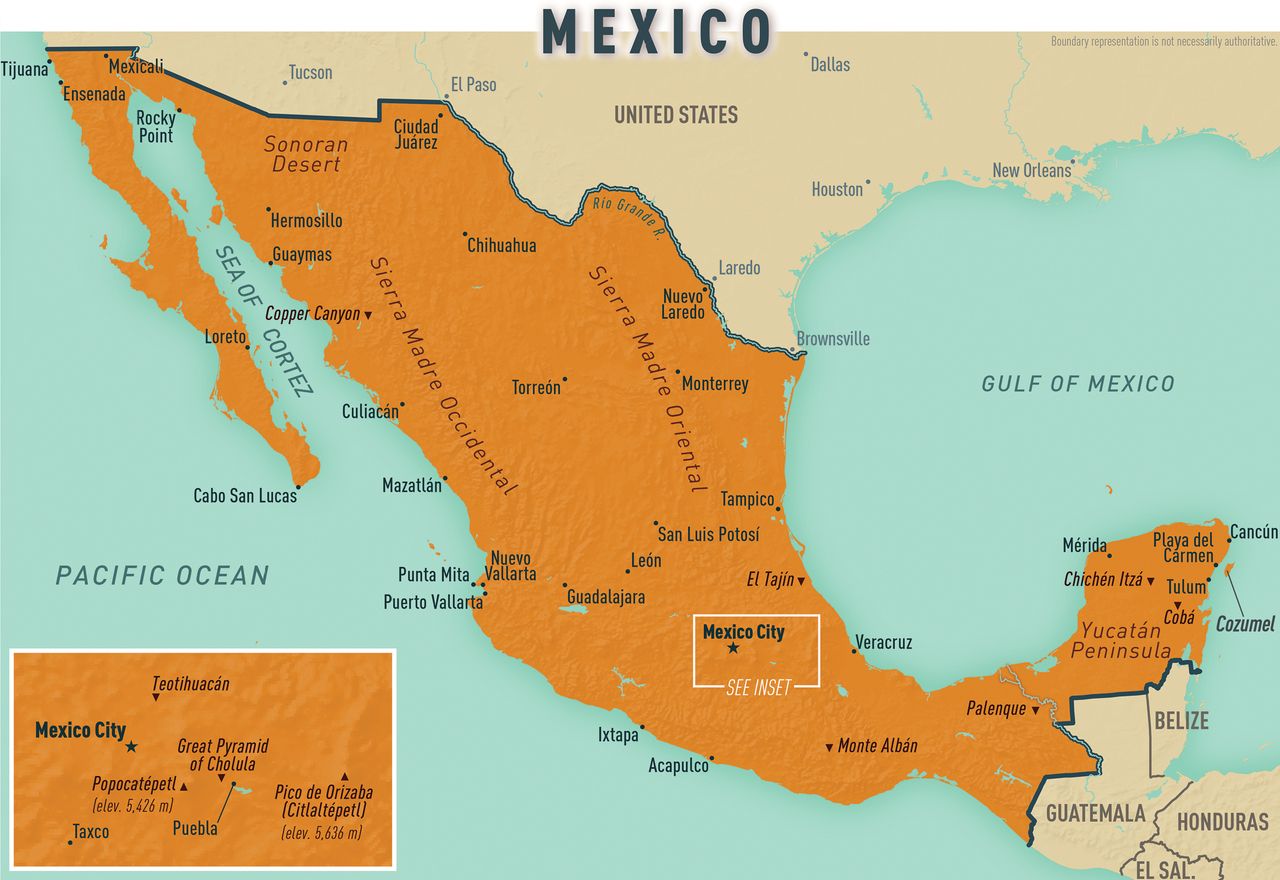
Mexico’s diverse geography throughout its 32 states attracts travelers for nature, recreation, and sport (Map 10-09). The country’s rich history, diverse cuisine, and proud culture reflects its pre-Columbian and Hispanic past. In the past decade, travelers to Mexico have increasingly sought health and wellness services throughout the country.
