Volume 20, Number 4—April 2014
Dispatch
Clinical Malaria along the China–Myanmar Border, Yunnan Province, China, January 2011–August 2012
Abstract
Passive surveillance for malaria cases was conducted in Yunnan Province, China, along the China–Myanmar border. Infection with Plasmodium vivax and P. falciparum protozoa accounted for 69% and 28% of the cases, respectively. Most patients were adult men. Cross-border travel into Myanmar was a key risk factor for P. falciparum malaria in China.
Increased global efforts to control and eliminate malaria are leading to substantial declines in malaria-related illness and death (1). Plasmodium vivax is the predominant malaria-causing species in China, followed by P. falciparum. Cross-border migration from Myanmar is suspected to be the major source for the introduction of P. falciparum malaria in southwestern China. During the past decade, the incidence of malaria in China has declined tremendously; the reduction in Myanmar has been less dramatic (1–5). To identify risk factors for clinical malaria and, in turn, to inform the ongoing malaria elimination programs in China, we conducted passive surveillance for malaria at health facilities along the China–Myanmar border in Yunnan Province, China, during January 2011–August 2012.
The Southeast Asia Malaria Research Center (www.niaid.nih.gov/LabsAndResources/resources/icemr/centers/Pages/southeastasia.aspx), an International Center of Excellence for Malaria Research, in collaboration with the Chinese Center for Disease Control and Prevention, conducted passive malaria case detection along the China–Myanmar border. Surveillance was conducted at 60 hospitals and health care centers in Tengchong, Yingjiang, Longchuan, and Ruili Counties in Yunnan Province, China. According to the Sixth National Population Census of the People's Republic of China conducted in 2010 (http://chinadatacenter.org/Announcement/AnnouncementContent.aspx?id=470), the population of the 4 counties totaled ≈1.5 million. During 2010, Ruili and Yingjiang Counties reported the highest incidence of malaria in China (2).
Persons who sought care for febrile illnesses at 1 of the 60 surveillance site hospitals or health care centers were screened for clinical signs and symptoms of malaria. Case report forms were used to collect the following information from patients: demographic characteristics, occupation, education level, clinical symptoms, history of malaria in the preceding 12 months, history of travel within the 2 weeks preceding the clinic visit, history of fever, and use of measures to prevent malaria. For each suspected case-patient, thick and thin blood smears were prepared and examined by 3 experienced microscopists to provide a final diagnosis and parasite densities. Patients were considered to have clinical malaria if they had signs and symptoms consistent with malaria and a plasmodium-positive blood smear; severe malaria was defined according to World Health Organization criteria (6).
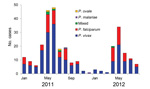
During January 2011–August 2012, a total of 8,296 Chinese and Myanmarese persons sought care for fever at the surveillance sites; 656 (7.9%) of the patients had other signs and symptoms consistent with malaria. Blood smear examination by microscope confirmed malaria infection in 303 (46.1%) of the 656 patients (Table 1). Protozoa of all 4 Plasmodium spp. that cause malaria in humans were detected; however, P. vivax and P. falciparum accounted for 69.0% and 27.7%, respectively, of the cases. Transmission peaked during April–July; cases of P. falciparum infection were detected primarily during the peak season (Figure). Asexual parasite densities were 1,285 and 2,515 parasites/μL, for P. vivax and P. falciparum, respectively. Chinese patients had fever for a median of 3.0 days, and Myanmarese patients (>90% of whom lived in China) had fever for a median of 2.5 days (range 1–10 days; p>0.05) before seeking care at a surveillance site. A total of 4 (1.9%) patients with P. vivax malaria and 13 (15.5%) patients with P. falciparum malaria had severe symptoms at the first clinical visit and were treated as inpatients.
A total of 84.4% of suspected and confirmed malaria case-patients in our passive case surveillance were Chinese. However, among patients with suspected malaria, Myanmarese patients were 2.5 times more likely than Chinese patients to have malaria (odds ratio [OR] 2.5, 95% CI 1.5%–4.1%; p<0.0001) (Table 1). Male patients were more likely than female patients to have malaria (OR 2.1, 95% CI 1.3%–3.5%; p<0.01), and most malaria case-patients were 18–60 years of age (OR 3.0, 95% CI 1.6%–5.3%; p<0.0001) (Table 1). Compared with persons who worked indoors (e.g., students, office workers, and housewives), persons who worked outdoors (e.g., construction workers, traders, truck drivers who traveled frequently, and farmers) were at higher risk for malaria (Table 1). Patients who reported using measures to prevent malaria (e.g., insecticide-treated nets and repellents) had a 14-fold lower odds of getting malaria than did patients who did not report using any preventive measures (OR 0.07, 95% CI 0.05%–0.10%; p<0.0001).
Among the 110 suspected malaria case-patients who reported travel during the 2 weeks before seeking care at a surveillance site, 54 were confirmed by blood-smear examination to have clinical malaria: 31 patients had P. vivax infections, 21 had P. falciparum infections, and 2 had mixed infections. After we adjusted for the confounding effects of age and sex, patients reporting travel across the border, >1 km into Myanmar, were 15 times more likely than nontravelers to have P. falciparum malaria (adjusted OR 15.0, 95% CI 2.9%–175.0%; p<0.001); however, travel into Myanmar was not significantly associated with P. vivax malaria (adjusted OR 1.9, 95% CI 0.8%–4.9%) (Table 2).
