Volume 18, Number 4—April 2012
Research
Comparison of Escherichia coli ST131 Pulsotypes, by Epidemiologic Traits, 1967–2009
Abstract
Escherichia coli sequence type 131 (ST131), an emerging disseminated public health threat, causes multidrug-resistant extraintestinal infections. Among 579 diverse E. coli ST131 isolates from 1967–2009, we compared pulsotypes (>94% similar XbaI pulsed-field gel electrophoresis profiles) by collection year, geographic origin, source, and antimicrobial drug–resistance traits. Of 170 pulsotypes, 65 had >2 isolates and accounted for 85% of isolates. Although extensively dispersed geographically, pulsotypes were significantly source specific (e.g., had little commonality between humans vs. foods and food animals). The most prevalent pulsotypes were associated with recent isolation, humans, and antimicrobial drug resistance. Predominant pulsotype 968 was associated specifically with fluoroquinolone resistance but not with extended-spectrum β-lactamase production or blaCTX-M-15. Thus, several highly successful antimicrobial drug–resistant lineages within E. coli ST131 have recently emerged and diffused extensively among locales while maintaining a comparatively restricted host/source range. Identification of factors contributing to this behavior of ST131 could help protect public health.
The prevalence of resistance to fluoroquinolones and extended-spectrum cephalosporins in Escherichia coli has increased dramatically over the past decade. This increase is largely the result of the widespread emergence of a single disseminated E. coli clonal group, designated sequence type (ST) 131 according to multilocus sequence typing (MLST) (1,2). E. coli ST131 is characterized by serotype O25b:H4 and often produces CTX-M-15 or other extended-spectrum β-lactamases (ESBLs) (3–5). Unlike most other antimicrobial drug–resistant E. coli, ST131 derives from virulence-associated phylogenetic group B2 and typically exhibits multiple virulence factors, including adhesins, siderophores, toxins, and group 2 capsule (1–7). It thereby poses the dual threat of extensive antimicrobial drug resistance plus virulence.
By definition, ST131 is homogeneous with respect to housekeeping gene sequence across the 7 MLST loci; however, within-lineage genetic variation has been noted since ST131 was first described (3–5). Specifically, diversity of pulsed-field gel electrophoresis (PFGE) profiles has provided insights into the ecology of ST131. For example, the presence of ST131 isolates with similar PFGE profiles in widely dispersed locales and of isolates with quite different profiles in the same locale has suggested rapid and ongoing global dissemination of ST131 (3,8). Likewise, recovery of ST131 isolates with similar PFGE profiles from multiple household members (9–12) and from food animals (or retail meats) and humans (13) has suggested host-to-host or foodborne transmission, respectively, as potential mechanisms for dissemination of ST131.
However, relevant studies to date have included relatively few isolates, locales, and sources and limited time periods (2,6). In addition, the idiosyncratic nature of PFGE analysis precludes across-study comparisons. Thus, we analyzed 579 ST131 isolates from diverse sources according to a standardized PFGE protocol and then compared PFGE profiles with other characteristics, including geographic origin, time of collection, ecologic source, and antimicrobial drug–resistance traits.
Isolates
The 579 ST131 study isolates, some previously published (3,9–12,14–19), were compiled as a series of convenience samples from collaborators in diverse locales. The isolates came already identified as ST131 or as generic E. coli in need of screening for ST131 status. They derived mostly from collections assembled by investigators or reference laboratories on the basis of specific resistance phenotypes, O antigens, geographic origins, and/or clinical syndromes of interest. Some isolates were from cases or case series involving infected humans or animals with distinctive signs and symptoms and/or predisposing conditions (9–12,14,15).
Isolates were accompanied by data regarding date of isolation (or receipt in the reference laboratory), ecologic source (i.e., host species, food, or water), and locale of origin. For some isolates, data were available regarding resistance-associated characteristics, i.e., fluoroquinolone resistance; ESBL production; and presence of blaCTX-M-15, which encodes the CTX-M-15 ESBL variant. If not provided, this information was newly generated.
