Volume 21, Number 2—February 2015
CME ACTIVITY - Research
Infectious Causes of Encephalitis and Meningoencephalitis in Thailand, 2003–2005
Introduction

Medscape, LLC is pleased to provide online continuing medical education (CME) for this journal article, allowing clinicians the opportunity to earn CME credit.
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education through the joint providership of Medscape, LLC and Emerging Infectious Diseases. Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)TM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 75% minimum passing score and complete the evaluation at http://www.medscape.org/journal/eid; (4) view/print certificate.
Release date: January 15, 2015; Expiration date: January 15, 2016
Learning Objectives
Upon completion of this activity, participants will be able to:
• Distinguish the prevalence of abnormal ancillary testing results among patients with encephalitis
• Assess demographic and clinical characteristics of patients with encephalitis
• Discuss the rate of confirmed or probable etiology of encephalitis in the current study
• Identify the most common causative organism associated with encephalitis in the current study.
CME Editor
P. Lynne Stockton, VMD, MS, ELS(D), Technical Writer/Editor, Emerging Infectious Diseases. Disclosure: P. Lynne Stockton, VMD, MS, ELS(D), has disclosed no relevant financial relationships.
CME Author
Charles P. Vega, MD, Clinical Professor of Family Medicine, University of California, Irvine. Disclosure: Charles P. Vega, MD, has disclosed the following financial relationships: served as an advisor or consultant for McNeil Pharmaceuticals.
Authors
Disclosures: Sonja J. Olsen, PhD; Angela P. Campbell, MD, MPH; Krongkaew Supawat, MSc; Sahas Liamsuwan, MD; Tawee Chotpitayasunondh, MD; Somsak Laptikultham, MD, FRCP; Akravudh Viriyavejakul, MD; Supoch Tunlayadechanont, MD; Anannit Visudtibhan, MD; Punnee Vasiknanonte, MD; Supachai Janjindamai, MD; Pairoj Boonluksiri, MD; Kiatsak Rajborirug, MD; Veerachai Watanaveeradej, MD; Nino Khetsuriani, MD, PhD; and Scott F. Dowell, MD, MPH, have disclosed no relevant financial relationships. Tasanee Tantirittisak, MD, has disclosed the following relevant financial relationships: served as a speaker or member of a speakers bureau for Lundbeck.
Abstract
Acute encephalitis is a severe neurologic syndrome. Determining etiology from among ≈100 possible agents is difficult. To identify infectious etiologies of encephalitis in Thailand, we conducted surveillance in 7 hospitals during July 2003–August 2005 and selected patients with acute onset of brain dysfunction with fever or hypothermia and with abnormalities seen on neuroimages or electroencephalograms or with cerebrospinal fluid pleocytosis. Blood and cerebrospinal fluid were tested for >30 pathogens. Among 149 case-patients, median age was 12 (range 0–83) years, 84 (56%) were male, and 15 (10%) died. Etiology was confirmed or probable for 54 (36%) and possible or unknown for 95 (64%). Among confirmed or probable etiologies, the leading pathogens were Japanese encephalitis virus, enteroviruses, and Orientia tsutsugamushi. No samples were positive for chikungunya, Nipah, or West Nile viruses; Bartonella henselae; or malaria parasites. Although a broad range of infectious agents was identified, the etiology of most cases remains unknown.
Acute encephalitis is a severe neurologic syndrome that is often associated with substantial illness and death. It can be caused by any of ≈100 infectious agents that vary by geographic region. Among leading known causes of encephalitis in the United States and worldwide are arthropodborne viruses (arboviruses) and herpesviruses (1–9). Data on encephalitis in Southeast Asia are limited, but previous studies have identified Japanese encephalitis virus (JEV) and herpesviruses as common causes (10–12). Dengue virus has also been associated with encephalopathy and other neurologic findings (4,13–15). Over the past decade, several viral encephalitides have emerged in Southeast Asia, including Nipah virus and enterovirus 71, and led to unexpected outbreaks of neurologic disease (4,16–23).
