Volume 18, Number 9—September 2012
Dispatch
Multiple-Insecticide Resistance in Anopheles gambiae Mosquitoes, Southern Côte d’Ivoire
Abstract
Malaria control depends on mosquito susceptibility to insecticides. We tested Anopheles gambiae mosquitoes from Côte d’Ivoire for resistance and screened a subset for target site mutations. Mosquitoes were resistant to insecticides of all approved classes. Such complete resistance, which includes exceptionally strong phenotypes, presents a major threat to malaria control.
Targeting the mosquito vector is the most effective way to prevent malaria transmission; worldwide, this method accounts for more than half of malaria control expenditures (1,2). During the past decade, increased use of insecticide-treated bed nets and indoor residual spraying have made a pivotal contribution toward decreasing the number of malaria cases (1). However, these gains are threatened by the rapid development and spread of insecticide resistance among major malaria vectors in Africa (3). To keep vector resistance from undermining control programs, insecticide-resistance management strategies must reduce the current overreliance on pyrethroids. These compounds are used widely for indoor residual spraying and uniquely for insecticide-treated bed nets. However, having a limited number of insecticides available for malaria vector control restricts options for effective insecticide resistance management. Only 4 classes of insecticide, which share 2 modes of action, are approved by the World Health Organization (WHO).
A mutation at a single target site can result in mosquito resistance to DDT and pyrethroids or to organophosphates and carbamates. Furthermore, mosquitoes can express multiple insecticide-resistance mechanisms (4). For example, in several populations of the major malaria vector in Africa, Anopheles gambiae s.l. mosquitoes, mutations in the DDT/pyrethroid target site, known as knockdown resistance (kdr) alleles, have been found in conjunction with resistance alleles of the acetylcholinesterase gene (Ace-1R), the target site of organophosphates and carbamates (5). To date, however, these cases of multiple-insecticide resistance have been restricted by the relatively low prevalence of organophosphate/carbamate resistance and the limited effect that kdr mutations alone have on pyrethroid-based interventions (6). We report a population of An. gambiae mosquitoes from a rice-growing area of southern Côte d’Ivoire that have high frequencies of kdr and Ace-1R alleles and unprecedentedly high levels of phenotypic resistance to all insecticide classes available for malaria control.
During May–September 2011, mosquito larvae were collected in irrigated rice fields surrounding Tiassalé, southern Côte d’Ivoire (5°52′47′′N; 4°49′48′′W) and reared to adults in insectaries on a diet of MikroMin (Tetra, Melle, Germany) fish food. A total of 1,571 adult female An. gambiae s.l. mosquitoes, 3–5 days of age, were exposed to 1 of 5 insecticides (0.1% bendiocarb, 1.0% fenitrothion, 0.75% permethrin, 0.05% deltamethrin, 4% DDT) or a control papers for 1 hour, according to standard WHO procedures (7). Mosquito deaths were recorded 24 hours later. DNA was extracted from individual mosquitoes according to the LIVAK method (8), and a subsample of 500 mosquitoes were all found to be the M molecular form of An. gambiae s.s. by using the SINE-PCR method (9). The target site mutation G119S in the Ace-1 gene (Ace-1R) and L1014F and L1014S kdr mutations were screened by using restriction fragment length polymorphism (10) or TaqMan assays (11), respectively.
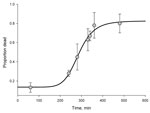
According to WHO criteria, An. gambiae mosquitoes from Tiassalé are resistant to all insecticide classes, and resistance is extremely prevalent; more than two thirds of mosquitoes survived the diagnostic dose for 4 of the 5 insecticides tested (Table 1). To assess the level of resistance, we exposed the Tiassalé population and a susceptible laboratory population of An. gambiae (Kisumu) mosquitoes to the pyrethroid deltamethrin or the carbamate bendiocarb for a range of exposure times and assessed deaths 24 hours later (Technical Appendix). We found an unexpectedly strong resistance phenotype to the 2 insecticides (Figure 1, Figure 2). For deltamethrin, 4 hours of exposure were required to kill 50% (median lethal time, [LT50]); in comparison, the LT50 for the susceptible Kisumu strain was <2 minutes (resistance ratio = 138) (Technical Appendix). Similarly, the LT50 for bendiocarb was nearly 5 hours for the Tiassalé strain yet <12 minutes for the susceptible strain (resistance ratio = 24) (Technical Appendix).