ST131 Status
Of the 579 study isolates, 34 (5.9%) came already defined as ST131 by 7-locus MLST (http://mlst.ucc.ie/mlst/dbs/Ecoli). The remaining 545 (94.1%) were presumptively identified as ST131 in the study laboratory by PCR-based screening for ST131-specific single-nucleotide polymorphisms (SNPs) in gyrB and mdh (17). Full MLST was done de novo for 57 (10.5%) of these presumptive ST131 isolates, which represented diverse time periods, locales, sources, and resistance characteristics; in each instance, presumptive ST131 status was confirmed (SNP PCR specificity 100%; 95% CI 94%–100%). Thus, 91 (16%) isolates were directly confirmed by MLST to be ST131. Another 301 (52%) isolates represented pulsotypes with >1 MLST-confirmed ST131 isolate, which indirectly confirmed their ST131 status. Therefore, in total, 392 (68%) isolates were directly or indirectly confirmed by MLST to be ST131. Of the 31 earliest isolates (1967–1997), including the 5 earliest isolates (1967–1986), 32% were directly confirmed by MLST to be ST131.
PFGE Analysis
PFGE analysis of XbaI-restricted total DNA of isolates was performed according to a standardized protocol (20) by a single observer in 1 laboratory. Profiles were captured and analyzed digitally by using BioNumerics software version 6.6 (Applied Maths, Austin, TX, USA). Marker lanes in each gel (E. coli O157:H7 strain g5244) enabled normalization within and across gels. Band positions were assigned manually, with computer assistance. The band tolerance setting, as derived empirically from analysis of multiple same-isolate profiles, was 1.15%.
Pairwise Dice similarity coefficients were used to define pulsotypes. Isolates exhibiting >94% profile similarity (≈3-band difference) to the index isolate for an established pulsotype, implying genetic similarity (21), were assigned to that pulsotype; others became the index isolate for a new pulsotype. Newly encountered pulsotypes were numbered sequentially. A PFGE profile dendrogram was constructed according to the unweighted pair group method for 87 (15%) of the isolates (selected randomly after inclusion of 2 representatives of each pulsotype with >6 members) plus the earliest isolated (1967) and earliest published (1985) isolates (8).
Susceptibility Testing
Disk diffusion testing for ciprofloxacin susceptibility and ESBL production was performed on isolates of unknown fluoroquinolone or ESBL phenotype as described (22,23). Fluoroquinolone resistance was defined as nonsusceptibility to ciprofloxacin.
Statistical Analyses
Geographic origin was categorized as United States (with 4 subregions—West, Midwest, South, and Northeast—as defined by the US Census Bureau [www.census.gov/geo/www/us_regdiv.pdf]), Canada, and other international locales combined. Ecologic source was categorized as human, companion animal, food animal, other animal, food, and water. Year of isolation/submission was assessed both continuously and categorically (e.g., pre-1990 vs. later).
Comparisons of proportions were tested by using 2-tailed Fisher exact (unpaired comparisons) and McNemar (paired comparisons) tests. Comparisons involving continuous variables were tested by using the Mann-Whitney U test (2-tailed). Other variables were assessed as independent predictors of selected pulsotype categories by using multivariable logistic regression analysis. The significance criterion was p<0.05.
Isolate Origins and Characteristics
The 579 ST131 study isolates were derived from humans (486 [84%]), animals (77 [13%]), environmental sources (15 [3%]), and an unknown source (n = 1). Animal uses included companion (22 [4%]), food (45 [8%]), and other (10 [2%]). Environmental sources included food (6 [1%]) and water (9 [2%]). Geographic origins included the United States (446 [77%]), Canada (53 [9%]), and other international locales (80 [14.1%]). The US isolates were from the West (59 [10%]; 9 centers, 4 states), Midwest (180 [31%] centers, 11 states), South (98 [17%] centers, 9 states), and Northeast (109 [19%] centers, 7 states). Isolates from Canada were from 9 centers in 8 provinces. Other international isolates were from 11 centers in 11 countries (Australia, Chile, France, South Korea, Lebanon, India, Italy, Peru, Portugal, Spain, Switzerland). Dates of isolation/submission ranged from 1967 through 2009 (median year 2007). Twenty (4%) isolates were isolated/submitted during 1967–1989, the 5 earliest during 1967, 1982, 1983, 1985, and 1986; 22 (4%) were isolated/submitted during 1990–1999; and 537 (93%) were isolated/submitted during 2000–2009. Overall, 462 (80%) isolates were fluoroquinolone-resistant, 272 (47%) were ESBL-producers, and 188 (33%) had blaCTX-M-15.
Pulsotypes
XbaI PFGE analysis resolved 170 distinct pulsotypes, each accounting for 1 isolate (105 pulsotypes) to 136 isolates (1 pulsotype, type 968). The 105 single-isolate pulsotypes collectively accounted for 105 isolates (18% of total); the 65 multiple-isolate pulsotypes accounted for the remaining 474 isolates (82% of total). Among the multiple-isolate pulsotypes, 12 contained >6 isolates each (i.e., >1% of the population), collectively accounting for 327 isolates (56% of total). The multiple-isolate pulsotypes contained 62 clusters of isolates (each comprising 2–5 isolates; total 150 isolates) with indistinguishable profiles.