Most previous studies of malaria in China have analyzed case reports collected and reported by counties as a part of their routine health reporting system (3–5,7–10). Such information is prone to reporting bias and to underreporting (11,12). Furthermore, most publications implicating cross-border activity as a risk for malaria have not adequately delineated how migration and travel data were collected or how these variables were defined (2–4,8,10).
Our study has 2 major strengths: data were collected prospectively and the association with travel to Myanmar was determined on the basis of travel histories within the 2 weeks before study participants sought care at a surveillance site hospital or health center. Our observation that 44% of the febrile case-patients were female, although female patients comprised only 9% of the malaria case-patients, supports the association between occupation and cross-border travel and risk for malaria.
Despite recent reductions in the number of malaria cases in the border counties, our findings suggest that P. vivax malaria persists in areas of Yunnan Province along the China–Myanmar border, whereas cases of P. falciparum malaria are probably imported from Myanmar (8,13). Cross-border trade, logging, quarry and plantation activities, and construction in Myanmar may reintroduce P. falciparum parasite to Yunnan Province. Whether the findings from this surveillance system, which focused on the China–Myanmar border areas, can be extrapolated to a larger geographic region needs further validation. Future elimination efforts should focus on the effects of cross-border activities on malaria parasite transmission, and elimination efforts should include more intensive surveillance so that prevention and control activities can be directed at hot-spot regions along the China–Myanmar border.
Dr Zhou is an associate scientist in the Program of Public Health at the University of California, Irvine, Irvine, California, USA. His research focuses on ecological epidemiology of infectious disease and vector ecology.
Acknowledgments
We thank Jianhua Duan for field activity coordination and Malla Rao for constructive suggestions on the study design and data analysis. We are grateful to the communities and hospitals for their support and willingness to participate in this research.
This project was funded by grants from the National Institutes of Health (U19 AI089672 to L.C., G.Z., and G.Y.); the National Science Foundation of China (no. U1202226, 81161120421 and 31260508 to Z.Y.); the Ministry of Education of China (no. 20125317110001 to Z.Y.), and Yunnan Science Foundation (no. 2012FB153 to Z.X.).
References
- World Health Organization. World malaria report 2011. Geneva: The Organization; 2011.
- Zhou SS, Wang Y, Li Y. Malaria situation in the People’s Republic of China in 2010 [in Chinese]. Chin J Parasitol Parasitic Dis. 2011;29:401–3.
- Clements ACA, Barnett AG, Cheng ZW, Snow RW, Zhou HN. Space-time variation of malaria incidence in Yunnan Province, China. Malar J. 2009;8:180. DOIPubMedGoogle Scholar
- Lin H, Lu L, Tian L, Zhou S, Wu H, Bi Y, Spatial and temporal distribution of falciparum malaria in China. Malar J. 2009;8:130. DOIPubMedGoogle Scholar
- Hui FM, Xu B, Chen ZW, Cheng X, Lu L, Huang HB, Spatio-temporal distribution of malaria in Yunnan Province, China. Am J Trop Med Hyg. 2009;81:503–9.PubMedGoogle Scholar
- World Health Organization. Management of severe malaria: a practical handbook. 2nd ed. Geneva: The Organization; 2000.
- Chen GW, Li HX, Lin YX. Horizontal survey on the epidemiological characteristics of malaria in Laiza City of the second special administrative region of Kachin State of Myanmar, a China–Myanmar border area [in Chinese]. Chin J Vector Biol Control. 2012;23:352–6.
- Xia ZG, Yang MN, Zhou SS. Malaria situation in the People’s Republic of China in 2011 [in Chinese]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2012;30:419–22.
- Zhou SS, Wang Y, Xia ZG. Malaria situation in the People’s Republic of China in 2009 [in Chinese]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2011;29:1–3.
- Li HX, Chen GW, Yang YC, Jiang H. Malaria situation in Yunnan Province during 2001–2005 [in Chinese]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2008;26:46–9.
- Zhou SS, Tang LH, Sheng HF. Malaria situation in the People’s Republic of China in 2003 [in Chinese]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2005;23:385–87.
- Sheng HF, Zhou SS, Gu ZC, Zheng X. Malaria situation in the People’s Republic of China in 2002 [in Chinese]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2003;21:193–6.
- Bi Y, Hu W, Yang H, Zhou XN, Yu W, Guo Y, Spatial patterns of malaria reported deaths in Yunnan Province, China. Am J Trop Med Hyg. 2013;88:526–35. DOIPubMedGoogle Scholar
Figure
Tables
Cite This Article1These authors contributed equally to this article.
Table of Contents – Volume 20, Number 4—April 2014
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Guiyun Yan, Program in Public Health, University of California, Irvine, Irvine, CA 92697, USA; , , orGuiyun Yan, Program in Public Health, University of California, Irvine, Irvine, CA 92697, USA; , , or
Top