Volume 21, Number 2—February 2015
Dispatch
Streptococcus suis Infection in Hospitalized Patients, Nakhon Phanom Province, Thailand
Abstract
In Nakhon Phanom, Thailand, we identified 38 hospitalized patients with Streptococcus suis infection during 2006–2012. Deafness developed in 12 patients; none died. Thirty-five reported recent exposure to pigs/pork. Annual incidence was 0.1–2.2 cases/100,000 population (0.2–3.2 in persons >20 years of age). Clinicians should consider S. suis infection in areas where pig exposure is common.
Streptococcus suis, a zoonotic pathogen found primarily in pigs, can cause serious infection in humans. Most cases in human occur in Southeast Asia, where pig rearing is common (1). In a recent global review, Thailand had the second highest number of reported cases, accounting for 11% of all reported cases worldwide (2). In Thailand, the first 2 cases of S. suis in humans were reported in 1987 (3). From 1997 (when S. suis infection was first reportable) through 2010, a total of 692 cases were reported (0–207 per year); nearly half were from northern Thailand (4). The national annual crude incidence rate was 0–0.381 per 100,000 persons (Table 1). The objective of this study was to describe persons hospitalized with, and incidence of, S. suis infection in Nakhon Phanom during 2006–2012.
In 2003, the Thailand Ministry of Public Health and the US Centers for Disease Control and Prevention established hospital-based surveillance for community-acquired acute lower respiratory infections (ALRI) at all 12 acute-care hospitals in Nakhon Phanom Province (northeastern Thailand; population 761,623) (5). In 2005, surveillance was expanded to include bloodstream infections, supported by the addition of an automated blood culture system and improved microbiology capacity (6). Blood was collected for culture at clinician discretion but encouraged for all patients with ALRI and children <5 years of age who had sepsis. Incidence of pneumococcal bacteremia (all ages) and other bloodstream infections (children <5 years) was previously published (6,7). This work was considered public health surveillance and thus exempt from institutional review board review.
Blood put into a blood culture bottle was transported at 15–30°C within 24 hours to the provincial hospital laboratory and processed by using the BacT/ALERT 3D automated blood culture system (bioMérieux, Durham, NC, USA). To obtain at least 10 mL per adult patient, we divided specimens into 2 bottles (standard aerobic growth and enhanced growth of fastidious pathogens). Bottles that indicated positive growth were subcultured and processed by standard methods (8). All possible pathogens were confirmed at the National Institute of Health, Ministry of Public Health, by conventional biochemical tests (9). We serotyped S. suis isolates using PCR (10) and confirmed serotypes by coagglutination using rabbit antiserum (Statens Serum Institut, Copenhagen, Denmark). A case of S. suis was defined as illness in a person hospitalized in Nakhon Phanom who had blood culture–confirmed S. suis infection. Two physicians (K.P. and S.S.) reviewed the medical data retrospectively. Patients were interviewed by using a standard protocol (http://www.boe.moph.go.th/files/report/20100902_39823811.pdf). We calculated annual incidence using the estimated population as the denominator (http://www.nesdb.go.th/temp_social/pop.zip).
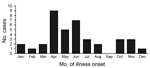
During 2006–2012, there were 56,983 blood cultures from 56,057 patients, an average of 8,008 patients per year (for comparison, in 2005, before microbiology enhancements, 2,340 patients had blood cultured at the provincial hospital). Median age of patients was 44 years (range 23–73 years). A pathogen was identified in 4,097 (7.2%) patients and S. suis in 38 (0.07%). Of the 38 S. suis cases, two occurred in 2006, one in 2007, two in 2008, three in 2009, eight in 2010, five in 2011, and 17 in 2012. Fifty-five percent of cases were identified during April–June (Figure). The annual crude incidence ranged from 0.1 to 2.2 cases per 100,000 population; incidence was highest in 2012 (Table 1). Of persons >20 years of age (all 38 S. suis patients), incidence was highest in 2012 (3.2 cases/100,000 population [range 0.2–3.2/100,000]).