Temporal Patterns
Pulsotypes varied significantly by temporal occurrence. The 65 multiple-isolate pulsotypes and 12 high-prevalence pulsotypes were significantly associated with more recent dates of isolation/submission, relative to the low-prevalence and single-isolate pulsotypes (Table 1). Temporal variation was also evident among the 12 high-prevalence pulsotypes; 4 were significantly associated with later and 1 (type 955) with earlier occurrence (Table 1).
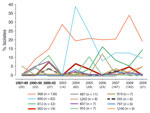
Analysis of temporal prevalence trends (Figure) showed that the 12 high-prevalence pulsotypes accounted collectively for only 5% of 20 isolates during the earliest period (1967–1989) but for 58% of isolates during subsequent years (p<0.001). Three of these pulsotypes (988, 800, 812) were the top 1, 2, or 3 most prevalent, overall and within each interval from 1990 forward. These 3 types appeared sequentially by overall pulsotype prevalence (i.e., in 1990–1999 for type 968, in 2000–2002 for type 800, and in 2005 for type 812) and, except for type 800 in 2003, were detected continuously after first appearing. After it appeared, type 968 maintained a consistently high prevalence (>19%), whereas types 800 and 812 exhibited early prevalence spikes followed by sizeable drops. In contrast, the 9 other high-prevalence types appeared intermittently, which, depending on the pulsotype, was mostly in earlier years, later years, or sporadically throughout (Figure).
A temporal trend was also evident in the PFGE dendrogram (Figure A1), which extended to 67% similarity. The more highly similar PFGE profiles in the upper region of the tree involved mostly recent isolates and higher prevalence pulsotypes, whereas the more basal, dissimilar profiles toward the lower region of the tree involved more older isolates (including isolates from 1967, 1982, 1985, and 1986) and low-prevalence pulsotypes.
Geographic Distribution
The pulsotypes primarily exhibited a broad geographic distribution, yet there was some geographic segregation. Table 2 shows the number of mutually exclusive geographic regions (among 6 total) in which each of the 65 multiple-isolate pulsotypes were found. Only 18 of 65 multiple-isolate pulsotypes were limited to a single geographic region (p<0.001 for occurrence in 1 vs. multiple regions, McNemar test). Moreover, these 18 pulsotypes included only 2 (13 pulsotypes), 3 (4 pulsotypes), or 4 (1 pulsotype) isolates each and represented <50% of pulsotypes within their size category. In contrast, all pulsotypes including >5 isolates were found in multiple geographic regions, and 3 of the 6 pulsotypes comprising >8 isolates spanned all 6 geographic regions (Table 2). Table 3 shows the overlap among regions by the number of shared pulsotypes and by the number of isolates in these pulsotypes. Each region overlapped partially with every other region (Table 3).
Against this background of broad geographic distribution, substantial geographic segregation of pulsotypes was evident. For example, at the isolate level, each region was negatively associated with at least 1 other region; the US West and non-Canadian international sites exhibited the greatest number of such negative associations, suggesting somewhat locale-specific pulsotype populations in these regions (Table 3). The only positive association between nonoverlapping regions involved the US Midwest and Canada.
Table 4 provides a pulsotype-level analysis of these geographic associations. For example, the high-prevalence and multiple-isolate pulsotypes were collectively significantly overrepresented in Canada, and the high-prevalence pulsotypes were also significantly underrepresented in the United States, specifically, in the US West. Among individual high-prevalence pulsotypes, 968 was overrepresented in the US Midwest and under-represented in the US West; 800 was over-represented in Canada and under-represented in the United States and the US West; 812 was over-represented in the US South; 987 was over-represented internationally (specifically in Australia, data not shown) and under-represented in the United States; and 1202 was over-represented in the US West (Table 4).
Source Distribution
In contrast with the generally broad geographic distribution of pulsotypes, the source distribution was more restricted, and source-specific segregation predominated over across-source commonality. For example, only 13 of 65 multiple-isolate pulsotypes spanned multiple sources (p<0.001, McNemar test); most of these included only 2 sources each, and none included >4 (of 6 possible) sources (Table 2).
