Volume 10, Number 9—September 2004
Research
Foodborne Botulism in the United States, 1990–2000
Abstract
Foodborne botulism, a potentially lethal neuroparalytic disease, is caused by ingesting preformed Clostridium botulinum neurotoxin. We reviewed surveillance data and reports from 1990 to 2000. Of 263 cases from 160 foodborne botulism events (episode of one or more related cases) in the United States, 103 (39%) cases and 58 events occurred in Alaska. Patients’ median age was 48 years; 154 (59%) were female; the case-fatality rate was 4%. The median number of cases per event was 1 (range 1–17). Toxin type A caused 51% of all cases; toxin type E caused 90% of Alaska cases. A particular food was implicated in 126 (79%) events. In the lower 49 states, a noncommercial food item was implicated in 70 (91%) events, most commonly, home-canned vegetables (44%). Two restaurant-associated outbreaks affected 25 persons. All Alaska cases were attributable to traditional Alaska Native foods. Botulism prevention efforts should be focused on those who preserve food at home, Alaska Natives, and restaurant workers.
Botulism is a paralytic illness caused by neurotoxins of the anaerobic, spore-forming bacterium, Clostridium botulinum, and rarely, by botulinum toxin–producing strains of C. baratii and C. butyricum. Seven immunologically distinct toxins exist, designated A through G. Types A, B, and E cause most human cases; type F cases have been reported rarely. Botulinum neurotoxins induce blockage of voluntary motor and autonomic cholinergic neuromuscular junctions, which prevents motor fiber stimulation. Clinical illness is characterized by cranial nerve palsies, followed by descending flaccid muscle paralysis, which can involve the muscles of respiration. Although ptosis and dysarthria may be mistaken for signs of encephalopathy, patients are fully alert, and the results of a sensory examination are normal. Recovery often takes weeks to months (1). The mainstays of therapy are meticulous intensive care unit support, with mechanical ventilation if needed, and administration of equine antitoxin (2). Timely antitoxin administration may arrest the progression of paralysis and decrease the duration of illness (2).
Foodborne botulism is a rare illness caused by eating foods contaminated with botulinum toxin. Spores of C. botulinum are ubiquitous in the environment (3), but growth and elaboration of toxin occur only under particular conditions that include an anaerobic, low-salt, low-acid environment. Bacterial growth is inhibited by refrigeration below 4°C, heating above 121°C, high water activity,or acidity (pH <4.5) (4). Toxin is destroyed by heating to 85°C for at least 5 minutes, and spores are inactivated by heating to 121°C under pressure of 15–20 lb/in2 for at least 20 minutes (5).
The canning and fermentation of foods are particularly conducive to creating anaerobic conditions that allow C. botulinum spores to germinate. Botulism was first described in consumers of sausages in Europe in the 18th century, and commercially canned foods caused outbreaks in the 19th and early 20th centuries before standard methods for inactivating C. botulinum spores in cans were perfected (6). Early in the 20th century, the proportion of botulism outbreaks caused by contaminated, commercially produced foods declined; however, improperly made home-canned foods have long constituted a major source of botulism in the continental United States (1,7). Since the 1970s, restaurant-associated botulism outbreaks have accounted for a large proportion of U.S. cases (8). Traditional Alaska Native foods, especially fermented foods like fish and fish eggs, seal, beaver, and whale, also pose a risk and account for the high incidence of botulism in Alaska (9). These foods, prepared by allowing the products to ferment at ambient temperatures, are often eaten without cooking.
Because contamination of a widely distributed food product could affect large numbers of persons, intensive surveillance is maintained for botulism cases in the United States, and every case is treated as a public health emergency. The Centers for Disease Control and Prevention (CDC) is the only source of therapeutic antitoxin, which is stocked in locations around the country for rapid release. CDC maintains a 24-hour clinical consultation and emergency antitoxin release service, and state health departments conduct epidemiologic investigations of suspected cases (http://www.cdc.gov/ncidod/dbmd/diseaseinfo/botulism.pdf) (1). Clinicians who suspect that they are treating a case of botulism should immediately contact their state health department’s emergency telephone number. Botulinum toxin has been developed as a biologic weapon by various countries and terrorist groups and could be disseminated by deliberate contamination of foods or aerosolization (10). This situation adds urgency to early recognition and reporting of botulism cases. We review surveillance data on cases and outbreaks of botulism in the United States from 1990 to 2000.