Within 24 hours after hospital admission, all patients were treated with ceftriaxone. In 12 (32%) patients, permanant deafness developed; all had reported hearing loss at admission. Thirty-five (92%) patients had exposure to pigs or pork in the 7 days before illness onset: 10 (26%), all women, reported preparing pork with their bare hands for consumption and eating undercooked pork, 12 (32%) reported eating both undercooked/uncooked pork and clotted pig blood, and 13 (34%) reported slaughtering pigs for their own consumption. Thirteen patients who reported slaughtering pigs also ate pork but stated that they could not recall how the meat was prepared because of having also consumed alcohol. Seven (18%) patients had acquired pigs in poor health from commercial farms at reduced prices or no cost. Patients resided in 18 (19%) of the 96 subdistricts within Nakhon Phanom, and 10 (26%) patients resided in the same subdistrict. Two clusters of cases occurred in 2012, in which 2 and 3 persons ate raw pork and drank alcohol together. All patients reported no prior knowledge of S. suis infection, its symptoms, or ways to prevent infection.
Of the 24 patients with meningitis, 21 (88%) had leukocytosis, 4 (17%) had thrombocytopenia, and 2 (8%) had thrombocytosis. Six of the 24 patients with meningitis had a cerebrospinal fluid (CSF) culture; 1 was positive for S. suis. Of the 10 patients with septicemia, 5 had leukocytosis, 1 had leukopenia, 3 had normal leukocyte counts; for 1, leukocyte count was unavailable. Thirty (79%) isolates were initially reported as Streptococcus group D nonenterococci by the hospital laboratory; the remaining 8 were reported as other streptococcal groups or species (Table 2). The National Institute of Health reference laboratory identified S. suis in 38 patients; all isolates were serotype 2 (PCR and coagglutination results were all concordant). All isolates tested for antimicrobial resistance by disk diffusion (Kirby-Bauer) were susceptible to penicillin (37 isolates) and ceftriaxone (11 isolates). Time from patient blood collection to final pathogen report to the clinician was 30–45 days.
S. suis infection is common in northern Thailand. Here we report laboratory-confirmed cases and incidence in Nakhon Phanom, a northeastern province. Few other studies have reported incidence. The Netherlands reported the most S. suis infections in the West (2) with an estimated annual incidence of S. suis infection of 0.002 cases per 100,000 persons (11), and the incidence in northern Thailand was 6.2 cases per 100,000 persons (12). Active surveillance suggests that S. suis infection might be more common in this region than previously realized (e.g., in 2010, the incidence in Nakhon Phanom was 1.6-fold higher in active than passive reporting; for other years it was greater). During 2006–2012, a total of 45% (17/38) of S. suis infection were detected in 2012, including 2 clusters.
Although we did not have a control group with which to compare exposures, our findings are consistent with studies performed in northern Thailand that highlight pork/pig exposure, combined with alcohol use, as a risk factor (13). Unlike in cases reported in other studies (12), no patients reported here died. Patients were treated promptly with ceftriaxone on the first day of admission, which is standard empiric management of suspected sepsis or meningitis in these hospitals. Permanent hearing loss was common, and deafness is usually permanent when it occurs before treatment (14).
Our data have several limitations. Blood cultures were performed at clinician discretion and not necessarily for all patients with possible sepsis or meningitis, possibly resulting in missed cases or biasing our study toward the more clinically apparent or severe cases. Blood volume might have been too low for adequate pathogen yield. Only 6 patients had CSF cultures, and most blood and CSF cultures occurred after start of antimicrobial therapy. Therefore, meningitis patients with negative blood cultures might have been missed. Furthermore, because comprehensive examinations were not performed on patients after discharge, neurologic or cognitivie sequalae might have been missed.
Because most hospital laboratories in Thailand are not able to confirm S. suis, the infection might be misdiagnosed (14). Clinicians in high-risk areas, or who see patients with recent travel to high-risk areas, should have a low index of suspicion for S. suis infection among patients presenting with meningitis or sepsis and recent pig/pork exposure (15). Improving the capacity of local laboratories to identify S. suis will aid clinical management and facilitate outbreak detection and response. Rapid identification enables faster epidemiologic investigation and swift initiation of control measures (2).
Dr. Prapasiri is an epidemiologist in the Influenza Program at the Thailand Ministry of Public Health–US Centers for Disease Control and Prevention Collaboration. His research interests include the epidemiology of acute respiratory illness and sociocultural risk factors for infectious diseases.
Acknowledgments
We thank Anek Keawpan and Sopida Pookkit for their contributions to this project.
The US Centers for Disease Control and Preventon, the Ministry of Public Health, Thailand, and the Association of Schools and Programs of Public Health (cooperative agreements 5U19GH000004 and U36/CCU300430) provided funding for this study.