Likewise, the by-source distribution of pulsotypes (Table 5) showed less overall commonality than did geographic distribution. Still, it showed multiple positive and negative associations at the isolate and the pulsotype level. Specifically, isolates from humans were associated positively with pulsotypes comprising isolates from water and negatively with pulsotypes comprising isolates from companion animals, food animals, or food. Isolates from companion animals were associated positively with pulsotypes containing isolates from other animals, and isolates from food animals were associated positively with pulsotypes containing isolates from food (Table 5). In addition, pulsotypes containing isolates from food animals were associated negatively with pulsotypes containing isolates from humans, but they were associated positively with pulsotypes containing isolates from food (Table 5).
Significant by-source segregation also was evident for individual pulsotypes (Table 6). Collectively, the multiple-isolate and high-prevalence pulsotypes were associated positively with humans and negatively with food animals and environmental sources, and high-prevalence pulsotypes were associated with companion animals. Furthermore, 5 high-prevalence pulsotypes were individually significantly distributed by source: type 968 was associated positively with pets and other animals and negatively with food animals and environmental sources, 800 was associated positively with humans and negatively with food animals, 812 was associated positively with humans, 1202 was associated negatively with humans and positively with food animals, and 955 was associated negatively with humans and positively with pets and environmental sources (Table 6). Five additional pulsotypes, comprising 2 food animal isolates each, were significantly associated with food animals (p = 0.004 for each; data not shown).
Antimicrobial Drug Resistance
Fluoroquinolone resistance, ESBL production, and blaCTX-M-15 also segregated significantly by pulsotype in varied patterns (Table 7). The high-prevalence and multiple-isolate pulsotypes collectively and type 968 were associated positively with fluoroquinolone resistance but indifferently with ESBL production and blaCTX-M-15. In contrast, type 800 was associated positively with fluoroquinolone resistance but negatively with ESBL production and blaCTX-M-15, whereas types 905, 812, and 919 were associated positively with all 3 traits, and type 987 was associated negatively with all 3 traits (Table 7).
Multivariable Analysis
All 3 resistance traits, plus several source groups and geographic regions, exhibited significant associations with year of isolation/submission (Table 1), suggesting possible confounding by temporal correlations among variables. Thus, we used multivariable logistic regression analysis to assess for independent associations of selected predictor variables with pulsotype. Separate models were constructed for the 3 most prevalent pulsotypes, the high-frequency pulsotypes, and the multiple-isolate pulsotypes, by using as candidate predictor variables 1 representative from each epidemiologic or resistance category (year, ecologic source, locale, fluoroquinolone phenotype, and ESBL status). ESBL status was a significant predictor in all 5 resulting models, as was fluoroquinolone resistance in 4 models (fluoroquinolone resistance was excluded from the fifth model because of its 100% prevalence in pulsotype 812), year in 3 models, and human source in 2 models (Table 8). In contrast, US origin (the representative geographic variable) was not a significant predictor in any model.
Indistinguishable PFGE Profile Isolates
We also assessed associations with other variables for the 7 largest clusters of isolates with indistinguishable PFGE profiles; each cluster contained 4–5 isolates. Of the 31 constituent isolates, 28 were recent (2007–2009) and the other 3 were from 2002 or 2004. Of the 7 clusters, 6 included isolates from multiple locales, from multiple continents in 3 instances. In contrast, only 3 clusters came from multiple host species. Whereas each cluster was internally homogeneous for fluoroquinolone phenotype (6 all-resistant clusters, 1 all-susceptible cluster), 4 were internally heterogeneous according to ESBL and/or blaCTX-M-15 status.
We used PFGE analysis to define population structure among 579 diverse E. coli ST131 isolates and then assessed temporal, geographic, ecologic, and resistance trait associations for the various pulsotypes, i.e., presumed sub-ST genetic lineages. Our findings support 4 main conclusions. First, although ST131 is highly diverse at the pulsotype level, a small number of high-frequency pulsotypes predominate, and pulsotype 968 accounts for 24% of the population. Second, pulsotypes differ in prevalence over time; high-prevalence pulsotypes tend to occur in more recent years, consistent with recent emergence and expansion, implying greater fitness. Third, whereas broad geographic distribution predominates over locale-specific segregation, implying widespread dispersal rather than localized endemicity, segregation by ecologic source predominates over across-source commonality, implying niche adaptation rather than broad host-range capability and interspecies transmission. Fourth, resistance traits (i.e., fluoroquinolone resistance, ESBL production, and blaCTX-M-15) are highly pulsotype-specific, suggesting predominantly subclonal distribution.
