Volume 15, Number 2—February 2009
Dispatch
Vaccine-induced Immunity Circumvented by Typical Mycobacterium tuberculosis Beijing Strains
Abstract
The frequency of typical and atypical Beijing strains of Mycobacterium tuberculosis was determined in the Netherlands; Vietnam; and Hong Kong Special Administrative Region, People’s Republic of China. The strains’ associations with drug resistance, M. bovis BCG vaccination, and patient characteristics were assessed. BCG vaccination may have positively selected the prevalent typical Beijing strains.
Mycobacterium tuberculosis Beijing strains cause a substantial proportion of tuberculosis (TB) cases worldwide (1). Experiments in a BALB/c mouse model (2) and a rabbit model (3) supported the hypothesis that Beijing strains might represent “escape variants” of M. bovis BCG vaccination (4). In a study in Ho Chi Minh City, Vietnam, presence of a BCG scar correlated, but not significantly, with infection by Beijing strains (5).
The Beijing clade is highly prevalent in Asia, where the proportion of TB cases caused by strains of this clade usually is stable over time, and no association with drug resistance has been recorded. In other areas (e.g., Cuba, South Africa, countries of the former Soviet Union, and Vietnam), Beijing strains are emerging and associated with resistance to anti-TB drugs (1). The Beijing clade comprises at least 2 major subgroups, which share the characteristic spoligotype pattern (6–8): typical and atypical Beijing strains. Typical (“modern” [8,9]) Beijing strains, including W strains (7), exhibit highly similar, multicopy insertion sequence (IS) 6110 restriction fragment length polymorphism (RFLP) patterns and have alterations in putative mutator genes (4,10). Atypical (“ancestral” [8,9]) Beijing strains more closely resemble the common ancestor of the Beijing clade (6–8,10). The ability of these Beijing clade subgroups to gain resistance or circumvent BCG vaccine–induced immunity may differ and thus explain the differences in geographic distribution of Beijing strains and the variation in association with drug resistance. However, few studies have distinguished between subgroups of the Beijing clade, or studies were limited in the number of strains analyzed (8,9,11,12).
We used 3 large data sets from previously described studies to investigate possible differences in correlation with resistance and BCG vaccination between sublineages of the Beijing clade. Details about drug-susceptibility testing, DNA fingerprinting, and demographics by origin can be found elsewhere (5,13,14). In the Netherlands, 415 (6%) of 6,829 M. tuberculosis isolates with available IS6110 RFLP patterns from 1993 through 2000 were of the Beijing clade (13); approximately one third of cases each originated in the Netherlands and Asia and the remaining one third in other areas (13). In Vietnam, 301 (53%) of 563 isolates from new TB cases, collected during 1998–1999 mainly in Ho Chi Minh City, belonged to the Beijing clade (5). In Hong Kong Special Administrative Region, People’s Republic of China, 355 (71%) of 500 randomly selected M. tuberculosis isolates collected during 1998–1999 from patients before treatment were of the Beijing clade (14). Information about patient sex and age was available from all 3 sites. Drug susceptibility data and BCG status of patients (presence/absence of BCG scar) were not available from Hong Kong. The patients in this study were treated according to World Health Organization guidelines, independent from their M. tuberculosis isolates’ genotype.
Beijing clade strains were defined by their spoligotype pattern (6). We used the multiplex PCR of Plikaytis et al. (15) to differentiate 3 subgroups of the Beijing clade (W strain, typical, atypical). A specific IS6110 insertion in the NTF region is detected in typical Beijing strains (7). W strains, a subgroup of typical Beijing strains, contain this IS6110 and an additional IS6110 insertion in this region (7,15). Figure 1 shows the correlation between the multiplex PCR results and IS6110 RFLP similarity.
A total of 1,023 M. tuberculosis Beijing clade isolates (410 from the Netherlands, 268 from Vietnam, and 345 from Hong Kong) were available for multiplex PCR analysis. Mean age category of patients was 25–34 years, and >75% were <45 years of age. Because the W strain occurred infrequently, we included it in our analysis of the typical Beijing strain.