Determining the etiology of encephalitis is difficult. The definition varies, and distinguishing the neurologic syndrome of encephalitis from meningoencephalitis or even meningitis or encephalopathy can be challenging (24,25). In recent studies, the etiology for most cases was not determined despite extensive testing (1,6–12,26). One characteristic of past studies is that laboratory diagnosis for encephalitis was often not complete because of lack of available diagnostics, limited scope of pathogens studied, or difficulty obtaining adequate specimens. Detection capabilities are limited by testing for only a limited core battery of pathogens or the most likely pathogens on the basis of exposure history and clinical information and by use of conventional diagnostics.
To determine the spectrum of encephalitis etiologic agents in Thailand, we conducted a prospective study and used an expanded testing approach. We used a case definition consistent with definitions used in prior studies, requiring acute brain dysfunction and evidence of inflammation and including patients who also had meningeal inflammation with an encephalitic component (meningoencephalitis) (1,10,12). We sought to identify etiologic pathogens for patients with a clinical syndrome consistent with encephalitis and meningoencephalitis and to describe the clinical features and outcomes associated with different causes.
Study Sites
Patients were recruited from 7 hospitals in Thailand: 5 in Bangkok (Queen Sirikit National Institute of Child Health, Rajvithi Hospital, Prasat Neurologic Institute, Ramathibodi Hospital, and Phramongkutkao Hospital) and 2 in the southern city of Hat Yai (Hat Yai Hospital, Prince Songkhla University Hospital). The main study physicians in each hospital were specialists in neurology or infectious diseases. During July 2003–August 2005, physicians identified potential study participants who met eligibility criteria and referred them to a study nurse, who obtained written informed consent. The protocol was approved by an institutional review board at the Centers for Disease Control and Prevention (CDC) and the Thailand Ministry of Public Health.
Enrollment Criteria and Case Definition
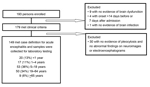
Enrollment criteria for patients of any age included all of the following: 1) acute brain dysfunction requiring hospitalization (new encephalopathy [i.e., altered mental status with or without lethargy], new onset of diffuse or focal central neurologic findings, or new onset of seizures); 2) acute onset of brain dysfunction within 14 days before or 7 days after admission to a study hospital; 3) documented fever (>38°C), history of fever, or hypothermia (<35°C); and 4) clinical indication for lumbar puncture as determined by the patient’s physician. After enrollment, participants were required to meet at least 1 of the following 3 criteria to meet the case definition of acute encephalitis or meningoencephalitis: 1) abnormal findings consistent with encephalitis seen on neuroimages obtained by computed tomography (CT) scan, magnetic resonance imaging (MRI), or cranial ultrasonography; 2) abnormal findings on electroencephalogram (EEG) consistent with encephalitis; or 3) cerebrospinal fluid (CSF) pleocytosis (>15 leukocytes/mm3 for infants <6 weeks of age and >5 leukocytes/mm3 for patients >6 weeks of age). Patients found to have an alternative confirmed diagnosis before discharge that explained their signs and symptoms (e.g., metabolic encephalopathy) were excluded from further study.
Epidemiologic Data and Specimen Collection
For each patient, study physicians completed standardized admission and discharge surveys documenting medical history, signs and symptoms, and neuroimaging and EEG results. Research nurses completed an extensive questionnaire about demographics, medical and exposure history, and laboratory results. Study nurses completed a follow-up questionnaire during each patient’s convalescent-phase visit 3–6 weeks after enrollment. The following specimens were collected: CSF (up to 6.5 mL); acute- and convalescent-phase blood (12.5–22.5 mL from children <5 years of age and 25.5 mL from all others); and oropharyngeal swab, saliva (0.7 mL), urine (10 mL), and fecal (10–20 g) specimens.
Specimen Handling, Storage, and Testing
Specimens were tested for the presence of >30 pathogens (Table 1). After collection, specimens were immediately separated into portions for clinical testing at hospitals and research testing at reference laboratories (Technical Appendix). Within 24 hours of collection, specimens destined for reference laboratories were aliquoted for distribution to >20 laboratories at the Thailand National Institute of Health and CDC. Any specimens that could not be aliquoted within 24 hours were stored at −20°C and then at −70°C after aliquoting. Specimens from Hat Yai were transported on dry ice to Bangkok every 2–4 weeks. If CSF or serum sample volume was limited, the order of specimen testing was prioritized (Technical Appendix).