The striking prevalence disparities among pulsotypes suggest that certain pulsotypes, especially the exceptionally successful pulsotype 968, possess fitness advantages over others. In retrospect, pulsotype 968 accounted for all previously reported household clusters, 3 of which involved serious or fatal disease in >1 household members (9–12). A possible founder effect for type 968 is unlikely because the pulsotypes that were detected earliest were mostly low-prevalence types; higher prevalence pulsotypes appeared only later, seemingly outcompeting the low-prevalence types. In regard to possible fitness advantages, ESBL production and blaCTX-M-15 were significantly associated with several high-prevalence pulsotypes and were present in most or all of their members (Table 7). However, they were not significantly associated with (predominant) pulsotype 968 and so are unlikely the main explanation for the recent expansion of ST131, of which pulsotype 968 was the single main component (Figure). In contrast, fluoroquinolone resistance was significantly associated with each of the 4 most prevalent pulsotypes and collectively with the 12 high-prevalence and 65 multiple-isolate pulsotypes. Thus, fluoroquinolone resistance may have made a major contribution to the recent expansion of ST131.
Although the predominant pattern was broad dispersal of pulsotypes, localized segregation also occurred. These trends imply considerable ongoing dissemination and intermixing of ST131 lineages among locales (sufficient to largely preclude establishment of locale-specific populations) but with variable degrees of intermixing versus segregation by locale and pulsotype. For example, the US Midwest and Canada shared pulsotypes more extensively than did other regions. Conversely, non-Canadian international locales and the US West had less pulsotype commonality with other regions (i.e., had more highly locale-specific populations) than did other locales. Several high-prevalence pulsotypes similarly exhibited distinct patterns of distribution and were variably concentrated in specific regions. Similar patterns have been described previously for ST131 but in lesser detail and without statistical analysis (3,6,8,17,24,25). The undefined mechanisms for the ongoing dispersal of ST131, possibly including international travel and commerce, wild bird migration, and foodborne or waterborne transmission, and its limited locale-specific segregation by pulsotype warrant study.
The associations of specific pulsotypes with different ecologic sources are relevant to the dispersal mechanisms of ST131. In contrast to the striking geographic dissemination of pulsotypes, we also found some evidence of niche segregation. Positive associations for niche segregation were found between humans and water, companion animals and other animals, and food animals and food. In contrast, negative associations were found between humans and most other sources, companion animals or other animals and food or food animals, and water and companion animals or food animals. These findings implicate humans as the source for ST131 isolates found in water and implicate food animals as the source for isolates found in food. In contrast, and consistent with findings in most, but not all, previous studies (13,26–28), these findings indicate that food animals and food are not major sources of ST131 for humans. They also suggest no special pet–human commonality of ST131 pulsotypes, notwithstanding some well-documented overlap (29). This argues against pets and the food supply as major vehicles for dissemination of ST131 strains among humans. Indeed, in 1 study, 7% of healthy humans were found to be colonized intestinally with an ST131 strain (30); thus, humans may be the main reservoir for human-associated strains. A larger, more current, and more systematically assembled study population is needed to confirm the findings of the present study.
Until now, the earliest reported isolate of ST131 was from a patient with urosepsis in 1985 (8). Here, we report 3 earlier isolations, from 1967, 1982, and 1983, none of which were from a high-prevalence pulsotype. This finding documents the presence of ST131 decades before its emergence as a disseminated human pathogen and suggests an opportunity to compare early isolates with recent isolates for characteristics that might confer enhanced fitness, possibly contributing to the emergence of ST131.
Our study had limitations. First, the population was a convenience sample with multiple possible sources of bias. Second, despite considerable diversity, the population was not balanced; it predominantly comprised recent isolates from human in the United States, reducing both generalizability and power for comparisons involving other times, sources, and regions. Third, minimal associated data (especially clinical details) were available for many isolates, limiting the possible epidemiologic analyses. Fourth, PFGE profiles reflect genetic relationships only indirectly and require subjective interpretation. Fifth, the multiple comparisons could have produced spurious associations by chance alone. However, the proportion of comparisons yielding a significant p value was much greater, and the associated p values much smaller, than should occur by chance alone. Last, the 94% PFGE similarity pulsotype criterion was somewhat arbitrary and possibly suboptimal; however, an alternate 100% similarity criterion yielded qualitatively similar conclusions.