Suspected and confirmed botulism cases are reported to CDC by state health departments. Surveillance data, published and unpublished case reports, and outbreak reports were reviewed. A case of foodborne botulism was defined as a compatible illness in a person whose serum, stool, or gastric secretions tested positive for botulinum toxin; a compatible clinical illness in a person who ate food that tested positive for botulinum toxin; a compatible illness in a person whose stool was culture-positive for C. botulinum; a compatible illness in a person who ate food that was also eaten by a person with a laboratory-confirmed case; or a designation of the illness as foodborne botulism by the reporting state health department. An outbreak was defined as two or more cases of botulism caused by consuming a common source–contaminated food. An event was defined as the occurrence of a sporadic case or an outbreak of botulism. A food was considered the source of an outbreak if it tested positive for botulinum toxin and was eaten by a case-patient, or if an epidemiologic investigation linked a food to a botulism event, if the food was not tested. States other than Alaska were designated as the “contiguous states and Hawaii.” Limited clinical data were collected at the time clinicians sought botulinum antitoxin from state health departments and CDC, and changes in data collection practices occurred during the period reported. Toxin detection and culture for C. botulinum were performed at CDC and 19 state and municipal public health laboratories according to standard methods (5). Limited clinical descriptors and outcome data were collected. Statistical analysis was performed using SAS version 8.2. (SAS, Cary, NC).
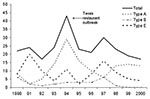
United States
From 1990 to 2000, 160 foodborne botulism events affected 263 people in the United States, an annual incidence of 0.1 per million. No discernable trend was evident in the overall or toxin type–specific annual case counts (Figure). The median number of cases per year was 23 (range 17–43), the median number of events per year was 14 (range 9–24), and the median number of cases per event was 1 (range 1–17). The highest incidence rates were in Alaska, Idaho, and Washington (Table 1). One hundred and thirty-one cases (50%) were caused by toxin type A, 27 (10%) by toxin type B, and 97 (37%) by toxin type E (Table 2). Among case-patients for whom data were available, 67 (26%) persons were intubated. Forty-one (84%) persons with type A intoxication were intubated, compared with 6 (33%) persons with type B and 17 (33%) of those with type E. For case-patients with available data, 7 persons (5%) with type A intoxication died, compared with 1 (4%) with type B and 3 (3%) with type E.
Contiguous States and Hawaii
Events
In the contiguous states and Hawaii, 102 foodborne botulism events occurred, which affected 160 persons; a median of 9 events (range 4–13) and 14 cases (range 4–30) took place per year. The median number of cases per event was 1 (range 1–17). The median age of case-patients in the contiguous states was 50 years (range 4–88 years), and 83 (52%) were female. The overall case-fatality rate was 5%. No clear seasonal pattern was observed.
A food was implicated by laboratory detection of toxin or epidemiologic investigation without laboratory confirmation in 77 (76%) events (Table 3). Of these events, 68 (67%) were caused by homemade foods. Home-canned foods accounted for 47 (69%) of the homemade food events, affecting 70 people, while other types of homemade foods accounted for the remaining 21 (31%) events, which affected 27 people. Of the nine events caused by nonhomemade foods, five (56%) events, which affected 10 people, were caused by commercial foods, and two (22%) events, which affected 25 people, were caused by restaurant-prepared foods.