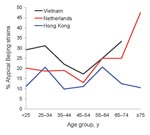
Typical and atypical subgroups were equally distributed among men and women but varied by country and patient age. Atypical Beijing strains occurred in 25.4% (68/268) of isolates in Vietnam, 21.2% (87/410) in the Netherlands, and 13.6% (47/345) in Hong Kong. Atypical Beijing strains were encountered less frequently in Hong Kong than in Vietnam (p<0.001) and the Netherlands (p = 0.007). The Beijing subgroups were equally prevalent among persons of different age groups in Hong Kong, but atypical Beijing strains occurred more frequently in older persons in the Netherlands and Vietnam (Figure 2). This increase in proportion of atypical Beijing strains in older persons was significant in the Netherlands (χ2trend 4.5, p<0.035). Combined data for the Netherlands and Vietnam showed significantly more atypical Beijing isolates among patients >75 years of age (odds ratio [OR] 2.96, 95% confidence interval [CI] 1.15–7.67) (Table 1), which suggests more recent introduction and spread of typical Beijing strains.
To determine whether BCG vaccination might drive this shift in prevalence of the 2 Beijing subgroups, we investigated their distribution in persons vaccinated and not vaccinated with BCG. Of 249 nonvaccinated persons, 27.7% were infected with atypical strains; of 265 vaccinated persons, a significantly lower proportion (20.8%) were infected with atypical strains (adjusted OR 0.60, 95% CI 0.38–0.95) (Table 1). The proportions per genotype emphasized this finding; 44.4% of atypical Beijing strains and 53.8% of typical Beijing strains were isolated from vaccinated persons. The association between typical Beijing strains and vaccination was strong in the data from the Netherlands: 14.2% of Beijing strains isolated from vaccinated persons and 31% of those from nonvaccinated persons were atypical (adjusted OR 0.39, 95% CI 0.20–0.76). In Vietnam, the proportions were nonsignificant (26.2% and 24.4%, respectively).
The unknown BCG vaccination status of 164 of 678 Beijing strain–infected patients is a limitation of our study. In these patients (from the Netherlands), the proportion of atypical Beijing strains was lower and almost similar to that for vaccinated patients. Therefore, if all patients with unknown BCG status were considered nonvaccinated, the association with typical Beijing strains and BCG vaccination would disappear. However, the Netherlands’ National Tuberculosis Register most likely lacks BCG status data because the BCG status for these patients was not checked; we assume the absence of these data introduced no bias. To investigate this further, we extended the analysis of the population in the Netherlands by including all patients with known BCG status (n = 4,004). The proportions of typical Beijing strains for BCG-vaccinated and BCG-nonvaccinated persons were 54.2% and 45.8%, respectively. For all strains other than Beijing strains (i.e., atypical Beijing strains and M. tuberculosis strains of all other genotypes), these proportions were 44.5% and 55.5%, respectively. Thus, including all isolates from persons with known BCG status, typical Beijing strains still were isolated significantly more often from BCG-vaccinated than BCG-nonvaccinated persons (p = 0.008). Our findings of significantly fewer typical Beijing isolates among patients >75 years of age (mostly experiencing reactivation and thus representing the population structure of M. tuberculosis of decades ago) and significantly more isolates of typical Beijing strains from BCG-vaccinated persons support the hypothesis that BCG vaccination might favor the spread of the typical Beijing strains.