To investigate the causes of this resistance, we screened a subset of mosquitoes for the target site mutations, kdr 1014F and 1014S. Only the 1014F kdr mutation was detected, and this resistance allele was found at high frequency (83%). There was a significant association between presence of the 1014F kdr allele and ability to survive exposure to DDT but not to either pyrethroid (Table 2). In contrast, the Ace-1R allele was strongly associated with survival after exposure to bendiocarb and fenitrothion (Table 2).
Pyrethroid resistance in An. gambiae mosquitoes was first reported from Côte d’Ivoire in 1993 (12); carbamate resistance was detected in the 1990s (13). Nevertheless, ≈2 decades later, it is surprising and worrying to find complete resistance to all insecticides tested, particularly—for deltamethrin and bendiocarb—at such high levels. Resistance mechanisms seem to be varied. Ace-1R is strongly associated with organophosphate and carbamate resistance, and the absence of 119S homozygotes might be attributable to the high fitness cost of the Ace-1R allele in the absence of insecticide (14). Presence of the 1014F kdr allele alone does not confer the ability to survive diagnostic doses of pyrethroids; thus, alternative mechanisms must be responsible for the high-level pyrethroid resistance in this population.
The selective pressures responsible for this intense multiple-insecticide resistance in Tiassalé mosquitoes are unclear. There is a high coverage of insecticide-treated bed nets, but this coverage does not differ from that in other parts of the continent, and indoor residual spraying has not been conducted in this region. Use of insecticides in agriculture has been linked to resistance in malaria vectors. This use is perhaps the most likely explanation in this district of intense commercial production of rice, cocoa, and coffee.
Whatever the cause, the implications of this resistance scenario for malaria control are severe. With no new classes of insecticides for malaria control anticipated until 2020 at the earliest (15), program managers have few options available when confronted with multiple-insecticide resistance. Assessing the effect of pyrethroid resistance on the efficacy of insecticide-treated bed nets is complex because of the poorly understood associations between net integrity, insecticide content, net usage, and net efficacy. Nevertheless, resistance levels, such as those reported here, combined with continual selection pressure will inevitably lead to suboptimal mosquito control by use of insecticide-treated bed nets and indoor residual spraying. If unchecked, this resistance could spread rapidly and threaten the fragile gains that have been made in reducing malaria across Africa.
Mr Edi is a PhD student at the Liverpool School of Tropical Medicine. His research interests are the causes and consequences of insecticide resistance in malaria vectors.
Acknowledgments
We acknowledge Bassirou Bonfoh, Kesse Nestor, Assamoi Jean, Irie Liliane, Kouassi Loukou Bernard, Zahouli Julien, and Tra Benjamin for their technical assistance at the Centre Suisse de Recherches Scientifiques en Côte d’Ivoire and the populations and the authorities of Tiassalé for facilitating this study.
The research leading to these results was supported by the European Union Seventh Framework Programme FP7 (2007-2013) under grant agreement no. 265660 AvecNet. C.A.V.E. was sponsored by the European Union AvecNet project. D.W. was supported by the National Institutes of Health, National Institute of Allergy and Infectious Diseases, grant no. 1R01AI082734-01.
References
- World Health Organization. WHO Global Malaria Programme. World malaria report 2011. Geneva: The Organization; 2012. p. 30–3.