Improper Food Handling Practices
Improper food handling practices that permit germination and growth of C. botulinum with subsequent toxin elaboration were identified in events involving noncanned homemade foods. For example, salsa made with raw vegetables that were placed in nonrefrigerated airtight plastic containers, which likely fostered an anaerobic environment, was associated with events in 1990 and 1993; each event involved one case-patient. Home-bottled garlic-in-oil was associated with events in 1991 in California and in 1999 in Florida. In one of these events, the garlic-in-oil was prepared by using home-canning methods; the mixture was heated to a temperature insufficient to kill C. botulinum spores (11). Lastly, investigators have suggested that failure to refrigerate freshly made home-cooked foods not normally associated with botulism, such as the beef chili implicated in an outbreak affecting two persons in New Jersey in 2000, can result in toxin production and illness.
Improper food handling practices identified in the five events caused by commercially produced foods (Table 3) include the following. First, an outbreak of botulism type E, affecting three people, was caused by mohola, a salt-cured traditional Egyptian fish product, reportedly purchased at an ethnic New Jersey retail fish market in 1992 (12). Second, an event of botulism type B, which affected one person in Oregon in 1997, was caused by a commercially produced burrito purchased at a roadside store. Third, an event of botulism type A, which affected one person in California in 1994, was attributable to a commercially produced bean dip that was stored in an airtight plastic container at room temperature; the “keep refrigerated” instruction on the container was in minuscule print. Fourth, an outbreak of botulism type A, which affected two people in California in 1994, was caused by a commercially produced clam chowder. The chowder was a low-acid product packed in a sealed plastic bag. Though the product was perishable and was sold in the refrigerated section of a grocery store, it carried no “perishable” label with instructions to refrigerate, as required by California state law. The case-patients stored the soup at room temperature for several weeks and then ate it despite its bad odor and flavor. Fifth, an outbreak of botulism type B, affecting three persons in Hawaii in 1990, was caused by commercially caught, retail-sold palani (surgeon fish). The fish was bought fresh, grilled, and eaten immediately; severe illness appeared to be associated with eating the cooked fish intestines (13).
Two outbreaks caused by restaurant-prepared foods involved skordalia, a potato-based dip, and a commercially canned cheese sauce. The first outbreak occurred in Texas in 1993 and affected 17 persons. The skordalia was prepared with potatoes that were baked in aluminum foil wrapping, then left wrapped in the foil at ambient temperature for several days (14). The second outbreak occurred in Georgia in 1993 and affected eight persons. It involved canned cheese sauce eaten after the opened can was left in the restaurant without refrigeration (15).
Botulinum Toxin Types
During the period under study, 60 events were caused by type A botulinum toxin. The implicated foods in 40 (50%) were home-canned products (27 vegetable items, two home-canned soups, two home-canned tuna items, one each home-canned tomato juice, garlic-in-oil, and stew). Other implicated home-prepared foods included five events from potato salad or potatoes, four from homemade soup, two from homemade sausage, and one from each of the following: roast beef, liver paté, bread pudding, salsa, apple pie, hamburger, and chili. In 18 (23%) events caused by botulinum toxin type A, the specific food vehicle was not identified.
During the period under study, 15 events were caused by type B botulinum toxin. The implicated foods in five (33%) of the type B toxin events were home-canned products (corn, eggs, green beans, olives, and an unspecified vegetable), and one event was due to each of the following: a commercially manufactured burrito, commercially caught and sold fish, pasta sauce and meatballs, salsa, turnip greens, and peyote. In four (25%) events, the food vehicle was not identified.
Three events, all attributable to consumption of fish, were caused by botulinum toxin type E. In one event, the toxin type was not identified.
Alaska
During the period under study, 58 botulism events occurred in Alaska; 103 persons were affected, with a median of 5 events (range 0–15) and 8 cases (range 0–20) occurring per year. The median number of cases per event was 1 (range 1–5). Most events occurred in the spring through the fall, with a sharp peak in July. The median age of case-patients was 44 years (range 8–92), and 70 (68%) were female. The case-fatality rate was 3%. The contaminated food was identified in 49 (84%) of events. All identified foods were homemade Alaska Native foods. Eleven events, affecting 21 persons, were caused by foods consisting of fermented aquatic mammal tissues, such as muktuk (whale skin and blubber), beaver tail, and seal flipper. Fourteen events, affecting 20 persons, were caused by seal oil; 14 events, affecting 28 persons, were caused by fish foods such as fermented salmon heads and whitefish; 7 events, affecting 18 persons, were caused by fermented fish eggs; and 3 events, affecting 5 persons, were caused by foods with mixed ingredients. Forty-nine (84%) events and 91 (88%) cases were caused by toxin type E, all involving foods from aquatic animals. Eight (14%) events with 11 (11%) cases were caused by toxin type B; 6 of these events were caused by animal foods of aquatic origin, and two were caused by unknown foods. In one event caused by fermented seal, the toxin type was not identified.