Our study also had strengths. The population was the largest reported to date for ST131 (2) and the most extensively distributed by time, source, and region. The PFGE analysis was conducted by 1 experienced observer in 1 laboratory by using software that enabled concurrent comparisons for all isolates. Diverse univariable and multivariable statistical approaches were used, pulsotypes were analyzed collectively and individually, and PFGE profiles were assessed by using 2 similarity thresholds (94% and 100%) and in a dendrogram.
Thus, within a large, diverse collection of E. coli ST131 isolates, we documented extensive PFGE profile diversity and a predominance of certain high-prevalence pulsotypes (particularly pulsotype 968, 24% overall) that exhibited distinctive temporal patterns of emergence. Notwithstanding some geographic localization, pulsotypes were extensively dispersed by region. In contrast, they were more highly source specific; in particular, isolates from humans exhibited almost no commonality with isolates from food animals or foods. Pulsotype 968 was much more closely associated with fluoroquinolone resistance than with ESBL production or blaCTX-M-15, suggesting a greater role for fluoroquinolone resistance than ESBLs in the expansion of this dominant pulsotype and ST131 in general. These findings considerably advance our understanding of the genetic structure, ecology, geographic distribution, and emergence of this widely disseminated antimicrobial drug–resistant pathogen, which represents a growing public health threat.
Dr Johnson is professor of medicine and senior associate director of the infectious diseases fellowship program at the University of Minnesota and head of the molecular epidemiology laboratory at the Minneapolis VA Medical Center. His research focuses on the molecular epidemiology, ecology, evolution, and virulence of extraintestinal pathogenic and antimicrobial drug–resistant E. coli.
Acknowledgments
The MASTER (Macrorestriction Analysis of ST131 for Epidemiologic Research) Investigators who contributed data include Jo-Ellyn Abraham (Abbott-Northwestern Hospital, Minneapolis, Minnesota, USA), Javier Adachi (The University of Texas MD Anderson Cancer Center, Houston, Texas, USA), Aristides Assimacopoulos (University of South Dakota, Souix Falls, South Dakota, USA), Robert L. Bergsbaken (Health Partners and Regions Medical Center, St. Paul, Minnesota, USA), Jorge Blanco (University of Santiago de Compostela, Lugo, Spain), Michael Cooperstock (University of Missouri School of Medicine, Columbia, Missouri, USA), Paul Edelstein (Hospital of the University of Pennsylvania, Philadelphia, Pennsylvania, USA), Peter T. Ender (St. Luke's Hospital and Health Network, Bethlehem, Pennsylvania, USA), Nancy Hansen (Creighton University, Omaha, Nebraska, USA), John Holter (Veterans Affairs Medical Center, Minneapolis), Thomas M. Hooton (University of Miami, Miami, Florida, USA), Michelle Hulse (Childrens Hospital, Minneapolis), James H. Jorgensen and James S. Lewis II (University Health System, San Antonio, Texas, USA), Karen Lolans (Rush Medical School, Chicago, Illinois, USA), Sybille Miller (Leesburg Veterinary Internal Medicine, Leesburg, Virginia, USA), Rob Owens (Cubist Pharmaceuticals, Falmouth, Maine, USA), Elizabeth Palavecino (Wake Forest University Baptist Medical Center, Winston-Salem, North Carolina, USA), David Paterson (University of Pittsburgh, Pittsburgh, Pennsylvania, USA, and Queensland University, Brisbane, Queensland, Australia), Johann D. D. Pitout (Calgary Laboratory Services, Calgary, Alberta, Canada), John P. Quinn (Pfizer Global Research, Groton, Connecticut, USA), James Rice (The Scripps Research Institute, La Jolla, California, USA), Daniel F. Sahm (Eurofins-Medinet, Chantilly, Virginia, USA), and Karen Vigil (University of Texas Health Sciences Center at Houston, Houston)
This material is based on work supported by the Office of Research and Development, Medical Research Service, Department of Veterans Affairs (J.R.J.). Dave Prentiss (Minneapolis VA Medical Center) prepared the figures.
J.R.J. received research funding from Merck and Rochester Medical Group; J.S.L. received research funding and/or honoraria from Merck, Ortho-McNeil, and Pfizer; J.P.Q. is an employee of Astra-Zeneca and a shareholder in Pfizer Global Research.