Drug resistance of M. tuberculosis Beijing subgroups varied by country (Table 2). In Vietnam, drug resistance was significantly higher than in the Netherlands; 6.7% of Beijing strains in Vietnam compared with 2.0% in the Netherlands were multidrug resistant (MDR), 32.1% compared with 11.0% were isoniazid (INH) resistant, and 44.0% compared with 15.9% were streptomycin resistant (Table 2). Atypical Beijing isolates were more often INH resistant (25.2%) than were typical Beijing isolates (17.6%). Furthermore, atypical Beijing strains were more often MDR (7.1% compared with 2.9%). Atypical Beijing strains were less often streptomycin resistant (21.3% compared with 28.7%) (Table 2). Thus, atypical Beijing isolates were associated with INH resistance and MDR and significantly less likely to be streptomycin resistant than typical Beijing isolates. Similar differences in drug resistance recently were found for the 2 Beijing subgroups among isolates circulating in Japan (12) and in the Beijing region of China (9), but the findings in China were not statistically significant, probably because of the limited number of stains analyzed. These differences in drug resistance associations suggest the different Beijing sublineages might have different mechanisms of drug resistance development.
Despite the association of atypical Beijing strains with INH and multidrug resistance found in this study, typical Beijing strains contribute most substantially to the worldwide MDR TB epidemic (1,4,11). However, in studies showing an association between typical Beijing strains and multidrug resistance, these strains usually also were resistant to streptomycin (as we also found). Typical Beijing strains may therefore become streptomycin resistant more easily, eventually leading to MDR TB, as the W-strain outbreak in New York showed (16). Alternatively, the increased prevalence of typical Beijing strains in the current global M. tuberculosis population may be caused not by drug-driven selection but by their hypervirulence (2), higher adaptability (10), higher rate of progression to disease, greater ability to circumvent BCG-induced immunity (2,3, this study), or other specific features.
We showed that subgroups of the M. tuberculosis Beijing clade have different associations with drug resistance and BCG vaccination. Individual lineages of the Beijing clade are likely to be evolving in different areas, possibly because of intrinsic strain characteristics, differences in anti-TB drug regimens and BCG-vaccination strategies in different areas, chance, or a combination of these. Thus, anti-TB drugs and BCG vaccination influence the dynamics in the population structure of M. tuberculosis. The efficacy of new candidate TB vaccines therefore should be tested against a broad panel of epidemic strains from all high-prevalence areas (4). Furthermore, treatment of infections by different M. tuberculosis genotypes might require different anti-TB treatment strategies. More extended studies are needed in high-prevalence settings, especially studies of other predominant genotype families of M. tuberculosis.
Dr Kremer is a researcher at the Mycobacterial Reference Unit of the National Institute of Public Health and the Environment, Bilthoven, the Netherlands. Her research interests include the molecular epidemiology and evolution of tuberculosis.
Acknowledgments
We thank Pablo Bifani and Natalia Kurepina for sharing DNA of the W strain and for helpful discussions, Frank Cobelens for helpful comments on the manuscript, and members of the Mycobacteria Reference Unit of the National Institute for Public Health and the Environment for their work on DNA fingerprinting and drug susceptibility testing of M. tuberculosis isolates.
The data from the Netherlands were analyzed with permission of the Registration Commission of the Netherlands Tuberculosis Register (ref. no. 08/2004). This study was supported by the European Union (TBadapt project LSHP-CT-2007-037919 and CAonTB project QLK2-CT-2000-00630).