U.S. Foodborne Botulism Cases with No Food Vehicle Identified
During the period under study, 37 cases of botulism were reported by state health departments as foodborne botulism attributable to an unknown food; these represented 14% of all cases. Of these, six were associated with outbreaks of two or more cases and therefore can be considered with certainty to be foodborne. The characteristics of the remaining 31 sporadic cases reported as foodborne, but not having an identified food, resembled those of other foodborne botulism cases. Twenty-two (61%) patients were female, and the median age was 55 (range 42–84). Seventeen (55%) cases were caused by toxin type A, 6 (19%) by toxin type B, 5 (16%) by toxin type E, and 3 (10%) by toxin type F. One (3%) case-patient died.
In previous eras, conditions conducive to the survival of C. botulinum spores and their subsequent germination in food were much more common. Nevertheless, enduring methods of preparing certain homemade foods, new ways of packaging commercial foods, new food preferences, or new techniques for preparing familiar foods that support the growth of C. botulinum render it likely that foodborne botulism will afflict humans for the foreseeable future.
From 1990 to 2000, home-canned foods remained a leading cause of foodborne botulism in the United States. New interventions should be explored to ensure that methods of home canning vegetables incorporate adequate barriers to prevent C. botulinum germination. Possible areas of research may include development of practical dye indicators for pH and temperatures above those of refrigeration. Botulism associated with Alaska Native foods is likely an age-old problem, compounded in recent decades by altering traditional practices in an unsafe manner, in particular, to include the use of plastic or glass containers for fermentation. To address this problem, the Alaska State Department of Health and Social Services, in partnership with CDC, has developed culturally appropriate educational materials on safer native food preparation. The preventive message focuses on handwashing, using safer, traditional fermentation processes, avoiding plastic and glass containers, shielding fermenting food from sunlight, boiling native foods before consumption, and discarding suspicious foods (www.phppo.cdc.gov/phtn/botulism/default/default.asp) (16).
C. botulinum rarely causes illness because the confluence of conditions required for its germination and toxin production—low acidity, high water activity, absence of preservatives, ambient temperature, and anaerobic milieu—rarely occurs in foods (4). However, from 1990 to 2000, preservative-free, low-salt, commercially produced foods packaged in air-tight containers with no intrinsic barriers to C. botulinum spore germination were popular, possibly because they are perceived by the public as healthier. The sole barrier to C. botulinum germination in these foods is refrigeration. The outbreaks attributable to commercial bean dip and clam chowder exemplify the failure of this lone safeguard. Prevention could be enhanced by mandating multiple barriers to spore germination, such as acidification and reduced water activity, along with prominent refrigeration instructions, in all low-oxygen packaged commercial foods.
Botulism from traditional recipes of uneviscerated fish is well documented in such preparations as Egyptian fasikh (17) and East-European kapchunka (18). The 1992 outbreak from moloha (Table 3) falls into this category. Current regulations prohibit the sale of uneviscerated fish (19). The outbreak from palani in Hawaii in 1990 is novel because the commercially caught fish was purchased fresh at a retail establishment, cooked, and served immediately (13). Control measures include appropriate refrigeration between catch and sale, similar to those used to control scombroid poisoning (20). From 1990 to 2000, restaurant-associated outbreaks continued to cause a disproportionate number of botulism cases. Investigation of the skordalia dip outbreak identified the practice of leaving baked potatoes wrapped in foil at ambient temperature as the principal hazard; this practice must be completely eliminated from restaurants and homes. Control measures depend on the education of restaurant operators and enforcement by sanitation authorities.