References
- Peirano G, Pitout JDD. Molecular epidemiology of Escherichia coli producing CTX-M β-lactamases: the worldwide emergence of clone ST131 O25:H4. Int J Antimicrob Agents. 2010;35:316–21. DOIPubMedGoogle Scholar
- Rogers BA, Sidjabat HE, Paterson DL. Escherichia coli O25b-ST131: a pandemic, multiresistant, community-associated strain. J Antimicrob Chemother. 2011;66:1–14. DOIPubMedGoogle Scholar
- Nicolas-Chanoine MH, Blanco J, Leflon-Guibout V, Demarty R, Alonso MP, Caniça MM, Intercontinental emergence of Escherichia coli clone O25:H4–ST131 producing CTX-M-15. J Antimicrob Chemother. 2008;61:273–81. DOIPubMedGoogle Scholar
- Clermont O, Lavollay M, Vimont S, Deschamps C, Forestier C, Branger C, The CTX-M-15producing Escherichia coli diffusing clone belongs to a highly virulent B2 phylogenetic subgroup. J Antimicrob Chemother. 2008;61:1024–8. DOIPubMedGoogle Scholar
- Coque TM, Novais Â, Carattoli A, Poirel L, Pitout J, Peixe L, Dissemination of clonally related Escherichia coli strains expressing extended-spectrum β-lactamase CTX-M-15. Emerg Infect Dis. 2008;14:195–200. DOIPubMedGoogle Scholar
- Gibreel TM, Dodgson AR, Cheesbrough J, Fox AJ, Bolton FJ, Upton M. Population structure, virulence potential and antibiotic susceptibility of uropathogenic Escherichia coli from northwest England. J Antimicrob Chemother. 2012;67:346–56. DOIPubMedGoogle Scholar
- Totsika M, Beatson SA, Sarkar S, Phan MD, Petty NK, Bachmann N, Insights into a multidrug resistant Escherichia coli pathogen of the globally disseminated ST131 lineage: genome analysis and virulence mechanisms. PLoS ONE. 2011;6:e26578. DOIPubMedGoogle Scholar
- Johnson JR, Johnston B, Clabots C, Kuskowski MA, Castanheira M. Escherichia coli sequence type ST131 as the major cause of serious multidrug-resistant E. coli infections in the United States (2007). Clin Infect Dis. 2010;51:286–94. DOIPubMedGoogle Scholar
- Johnson JR, Anderson JT, Clabots C, Johnston B, Cooperstock M. Within-household sharing of a fluoroquinolone-resistant Escherichia coli sequence type ST131 strain causing pediatric osteoarticular infection. Pediatr Infect Dis J. 2010;29:473–5. DOIPubMedGoogle Scholar
- Ender PT, Gajanana D, Johnston B, Clabots C, Tamarkin FJ, Johnson JR. Transmission of extended-spectrum beta-lactamase-producing Escherichia coli (sequence type ST131) between a father and daughter resulting in septic shock and emphysematous pyelonephritis. J Clin Microbiol. 2009;47:3780–2. DOIPubMedGoogle Scholar
- Owens RC, Johnson JR, Stogstill P, Yarmus L, Lolans K, Quinn J. Community transmission in the United States of a CTX-M-15-producing sequence type ST131 Escherichia coli strain resulting in death. J Clin Microbiol. 2011;49:3406–8. DOIPubMedGoogle Scholar
- Johnson JR, Miller S, Johnston B, Clabots C. DebRoy C. Sharing of Escherichia coli sequence type ST131 and other multidrug-resistant and urovirulent E. coli strains among dogs and cats within a household. J Clin Microbiol. 2009;47:3721–5. DOIPubMedGoogle Scholar
- Platell JL, Johnson JR, Cobbold RN, Trott DJ. Multidrug-resistant extraintestinal pathogenic Escherichia coli of sequence type ST131 in animals and foods. Vet Microbiol. 2011;153:99–108. DOIPubMedGoogle Scholar
- Johnson JR, Johnston B, Clabots C, Kuskowski MA, Pendyala S, DebRoy C, Escherichia coli sequence type ST131 as an emerging fluoroquinolone-resistant uropathogen among renal transplant recipients. Antimicrob Agents Chemother. 2010;54:546–50. DOIPubMedGoogle Scholar
- Vigil KJ, Johnson JR, Johnston BD, Kontoyiannis DP, Mulanovich VE, Raad II, Escherichia coli pyomyositis: an emerging entity among patients with hematologic malignancies. Clin Infect Dis. 2010;50:374–80. DOIPubMedGoogle Scholar
- Urban C, Mariano N, Bradford PA, Tuckman M, Segal-Maurer S, Wehbeh W, Identification of CTX-M β-lactamases in Escherichia coli from hospitalized patients and residents of long-term care facilities. Diagn Microbiol Infect Dis. 2010;66:402–6. DOIPubMedGoogle Scholar