Infectious Disease Risks
All travelers should be up to date on their routine immunizations. Varicella is endemic to Mexico, and measles and mumps outbreaks in Mexico have coincided with worldwide and regional outbreaks. Hepatitis A is also endemic to Mexico; visitors should receive ≥1 dose of the hepatitis A vaccine series before travel.
Enteric Infections & Diseases
Cholera
Isolated cases and outbreaks of Vibrio cholera occur occasionally in Mexico. Risk for infection is low, however, and cholera vaccination is not recommended for travelers to Mexico.
Giardiasis
Giardia is endemic throughout the world. In addition to drinking water precautions, remind travelers to avoid swallowing water when swimming or wading in recreational waters, including pools and lakes (see Sec. 5, Part 3, Ch. 12, Giardiasis).
Taeniasis & Cysticercosis
Taeniasis in humans, a tapeworm infection, is caused by ingestion of the eggs of 3 Taenia parasite species in raw or undercooked beef or pork (see Sec. 5, Part 3, Ch. 22, Taeniasis). Taeniasis can present as a mild or asymptomatic intestinal infection. Cysticercosis, a more serious infection of muscle, brain, or other tissues, is caused by ingestion of the larval cysts of Taenia solium excreted by human carriers (see Sec. 5, Part 3, Ch. 6, Cysticercosis). Over months to decades, the infection can progress to neurocysticercosis, a rare but potentially disabling or fatal infection. T. solium is endemic to Mexico. Undercooked vegetables contaminated with T. solium larvae could be the major source of cysticercosis infection.
Travelers’ Diarrhea
Travelers’ diarrhea commonly affects visitors to Mexico. Education is key to prevention; provide travelers with instructions on safe food and water precautions (see Sec. 2, Ch. 8, Food & Water Precautions). Remind travelers that tap water in Mexico is not potable; that they should avoid consuming unpasteurized, often artisanal, dairy products, particularly soft or fresh cheeses; and that they should avoid eating raw or undercooked meat or fish, leafy greens, or raw vegetables. For further information about travelers’ diarrhea, see Sec. 2, Ch. 6, Travelers’ Diarrhea.
Typhoid Fever
Typhoid fever is endemic to Mexico and can be life-threatening (see Sec. 5, Part 1, Ch. 24, Typhoid & Paratyphoid Fever). The Centers for Disease Control and Prevention (CDC) recommends that most travelers to Mexico get the typhoid vaccine, especially people planning to stay with friends or relatives, and those visiting smaller cities or rural areas. Vaccinated travelers also should follow food and water precautions to prevent typhoid fever and other enteric infections.
Respiratory Infections & Diseases
Coronavirus Disease 2019
All travelers going to Mexico should be up to date with their COVID-19 vaccines.
Endemic Fungi
Coccidioides is endemic to the soil of northwestern Mexico and Histoplasma is found mainly in Mexico’s central and southeast regions (see Sec. 5, Part 4, Ch. 1, Coccidioidomycosis / Valley Fever, and Sec. 5, Part 4, Ch. 2, Histoplasmosis). Anyone planning to participate in soil disrupting activities (e.g., construction or farming) should be aware of the risks for and symptoms of fungal lung infection, and practice mitigation techniques. For prevention measures, see the NIOSH Valley Fever and Histoplasmosis.
Influenza
Influenza strains circulate in Mexico, just as they do in the United States. Pretravel influenza vaccination ≥2 weeks before departure is a prudent health protection measure.
Legionnaires’ Disease
Consider legionellosis in the differential diagnosis of travelers who develop pneumonia within 14 days of travel, especially older and immunocompromised people (see Sec. 5, Part 1, Ch. 9, Legionnaires’ Disease & Pontiac Fever). Travel histories for people returning from Mexico who were diagnosed with Legionnaires’ disease periodically identify associations between the disease and stays at specific hotels and resorts in Mexico.
