Volume 19, Number 6—June 2013
Letter
Shewanella haliotis Associated with Severe Soft Tissue Infection, Thailand, 2012
To the Editor: Marine bacteria of the family Shewanellaceae, genus Shewanella, are gram-negative, motile bacilli that grow aerobically or anaerobically and produce hydrogen sulfide (1). Organisms belonging to a Shewanella species were first isolated in 1931 by Derby and Hammer from dairy products and classified as Achromobacter putrefaciens (2). Members of Shewanella species usually are found in marine environments in warm climates or during summer in temperate climates (3). In humans, most Shewanella species infections occur in skin and soft tissues (4). One species (S. algae) and possibly a second (S. putrefaciens) have been isolated from human samples on multiple occasions (5). A third species, S. haliotis, was implicated in human infections during 2010 (6) and S. xiamenensis was reported as the fourth infectious species among humans during 2011 (7). S. haliotis is a novel bacterial species that was isolated from the gut microflora of abalones (Haliotis discus hannai) in 2007 (8). We report the second description, to our knowledge, of S. haliotis involved in human disease.
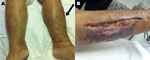
In September 2012, a 52-year-old woman, living in Bangkok, Thailand, was hospitalized after experiencing drowsiness for 2 hours. She had a low-grade fever, chills, and swelling, erythema, and tenderness in her left leg. During the previous week, she had handled fresh seafood in a market and had eaten cooked mackerel. She denied having eaten uncooked food or wading into flooded areas or the sea. She had undergone orthotopic liver transplantation 6 months previously to excise hepatocellular carcinoma related to Child-Pugh class C hepatitis C cirrhosis; since that procedure, she had been under treatment with immunosupressive drugs. She also had diabetes, hypertension, and nephrotic syndrome. Physical examination revealed that in addition to above-named symptoms, multiple blisters were noted (Figure, panel A). Her oral temperature was 37.8°C, blood pressure 80/40 mm Hg, pulse was 110 bpm, and respiratory rate was 24 breaths/minute. A complete blood count showed a leukocyte count of 2,250 cells/μL (91.2% neutrophils). Despite adequate rehydration, monitored by central venous pressure, the patient required norepinephrine to stabilize her vital signs. The clinical diagnosis of her condition was septic shock with suspected necrotizing fasciitis.
After tissue and blood samples were collected and submitted for microbiological analysis, shock resuscitation and an emergency fasciotomy (Figure, panel B) were performed, and antimicrobial drug treatment with meropenem and vancomycin was started. Surgeons did not confirm the suspected necrotizing fasciitis. Two sets of blood cultures and fluid culture sampled from the left leg identified S. algae by conventional biochemical methods. The MICs of antimicrobial drugs were determined by Etest (bioMérieux, Solna, Sweden). This strain was susceptible to ciprofloxacin (0.25 mg/L), piperacillin-tazobactam (1.0 mg/L), ceftriaxone (1.0 mg/L), and meropenem (0.38 mg/L). The patient had fever for the first 2 days of hospitalization. After 2 weeks of treatment, the antimicrobial drug was switched to oral ciprofloxacin; treatment was continued after dressing and debridement of the fasciotomy wound.
The organism produced yellowish-brown mucoid colonies on sheep blood agar and chocolate agar after 18 hours of incubation at 35°C under CO2 atmosphere. MacConkey agar showed non–lactose-fermenting colonies that were oxidase-positive, motile, and produced hydrogen sulfide on triple sugar iron agar. Growth at 42oC with 6.5% NaCl suggested that this organism was S. algae. Because phylogenetically related Shewanella species may be misidentified by routine biochemical tests, the strain was confirmed by using 16S rRNA gene sequencing.
Molecular characterization of 16S rRNA gene sequencing was performed by using PCR with Shewanella species consensus primers (Technical Appendix Table) and direct sequencing from PCR product (JX968803). Phylogenetic analysis of the 16S rRNA gene sequence showed clustering with S. haliotis (NR_044134T) and 99.9% similarity and 1 base difference (online Technical Appendix Figure). By using BLAST (http://blast.ncbi.nlm.nih.gov/Blast.cgi) analysis, JX968803 showed the closest match (99.9%; 1 base difference) with Alteromonadaceae bacterium PH39 (AF513471).
The strain was confirmed as S. haliotis by using additional biochemical tests and API 20 NE System (bioMérieux, Durham, NC, USA). It was positive for ornithine decarboxylase, gelatinase, reduction of nitrates to nitrites, tolerance to 6% NaCl, and assimilation of caprate and malate, but negative for citrate utilization, arginine dihydrolase, lysine decarboxylase, urease, indole production, assimilation of mannose, glucose, arabinose, mannitol, maltose, adipate, and acidification of glucose. This strain was resistant to polymyxin B (300 µg/disc).