Thirty-one reported sporadic foodborne cases had no identified contaminated food source. Were these, in fact, cases of foodborne botulism? The median age, gender distribution, and fatality rate were similar to those of other foodborne cases, and no patients were reported to be injection drug users, the leading risk factor for wound botulism (21). However, some of these may represent cases of adult intestinal toxemia botulism (AITB) or adult-infant botulism. The diagnosis of AITB is difficult to establish because it requires proof of in vivo toxin production by demonstrating botulinum toxin or C. botulinum in patient specimens over time (22). Absence of a toxin-containing food, identification of C. botulinum in stool, and a history of abnormal bowel anatomy or recent antimicrobial drug use support the diagnosis of AITB (23,24). Some AITB cases may have been misclassified as foodborne. All three cases of botulism type F reported from 1990 to 2000 were reported as foodborne but with no implicated food. Since identification of type F toxin in food is practicable (25,26), failure to implicate a food may indicate these cases were misclassified AITB. For patients with sporadic cases of adult botulism with no implicated food or injection drug history, repeated stool cultures over time may help establish the diagnosis of AITB. As the clinical syndrome of inhalational botulism probably does not differ from that of foodborne botulism (27), the possibility of aerosol exposure should be considered in otherwise unexplained cases.
Our data have several limitations. Most clinical data were collected at one point, when antitoxin was sought by the treating clinician from CDC or a state health department. Changes in reporting format during the period reported resulted in incomplete data for a substantial portion of cases. Differences in toxin type–specific rates of intubation and deaths on a subset of cases must be cautiously interpreted in light of these facts.
Foodborne botulism, while rare, remains a public health emergency because of its severity and epidemic potential. Home-canned foods and Alaska Native foods remain the leading causes in the United States, and restaurant-associated outbreaks continue to account for a disproportionate number of illnesses. All suspected cases of botulism should be reported to public health authorities immediately. Prompt epidemiologic investigation helps prevent additional cases and can identify new risk factors for intoxication.
Dr. Sobel is a medical epidemiologist in the Foodborne and Diarrheal Diseases Branch, CDC. His research interests include the epidemiology of bacterial enteric infections with a special focus on botulism.
References
- Shapiro R, Hathaway C, Swerdlow DL. Botulism in the United States: a clinical and epidemiologic review. Ann Intern Med. 1998;129:221–8.PubMedGoogle Scholar
- Tacket CO. SW, Mann JM, Hargrett NT, Blake PA. Equine antitoxin use and other factors that predict outcome in type A foodborne botulism. Am J Med. 1984;76:794–8. DOIPubMedGoogle Scholar
- Houschild AHW. Clostridium botulinum. In: Doyle M, editor. Foodborne bacterial pathogens. New York: Marcel Dekker; 1989. p. 112–89.
- International Commission on Microbiological Specifications for Foods. Clostridium botulinum. In: Micro-organisms in foods 5: characteristics of microbial pathogens. New York: Blackie Academic & Professional; 1996. p. 68–111.
- Centers for Disease Control and Prevention. Botulism in the United States, 1899–1996, handbook for epidemiologists, clinicians and laboratory workers. Atlanta: The Centers; 1998.
- Meyer K. The protective measures of the state of California against botulism. J Prevent Med. 1931;5:261–93.