Tuberculosis
Mexico is considered a moderate-incidence country for tuberculosis (TB). TB incidence in Mexico is lower than in Africa, Asia, and Eastern Europe, but incidence is several-fold greater than in the United States. Help travelers determine their potential for exposure to Mycobacterium tuberculosis. Risk for infection is greatest among people intending to remain in Mexico ≥6 months; anyone planning to work in places where they could be exposed to patients with untreated TB (e.g., drug rehabilitation centers, health care settings, prisons, shelters); people planning extended or frequent visits home to spend time with friends and relatives; or people eating unpasteurized dairy products (see Sec. 5, Part 1, Ch. 22, Tuberculosis).
Sexually Transmitted Infections & HIV
HIV prevalence in Mexico is low, except among high-risk populations (e.g., sex workers, injection drug users, men who have sex with men). Other sexually transmitted infections, including chlamydia, gonorrhea, and syphilis, also are more prevalent in these populations. Travelers should avoid condomless sex with unknown or unfamiliar partners (condoms are easily available for purchase in Mexico) and injection drug use.
For people expecting to stay in Mexico ≥6 months, medical tourists, or anyone who might be exposed to blood or other body fluids, including through sexual contact, hepatitis B vaccine is recommended.
Soil- & Waterborne Infections
Cutaneous Larva Migrans
More remote (i.e., less visited) beaches pose a risk for cutaneous larva migrans (CLM), a creeping skin eruption commonly associated with dog hookworm infection (see Sec. 5, Part 3, Ch. 4, Cutaneous Larva Migrans, and Sec. 11, Ch. 8, Dermatologic Conditions). Resort areas implementing stray cat and dog removal programs have reduced the chances of infection on their beaches. CLM is preventable by wearing shoes and avoiding direct skin contact with soil and sand.
Vectorborne Diseases
Arboviruses: Chikungunya, Dengue & Zika
Counsel all travelers to Mexico, including those visiting friends or relatives frequently or for extended periods, to take steps to prevent mosquito bites by using insect repellent, wearing long-sleeved shirts and long pants, and staying in accommodations with air conditioning or screens (see Sec. 4, Ch. 6, Mosquitoes, Ticks & Other Arthropods).
Chikungunya has been reported in Mexico since 2014 (see Sec. 5, Part 2, Ch. 2, Chikungunya). Dengue is endemic throughout Mexico; virus transmission is a risk year-round, and large outbreaks occur periodically (see Sec. 5, Part 2, Ch. 4, Dengue). Zika also is a risk in Mexico (see Sec. 5, Part 2, Ch. 27, Zika). Because of the risk for birth defects in infants born to mothers infected with Zika during pregnancy, people who are pregnant or trying to become pregnant, and their sex partners, should be aware of the most recent CDC recommendations.
Leishmaniasis
Sand flies that transmit cutaneous leishmaniasis are found in southern Mexico and along parts of both the Pacific and Gulf coasts (see Sec. 5, Part 3, Ch. 14, Cutaneous Leishmaniasis). Risk for infection is greatest for ecotourists, field biologists, and long-term travelers. Travelers can reduce their risk for sand fly bites by avoiding outdoor activities at night, wearing protective clothing and applying insect repellent to exposed skin and under the edges of clothing; and sleeping in air-conditioned or well-screened areas.
Malaria
Dramatic decreases in malaria incidence in recent decades mean risk for infection among travelers to Mexico is low. Major resorts are free of the disease, as is the US–Mexico border region. Plasmodium vivax malaria prophylaxis is currently recommended only for travelers going to Chiapas and the southern part of Chihuahua (see Sec. 2, Ch. 5, Yellow Fever Vaccine and Malaria Prevention Information, by Country). Mosquito avoidance (but not chemoprophylaxis) is recommended for travelers visiting Campeche, Durango, Nayarit, Quintana Roo, Sinaloa, Sonora, and Tabasco.