References
- Wertheim HF, Nghia HD, Taylor W, Schultsz C. Streptococcus suis: an emerging human pathogen. Clin Infect Dis. 2009;48:617–25. DOIPubMedGoogle Scholar
- Lun ZR, Wang QP, Chen XG, Li AX, Zhu XQ. Streptococcus suis: an emerging zoonotic pathogen. Lancet Infect Dis. 2007;7:201–9. DOIPubMedGoogle Scholar
- Phuapradit P, Boongird P, Boonyakarnkul S, Niramarnsakul S, Ponglikitmongkol S, Vorachit M, Meningitis caused by Streptococcus suis. Intern Med. 1987;3:120–2.
- Thailand Ministry of Public Health Bureau of Epidemiology. Laboratory surveillance of Streptococcus suis. 2013 [cited 2013 Sep 27]. http://www.boe.moph.go.th/Annual/aesr2553/AESR53_Part1/B_Part1_53/2553_StreptococcusLab.pdf.
- Olsen SJ, Thamthitiwat S, Chantra S, Chittaganpitch M, Fry AM, Simmerman JM, Incidence of respiratory pathogens in persons hospitalized with pneumonia in two provinces in Thailand. Epidemiol Infect. 2010;138:1811–22. DOIPubMedGoogle Scholar
- Baggett HC, Peruski LF, Olsen SJ, Thamthitiwat S, Rhodes J, Dejsirilert S, Incidence of pneumococcal bacteremia requiring hospitalization in rural Thailand. Clin Infect Dis. 2009;48(Suppl 2):S65–74. DOIPubMedGoogle Scholar
- Hasan R, Rhodes J, Thamthitiwat S, Olsen SJ, Prapasiri P, Naorat S, Incidence and etiology of acute lower respiratory tract infections in hospitalized children younger than 5 years in rural Thailand. Pediatr Infect Dis J. 2014;33:e45–52. DOIPubMedGoogle Scholar
- Perilla MJ, Ajello G, Bopp C, Elliott J, Facklam R, Knapp JS, Manual for the laboratory identification and antimicrobial susceptibility testing of bacterial pathogens of public health importance in the developing world. Geneva: World Health Organization; 2003.
- Facklam R. What happened to the streptococci: overview of taxonomic and nomenclature changes. Clin Microbiol Rev. 2002;15:613–30. DOIPubMedGoogle Scholar
- Kerdsin A, Akeda Y, Hatrongjit R, Detchawna U, Sekizaki T, Hamada S, Streptococcus suis serotyping by a new multiplex PCR. J Med Microbiol. 2014;63:824–30. DOIPubMedGoogle Scholar
- Arends JP, Zanen HC. Menigitis caused by Streptococcus suis in humans. Rev Infect Dis. 1988;10:131–7. DOIPubMedGoogle Scholar
- Fongcom A, Pruksakorn S, Netsirisawan P, Pongprasert R, Onsibud P. Streptococcus suis infection: a prospective study in northern Thailand. Southeast Asian J Trop Med Public Health. 2009;40:511–7 .PubMedGoogle Scholar
- Khadthasima N, Sutdan D, Noimoh T, Chalamat M, Thannawitjaya P, Areechoechai D, Outbreak investigation of Streptococcus suis in Phusang district, Payao Province, May 2007. Wkly Epidemiol Surveill Rep. 2007;38:393–8 [cited 2013 Sep 27]. http://203.157.15.4/wesr/file/y50/F50231.pdf
- Donsakul K, Dejthevaporn C, Witoonpanich R. Streptococcus suis infection: clinical features and diagnostic pitfalls. Southeast Asian J Trop Med Public Health. 2003;34:154–8 .PubMedGoogle Scholar
- Teekakirikul P, Wiwanitkit V. Streptococcus suis infection: overview of case reports in Thailand. Southeast Asian J Trop Med Public Health. 2003;34(Suppl 2):178–83 .PubMedGoogle Scholar
Figure
Tables
Cite This ArticleTable of Contents – Volume 21, Number 2—February 2015
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Address for correspence: Prabda Praphasiri, Thailand MOPH–US CDC Collaboration, DDC Bldg 7, 4th Fl, Ministry of Public Health, Soi 4, Tivanon Rd, Nonthaburi 11000, Thailand
Top