More than 50 species of Shewanella have been reported. The route of Shewanella infection is associated with direct contact with the organism through seawater or ingestion of raw seafood (9). Japan reported 1 case of S. haliotis infection in an elderly patient in whom Vibrio vulnificus infection was initially suspected (6), and various clinical manifestations of S. algae infection have been reported (5). Community- and hospital-acquired infection with Shewanella species from contaminated medical devices have also been reported (10). S. haliotis and S. algae are closely related organisms; discriminating between them on the basis of biochemical tests is difficult. Molecular characterization of 16S rRNA gene sequencing can be used to differentiate the 2 species. In summary, this case suggests that immune-compromised persons in tropical climates could be susceptible to S. haliotis soft tissue infection in the absence of typical exposures.
Acknowledgments
We thank the staff of the Gastroenterology Unit, Department of Medicine, Liver Transplant Unit, Center of Excellence in Clinical Virology, Faculty of Medicine, Chulalongkorn University and Hospital, and the Thai Red Cross Society. We also thank Petra Hirsch for reviewing the manuscript.
This work was supported by the Higher Education Research Promotion and National Research University Project of Thailand, Office of the Higher Education Commission (HR1155), Thailand Research Fund (DPG5480002), Center of Excellence in Clinical Virology, Chulalongkorn University, Integrated Innovation Academic Center , Chulalongkorn University Centenary Academic Development Project (CU56-HR01), and King Chulalongkorn Memorial Hospital.
References
- Ivanova EP, Flavier S, Christen R. Phylogenetic relationships among marine Alteromonas-like proteobacteria: emended description of the family Alteromonadaceae and proposal of Pseudoalteromonadaceae fam. nov., Colwelliaceae fam. nov., Shewanellaceae fam. nov., Moritellaceae fam. nov., Ferrimonadaceae fam. nov., Idiomarinaceae fam. nov. and Psychromonadaceae fam. nov. Int J Syst Evol Microbiol. 2004;54:1773–88. DOIPubMedGoogle Scholar
- Derby HA, Hammer BW. Bacteriology of butter. IV. Bacteriological studies on surface taint butter. Iowa Agric Exp Station Res Bull. 1931;145:387–416.
- Holt HM, Gahrn-Hansen B, Bruun B. Shewanella algae and Shewanella putrefaciens: clinical and microbiological characteristics. Clin Microbiol Infect. 2005;11:347–52. DOIPubMedGoogle Scholar
- Goyal R, Kaur N, Thakur R. Human soft tissue infection by the emerging pathogen Shewanella algae. J Infect Dev Ctries. 2011;5:310–2. DOIPubMedGoogle Scholar
- Janda JM, Abbott SL. The genus Shewanella: from the briny depths below to human pathogen. Crit Rev Microbiol. 2012;10:1–21 and. DOIPubMedGoogle Scholar
- Tadera K, Shimonaka A, Ohkusu K, Morii D, Shimohana J, Michinaka T, A case report of Shewanella haliotis showing a phlegmonous inflammation of right lower leg with sepsis [in Japanese]. JSCM. 2010;20:239–44.
- Zong Z. Nosocomial peripancreatic infection associated with Shewanella xiamenensis. J Med Microbiol. 2011;60:1387–90. DOIPubMedGoogle Scholar
- Kim D, Baik KS, Kim MS, Jung BM, Shin TS, Chung GH, Shewanella haliotis sp. nov., isolated from the gut microflora of abalone, Haliotis discus hannai. Int J Syst Evol Microbiol. 2007;57:2926–31. DOIPubMedGoogle Scholar
- Myung DS, Jung YS, Kang SJ, Song YA, Park KH, Jung SI, Primary Shewanella algae bacteremia mimicking Vibrio septicemia. J Korean Med Sci. 2009;24:1192–4. DOIPubMedGoogle Scholar
- Oh HS, Kum KA, Kim EC, Lee HJ, Choe KW, Oh MD. Outbreak of Shewanella algae and Shewanella putrefaciens infections caused by a shared measuring cup in a general surgery unit in Korea. Infect Control Hosp Epidemiol. 2008;29:742–8. DOIPubMedGoogle Scholar
Figure
Cite This ArticleRelated Links
Table of Contents – Volume 19, Number 6—June 2013
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Yong Poovorawan, Center of Excellence in Clinical Virology, Department of Pediatrics, Faculty of Medicine, Chulalongkorn University, Bangkok 10330 Thailand
Top