Rickettsial Disease
In Mexico, rickettsial diseases include tickborne Rocky Mountain spotted fever (RMSF), which potentially is fatal unless treated promptly with a tetracycline; and fleaborne typhus, a disease with dengue-like symptoms (see Sec. 5, Part 1, Ch. 18, Rickettsial Diseases). Mexico’s large urban and rural stray dog population is a reservoir for the RMSF vector, Rhipicephalus sanguineus, the brown dog tick. Risk for infection is greatest among people who have contact with dogs, and visitors to grassy, brushy, or wooded areas, particularly in states along the US–Mexico border, including Baja California, Sonora, Chihuahua, and Coahuila. Provide travelers with information about how to avoid flea and tick bites, both indoors and outside (Sec. 4, Ch. 6, Mosquitoes, Ticks & Other Arthropods).
Trypanosomiasis
Chagas disease, transmitted by triatomine insects infected with Trypanosoma cruzi, is endemic throughout Mexico (see Sec. 5, Part 3, Ch. 25, American Trypanosomiasis / Chagas Disease). In 2017, the national incidence was reported to be 0.70 cases (<1 case) per 100,000 population, varying by year and state. Most cases occur along the Pacific Coast and the Gulf of Mexico, and in central and southern Mexico. The risk for travelers is believed to be extremely low; risk might be heightened for travelers staying in poor-quality housing in endemic regions.
Environmental Hazards & Risks
Air Pollution
Air pollution in Mexico City has decreased in recent years. It can still be particularly severe during the dry winter months, however, exacerbating asthma and aggravating chronic lung and heart conditions (see Sec. 4, Ch. 3, Air Quality & Ionizing Radiation).
Altitude Illness
Mexico City is over a mile high (2,250 m; 7,382 ft). Healthy travelers coming from lower elevations and people with heart and lung conditions might require an acclimatization period (see Sec. 4, Ch. 5, High Elevation Travel & Altitude Illness).
Animal Bites
Rabies
In late 2019, the World Health Organization declared Mexico free from human rabies transmitted by dogs. Other animals, including bats, coatis (also known as coatimundi, cholugo, moncún, or tejón), coyotes, foxes, and skunks, are reported carriers of rabies virus. Preexposure rabies prophylaxis is recommended for adventure travelers, ecotourists, field biologists, and others participating in activities where they are at increased risk for wildlife exposure, and also for those visiting less developed, remote areas of the country where access to medical care is limited. Rabies immune globulin for postexposure prophylaxis is available in Mexico (see Sec. 5, Part 2, Ch. 18, Rabies).
Scorpions, Snakes & Other Venomous Wildlife
When visiting rural areas or participating in outdoor activities, especially during spring and summer, travelers should be aware of Mexico’s diverse venomous creatures. Injuries and deaths caused by Centruroides genus (bark) scorpions have been reported from states along the Pacific Coast and in the central states of Durango, Guanajuato, State of Mexico, and Morelos. Other potential exposures include bites from pit vipers (Agkistrodon, Bothrops, and Crotalus spp.), coral snakes (Micruroides spp.), and spiders (Latrodectus and Loxosceles spp.), and stings from fire ants, bees, and wasps (see Sec. 4, Ch. 7, Zoonotic Exposures: Bites, Stings, Scratches & Other Hazards). Antidotes and antivenoms are available at some locations in Mexico.
Beach & Ocean Exposures
Sargassum Seaweed
Sargassum (brown seaweed) season occurs during the warmer months, typically April–August along Mexico’s Caribbean coastline. Exposure to decomposing seaweed can result in difficulty breathing, headaches, nausea, and skin eruptions called “swimmers’ dermatitis.” Advise travelers to avoid direct skin exposure to Sargassum seaweed and, if exposed, to rinse themselves with copious amounts of fresh water and to seek medical attention if they experience respiratory trouble.
Climate & Sun Exposure
Mexico’s climate varies by region, season, and elevation. Longer wavelength ultraviolet (UV) A and shorter wavelength UVB rays intensify at southern latitudes. Travelers engaging in outdoor activities should use broad-spectrum sunscreen (readily available for purchase in Mexico) and use caution with prolonged or repetitive sun exposure to avoid sunburn (see Sec. 4, Ch. 1, Sun Exposure).
Natural Disasters
Earthquakes
Sitting atop 3 large tectonic plates, Mexico is one of the most seismically active countries in the world; 80% of earthquakes are registered in the southeastern region. Travelers should follow the audible earthquake early warning system and evacuation instructions, typically posted in large buildings.