References
- European Concerted Action on New Generation Genetic Markers and Techniques for the Epidemiology and Control of Tuberculosis. Beijing/W genotype Mycobacterium tuberculosis and drug resistance. Emerg Infect Dis. 2006;12:736–43.PubMedGoogle Scholar
- Lopez B, Aguilar D, Orozco H, Burger M, Espitia C, Ritacco V, A marked difference in pathogenesis and immune response induced by different Mycobacterium tuberculosis genotypes. Clin Exp Immunol. 2003;133:30–7. DOIPubMedGoogle Scholar
- Tsenova L, Harbacheuski R, Sung N, Ellison E, Fallows D, Kaplan G. BCG vaccination confers poor protection against M. tuberculosis HN878-induced central nervous system disease. Vaccine. 2007;25:5126–32. DOIPubMedGoogle Scholar
- van Soolingen D, Qian L, de Haas PE, Douglas JT, Traore H, Portaels F, Predominance of a single genotype of Mycobacterium tuberculosis in countries of East Asia. J Clin Microbiol. 1995;33:3234–8.PubMedGoogle Scholar
- Anh DD, Borgdorff MW, Van LN, Lan NT, van Gorkom T, Kremer K, Mycobacterium tuberculosis Beijing genotype emerging in Vietnam. Emerg Infect Dis. 2000;6:302–5.PubMedGoogle Scholar
- Kremer K, Glynn JR, Lillebaek T, Niemann S, Kurepina NE, Kreiswirth BN, Definition of the Beijing/W lineage of Mycobacterium tuberculosis on the basis of genetic markers. J Clin Microbiol. 2004;42:4040–9. DOIPubMedGoogle Scholar
- Kurepina NE, Sreevatsan S, Plikaytis BB, Bifani PJ, Connell ND, Donnelly RJ, Characterization of the phylogenic distribution and chromosomal insertion sites of five IS6110 elements in Mycobacterium tuberculosis: non-random integration in the dnaA-dnaN region. Tuber Lung Dis. 1998;79:31–42. DOIPubMedGoogle Scholar
- Mokrousov I, Narvskaya O, Otten T, Vyazovaya A, Limeschenko E, Steklova L, Phylogenetic reconstruction within Mycobacterium tuberculosis Beijing genotype in northwestern Russia. Res Microbiol. 2002;153:629–37. DOIPubMedGoogle Scholar
- Mokrousov I, Jiao WW, Sun GZ, Liu JW, Valcheva V, Li M, Evolution of drug resistance in different sublineages of Mycobacterium tuberculosis Beijing genotype. Antimicrob Agents Chemother. 2006;50:2820–3. DOIPubMedGoogle Scholar
- Rad ME, Bifani P, Martin C, Kremer K, Samper S, Rauzier J, Mutations in putative mutator genes of Mycobacterium tuberculosis strains of the W-Beijing family. Emerg Infect Dis. 2003;9:838–45.PubMedGoogle Scholar
- Hanekom M, van der Spuy GD, Streicher E, Ndabambi SL, McEvoy CR, Kidd M, A recently evolved sublineage of the Mycobacterium tuberculosis Beijing strain family is associated with an increased ability to spread and cause disease. J Clin Microbiol. 2007;45:1483–90. DOIPubMedGoogle Scholar
- Iwamoto T, Yoshida S, Suzuki K, Wada T. Population structure analysis of the Mycobacterium tuberculosis Beijing family indicates an association between certain sublineages and multidrug resistance. Antimicrob Agents Chemother. 2008;52:3805–9. DOIPubMedGoogle Scholar
- Borgdorff MW, de Haas P, Kremer K, van Soolingen D. Mycobacterium tubercuiosis Beijing genotype, the Netherlands. Emerg Infect Dis. 2003;9:1310–3.PubMedGoogle Scholar
- Chan MY, Borgdorff MW, Yip CW, de Haas PEW, Wong WS, Kam KM, Seventy percent of the Mycobacterium tuberculosis isolates in Hong Kong represent the Beijing genotype. Epidemiol Infect. 2001;127:169–71. DOIPubMedGoogle Scholar
- Plikaytis BB, Marden JL, Crawford JT, Woodley CL, Butler WR, Shinnick TM. Multiplex PCR assay specific for the multidrug-resistant strain W of Mycobacterium tuberculosis. J Clin Microbiol. 1994;32:1542–6.PubMedGoogle Scholar
- Bifani PJ, Plikaytis BB, Kapur V, Stockbauer K, Pan X, Lutfey ML, Origin and interstate spread of a New York City multidrug-resistant Mycobacterium tuberculosis clone family. JAMA. 1996;275:452–7. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleTable of Contents – Volume 15, Number 2—February 2009
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Kristin Kremer, Mycobacteria Reference Unit (Pb 22), Diagnostic Laboratory for Infectious Diseases and Perinatal Screening, National Institute for Public Health and the Environment (RIVM), PO Box 1, 3720 BA Bilthoven, the Netherlands;
Top