- Murray CJL, Rosenfeld LC, Lim SS, Andrews KG, Foreman KJ, Haring D, Global malaria mortality between 1980 and 2010: a systematic analysis. Lancet. 2012;379:413–31. DOIPubMedGoogle Scholar
- Ranson H, N’Guessan R, Lines J, Moiroux N, Nkuni Z, Corbel V. Pyrethroid resistance in African anopheline mosquitoes: what are the implications for malaria control? Trends Parasitol. 2011;27:91–8. DOIPubMedGoogle Scholar
- Perera MDB, Hemingway J, Karunaratne SP. Multiple insecticide resistance mechanisms involving metabolic changes and insensitive target sites selected in anopheline vectors of malaria in Sri Lanka. Malar J. 2008;7:168. DOIPubMedGoogle Scholar
- Yewhalaw D, Wassie F, Steurbaut W, Spanoghe P, Van Bortel W, Denis L, Multiple insecticide resistance: an impediment to insecticide-based malaria vector control program. PLoS ONE. 2011;6:e16066. DOIPubMedGoogle Scholar
- Hougard JM, Corbel V, N’Guessan R, Darriet F, Chandre F, Akogbéto M, and al. Efficacy of mosquito nets treated with insecticide mixtures or mosaics against insecticide resistant Anopheles gambiae and Culex quinquefasciatus (Diptera: Culicidae) in Côte d’Ivoire. Bull Entomol Res. 2003;93:491–8. DOIPubMedGoogle Scholar
- World Health Organization. Test procedures for insecticide resistance monitoring in malaria vectors, bio-efficacy and persistence of insecticide on treated surfaces. Geneva: The Organization, 1998.WHO/CDS/CPC/MAL/98.12.
- Livak KJ. Organization and mapping of a sequence on the Drosophila melanogaster X and Y chromosomes that is transcribed during spermatogenesis. Genetics. 1984;107:611–34.PubMedGoogle Scholar
- Santolamazza F, Mancini E, Simard F, Qi Y, Tu Z, della Torre A. Insertion polymorphisms of SINE200 retrotransposons within speciation islands of Anopheles gambiae molecular forms. Malar J. 2008;7:163. DOIPubMedGoogle Scholar
- Weill M, Malcolm C, Chandre F, Mogensen K, Berthomieu A, Marquine M, The unique mutation in ace-1 giving high insecticide resistance is easily detectable in mosquito vectors. Insect Mol Biol. 2004;13:1–7. DOIPubMedGoogle Scholar
- Bass C, Nikou D, Donnelly MJ, Williamson MS, Ranson H, Ball A, Detection of knockdown resistance (kdr) mutations in Anopheles gambiae: a comparison of two new high-throughput assays with existing methods. Malar J. 2007;6:111. DOIPubMedGoogle Scholar
- Elissa N, Mouchet J, Riviere F, Meunier JY, Yao K. Resistance of Anopheles gambiae s.s. to pyrethroids in Côte d’Ivoire. Ann Soc Belg Med Trop. 1993;73:291–4.PubMedGoogle Scholar
- N’Guessan R, Darriet F, Guillet P, Carnevale P, Traore-Lamizana M, Corbel V, Resistance to carbosulfan in Anopheles gambiae from Ivory Coast, based on reduced sensitivity of acetylcholinesterase. Med Vet Entomol. 2003;17:19–25. DOIPubMedGoogle Scholar
- Labbé P, Berthomieu A, Berticat C, Alout H, Raymond M, Lenormand T, Independent duplications of the acetylcholinesterase gene conferring insecticide resistance in the mosquito Culex pipiens. Mol Biol Evol. 2007;24:1056–67. DOIPubMedGoogle Scholar
- The Innovative Vector Control Consortium. IVCC develops new public health insecticides. 2010 Nov 22 [cited 2012 Feb 20]. http://www.ivcc.com/media/press_releases/ivcc_develops_new.htm
Figures
Tables
Cite This ArticleTable of Contents – Volume 18, Number 9—September 2012
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Hilary Ranson, Vector Group, Liverpool School of Tropical Medicine, Pembroke Place, Liverpool L3 5QA, UK
Top