- Johnson JR, Menard M, Johnston B, Kuskowski MA, Nichol K, Zhanel GG. Epidemic clonal groups of Escherichia coli as a cause of antimicrobial-resistant urinary tract infections in Canada, 2002–2004. Antimicrob Agents Chemother. 2009;53:2733–9. DOIPubMedGoogle Scholar
- Sidjabat HE, Paterson DL, Adams-Haduch JM, Ewan L, Pasculle AW, Muto CA, Molecular epidemiology of CTX-M–producing Escherichia coli isolates at a tertiary medical center in western Pennsylvania. Antimicrob Agents Chemother. 2009;53:4733–9. DOIPubMedGoogle Scholar
- Lewis JS II, Herrera M, Wickes B, Patterson JE, Jorgensen JH. First report of the emergence of CTX-M–type extended-spectrum beta-lactamases (ESBLs) as the predominant ESBL isolated in a US health care system. Antimicrob Agents Chemother. 2007;51:4015–21. DOIPubMedGoogle Scholar
- Ribot EM, Fair MA, Gautom R, Cameron DN, Hunter SB, Swaminathan B, Standardization of pulsed-field gel electrophoresis protocols for the subtyping of Escherichia coli O157:H7, Salmonella, and Shigella for PulseNet. Foodborne Pathog Dis. 2006;3:59–67. DOIPubMedGoogle Scholar
- Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH, Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol. 1995;33:2233–9.PubMedGoogle Scholar
- Clinical Laboratory Standards Institute. Performance standards for antimicrobial disk susceptibility tests; approved standard—tenth edition. M02–A10. Wayne (PA): The Institute; 2009.
- Clinical Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; nineteenth informational supplement. M100–S19. Wayne (PA): The Institute; 2009.
- Blanco M, Alonso MP, Nicolas-Chanoine MH, Dahbi G, Mora A, Blanco JE, Molecular epidemiology of Escherichia coli producing extended-spectrum β-lactamases in Lugo (Spain): dissemination of clone O25b:H4–ST131 producing CTX-M-15. J Antimicrob Chemother. 2009;63:1135–41. DOIPubMedGoogle Scholar
- Manges AR, Tabor H, Tellis P, Vincent C, Tellier P-P. Endemic and epidemic lineages of Escherichia coli that cause urinary tract infections. Emerg Infect Dis. 2008;14:1575–83. DOIPubMedGoogle Scholar
- Dhanji H, Murphy NM, Doumith M, Durmus S, Lee SS, Hope R, Cephalosporin resistance mechanisms in Escherichia coli isolated from raw chicken imported into the UK. J Antimicrob Chemother. 2010;65:2534–7. DOIPubMedGoogle Scholar
- Mora A, Herrera A, Mamani R, López C, Alonso MP, Blanco JE, Recent emergence of clonal group O25b:K1:H4–B2-ST131 ibeA strains among Escherichia coli poultry isolates, including CTX-M-9producing strains, and comparison with clinical human isolates. Appl Environ Microbiol. 2010;76:6991–7. DOIPubMedGoogle Scholar
- Vincent C, Boerlin P, Daignault D, Dozois CM, Dutil L, Galanakis C, Food reservoir for Escherichia coli causing urinary tract infections. Emerg Infect Dis. 2010;16:88–95. DOIPubMedGoogle Scholar
- Platell JL, Cobbold RN, Johnson JR, Heisig A, Heisig P, Clabots C, Commonality among fluoroquinolone-resistant sequence type ST131 extraintestinal Escherichia coli isolates from humans and companion animals in Australia. Antimicrob Agents Chemother. 2011;55:3782–7. DOIPubMedGoogle Scholar
- Leflon-Guibout V, Blanco J, Amaqdouf K, Mora A, Guize L, Nicolas-Chanoine MH. Absence of CTX-M enzymes but high prevalence of clones, including clone ST131, among fecal Escherichia coli isolates from healthy subjects living in the area of Paris, France. J Clin Microbiol. 2008;46:3900–5. DOIPubMedGoogle Scholar
Figures
Tables
Cite This Article1MASTER (Macrorestriction Analysis of ST131 for Epidemiologic Research) Investigators who contributed data are listed at the end of this article.
Table of Contents – Volume 18, Number 4—April 2012
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
James R. Johnson, VA Medical Center, Infectious Diseases (111F), 1 Veterans Dr, Minneapolis, MN 55417, USA
Top