- MacDonald KL, Cohen ML, Blake PA. The changing epidemiology of adult botulism in the United States. Am J Epidemiol. 1986;124:794–9.PubMedGoogle Scholar
- Wainright RB, Middaugh JP, Hatheway CL, Harpster AP, Bender TR. Food-borne botulism in Alaska, 1947–1985: epidemiology and clinical findings. J Infect Dis. 1988;157:1158–62.PubMedGoogle Scholar
- Arnon SS, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS. Botulism toxin as a biological weapon: medical and public health management. JAMA. 2001;285:1059–70. DOIPubMedGoogle Scholar
- Morse DL, Guzewich JJ, Devine BD, Shayegani M. Garlic-in-oil associated botulism: episode leads to product modification. Am J Public Health. 1990;80:1372–3. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Outbreak of type E botulism associated with an uneviscerated, salt-cured fish product—New Jersey, 1992. MMWR Morb Mortal Wkly Rep. 1992;41:521–2.PubMedGoogle Scholar
- Centers for Disease Control. Fish botulism—Hawaii, 1990. MMWR Morb Mortal Wkly Rep. 1991;40:412–4.PubMedGoogle Scholar
- Angulo FJ, Getz J, Taylor JP, Hendricks KA, Hatheway CL, Barth SS, A large outbreak of botulism: the hazardous baked potato. J Infect Dis. 1998;178:172–7.PubMedGoogle Scholar
- Townes J, Cieslak PR, Hatheway CL, Solomon HM, Hollaway JT, Baker MP, An outbreak of type A botulism associated with a commercial cheese sauce. Ann Intern Med. 1996;125:558–63.PubMedGoogle Scholar
- Centers for Disease Control and Prevention. Botulism outbreak associated with eating fermented food—Alaska, 2001. MMWR Morb Mortal Wkly Rep. 2001;50:680–2.PubMedGoogle Scholar
- Weber JT, Darwish A, Mishu B, Corwin AL, Rakha M, Hatheway CL, A massive outbreak of type E botulism associated with traditional salted fish in Cairo. J Infect Dis. 1993;167:451–4.PubMedGoogle Scholar
- Centers for Disease Control. Botulism associated with commercially distributed Kapchunka—New York City. MMWR Morb Mortal Wkly Rep. 1985;34:546–7.PubMedGoogle Scholar
- Food and Drug Administration (FDA). Compliance policy guide: compliance policy guidance for FDA staff. Section 540.650: Uneviscerated fish products that are salt-cured, dried, or smoked (CPG 7108.17). Washington: FDA; 2000.
- Centers for Disease Control and Prevention. Scombroid fish poisoning—Pennsylvania, 1998. MMWR Morb Mortal Wkly Rep. 2000;49:398–400.
- Werner SB, Passaro D, McGee J, Schechter R, Vugia D. Wound botulism in California, 1951–1998: recent epidemic in heroin injectors. Clin Infect Dis. 2000;31:1018–31. DOIPubMedGoogle Scholar
- Arnon S. Botulism as an intestinal toxemia. In: Blaser MJ, Ravdin JI, Greenberg HB, Guerrant RL, editors. Infections of the gastrointestinal tract. New York: Raven Press; 1995. p. 257–71.
- McCroskey LM, Hatheway CL. Laboratory findings in four cases of adult botulism suggest colonization of the intestinal tract. J Clin Microbiol. 1988;26:1052–4.PubMedGoogle Scholar
- McCroskey L, Hatheway CL, Woodruff BA, Greenberg JA, Jurgenson P. Type F botulism due to neurotoxigenic Clostridium baratii from an unknown source in an adult. J Clin Microbiol. 1991;29:2618–20.PubMedGoogle Scholar
- Moller V. Preliminary report on the isolation of an apparently new type of Cl. botulinum. Acta Pathol Microbiol Scand. 1960;48:80. DOIPubMedGoogle Scholar
- Center for Disease Control. Botulism type F—California. MMWR Morb Mortal Wkly Rep. 1966;15:359.
- Middlebrook JL, Franz DR. Botulinum toxins. In: FR Sidell, ET Takafuji, DR Franz, editors. Medical aspects of chemical and biological warfare. Washington: Borden Institute, Walter Reed Army Medical Center; 1998. p. 643–54.
Figure
Tables
Cite This ArticleTable of Contents – Volume 10, Number 9—September 2004
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Jeremy Sobel, Foodborne and Diarrheal Diseases Branch, Centers for Disease Control and Prevention, 1600 Clifton Road, Mailstop A38, Atlanta, GA 30333, USA; fax: 404-639-2205
Top