Hurricanes
Hurricane season extends from mid-May–November. Travelers, especially to coastal regions, should be alert to weather reports. After tropical storms or hurricanes, travelers should be mindful of the potential increased incidence of diarrheal illnesses and mosquito-borne diseases.
Toxic Exposures
Lead
Lead can be present in traditional Mexican pottery. Although many traditional potters have switched to lead-free glazes, their kilns might remain contaminated from past use. Lead can leach into food and into beverages prepared, stored, and served in these dishes. The effects of lead poisoning depend on the amount and duration of exposure, and the age of the person intoxicated. The US Food and Drug Administration (FDA) strongly advises against using pottery with leachable lead for cooking, serving, or storing food and drink. Lead-testing kits can help assess safety.
Mercury
Occasional reports of severe mercury poisoning associated with use of Mexican skin-lightening creams should serve as a warning against the purchase of any cosmetics that claim to treat acne, lighten the skin, or fade freckles or age spots.
Safety & Security
Crime
Although travel to Mexico is generally considered safe, thefts and robberies do occur, and drug-related violence exists (see Sec. 4, Ch. 11, Safety & Security Overseas). Travelers should consult the US Department of State website for relevant safety and security alerts pertaining to their intended destinations within Mexico.
Political Unrest
Frequent protests occur in the big cities. Demonstrations are usually peaceful but can be large and worsen already congested traffic. When possible, travelers should avoid protests and the surrounding areas.
Traffic-Related Injuries
Injuries, not infectious diseases, pose the greatest life threat to healthy travelers in Mexico. In one review, about half (51%) of all US traveler deaths in Mexico were injury-related, with 18% due to motor vehicle crashes (see Sec. 8, Ch. 5, Road & Traffic Safety). Mexico’s highway system and roads are mostly modern, well-maintained, and safe. Toll highways are often of higher quality. Nevertheless, driving in city traffic and at night through the countryside can be dangerous. Remind travelers to use seat belts when riding in cars. Helmet use when riding a bicycle or motorbike is highly recommended, although not strictly enforced.
Availability & Quality of Medical Care
Good health care is available in most cities in Mexico, and tourist hotels and resorts usually have physicians available. Payment (cash or credit card) might be required before any care is given. Most providers do not accept US health insurance or Medicare/Medicaid plans.
Medical Tourism
Many US residents visit Mexico to receive health services. Medical tourists going to Mexico primarily seek cosmetic surgery, dental, and eye care services from providers in northern border cities. Increasingly, a complete range of services and specialized procedures for medical tourists are being made available in Cancún, Guadalajara, Mérida, Mexico City, Monterrey, and Tijuana, cities that feature a more robust infrastructure.
Some people who travel to Mexico for medical care have become infected with antimicrobial- resistant strains of bacteria not commonly found in the United States (see Sec. 11, Ch. 5, Antimicrobial Resistance). In 2019, for example, CDC warned medical tourists against having invasive medical procedures performed in specific hospitals and cities due to risk for infection with carbapenem-resistant Pseudomonas aeruginosa. People considering travel to Mexico for medical procedures are advised to consult with a US health professional ≥1 month before departure and to verify provider qualifications and facility credentials in Mexico. Local standards for facility accreditation and provider certification differ from those in the United States. Make potential medical tourists aware of the additional inherent risks associated with surgery, medical procedures, and traveling while being treated for a medical condition or during recovery (see Sec. 6, Ch. 4, Medical Tourism).
Many people also travel to Mexico to purchase more affordable prescription drugs. The FDA recommends only purchasing medications from legal sources in the United States because the safety and effectiveness of drugs purchased in other countries cannot be assured (see Sec. 6, Ch. 3, . . . perspectives: Avoiding Poorly Regulated Medicines & Medical Products During Travel). The agency has posted guidance regarding the importation of drug or device products into the United States from other countries.
The following authors contributed to the previous version of this chapter: Margarita E. Villarino, Sonia H. Montiel, Kathleen Moser