Etiologic Classification
Definitions were created to define the etiologic link between identified pathogens and encephalitis; the etiology for each case was classified as confirmed, probable, possible, or unknown (Table 1). Each case could be assigned >1 etiology. The classification system considered the nature of an agent (well-established cause of encephalitis or not) and etiologic significance of a given positive laboratory test result.
Etiology was considered confirmed for cases with positive results for PCR, culture, antigen, or pathogen-specific IgM in CSF for a pathogen considered to be a well-established cause of encephalitis. For arboviruses commonly associated with encephalitis (i.e., JEV or West Nile virus), documentation of acute infection in paired serum samples was considered the diagnostic standard and therefore was considered confirmatory.
Etiology was considered probable for cases with positive results that were strongly suggestive but not considered confirmatory and not clearly established as diagnostic for encephalitis in all situations or cases for which a pathogen not generally established as a cause of encephalitis was detected in CSF. For example, etiology would be considered probable if PCR of CSF was positive for lymphotropic agents (e.g., cytomegalovirus, Epstein-Barr virus [EBV]) or if serum testing results provided evidence of acute infection for pathogens known to be associated with encephalitis, such as Orientia tsutsugamushi, Bartonella henselae, and Mycoplasma pneumoniae.
Etiology was considered possible for cases with no laboratory evidence of CNS involvement but some evidence of acute infection that suggested a potential etiologic role in encephalitis, such as a >4-fold rise in antibody titer for enteroviruses or an oropharyngeal swab sample positive for influenza or parainfluenza viruses. In addition, etiology was considered possible for cases for which information to determine etiology of encephalitis (e.g., human adenoviruses 40 and 41) was insufficient, even if detected in CSF (27). Etiology was considered unknown for cases for which all testing results were negative.
In an effort to differentiate between cases of encephalitis and meningoencephalitis, we defined a subset of patients who met the case definition and specifically had CSF pleocytosis and stiff neck as having meningoencephalitis. To provide a complete description of all patients who met the case definition, we retained the 8 patients for whom a sole confirmed bacterial agent commonly associated with bacterial meningitis was found. Pertinent analyses were performed with and without these 8 patients. For 1 patient for whom a bacterial etiology was confirmed, a viral etiology (JEV) was also confirmed; thus, this patient was not excluded from either analysis.
Statistical Analyses
We present descriptive data with case counts and frequencies. We used the Wilcoxon rank-sum test to compare continuous variables between the confirmed/probable and possible/unknown etiologic groups. The prevalence of categorical variables was compared by using χ2 analysis or the Fisher exact test. We considered 2-sided p values <0.05 to be statistically significant. Statistical analyses were performed by using SPSS Statistics for Windows version 21.0 (IBM Corp., Armonk, NY, USA).
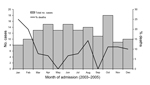
We enrolled 193 patients, among whom 149 (77%) met the case definition for acute encephalitis (Figure 1). Of the 149 acute encephalitis patients, CSF pleocytosis was found for 125 (84%), abnormal neuroimages for 80 (54%) (45 brain MRI, 55 brain CT, 6 cranial ultrasonography), and EEG findings consistent with encephalitis (categories not mutually exclusive) for 28 (19%). Of the 149 patients, 84 (56%) were male and median age was 12 (range 0–83) years. A median of 5 patients were admitted each month, varying somewhat by season (Figure 2). A total of 30 (20%) patients were from Songkhla; 73 (49%) reported having lived in a city or town in the past 3 months. Median time between onset of neurologic symptoms and admission was 1 day (range 12 days before admission to 7 days after), and median length of hospital stay was 15 (range 1–180) days. A total of 22 (15%) patients had an underlying condition (e.g., HIV infection, malignancy, diabetes mellitus). Of 3 main antimicrobial treatments given empirically during hospitalization, acyclovir was given to 62 (42%) patients; a third- or fourth-generation cephalosporin to 97 (65%), 16 of whom also received a carbapenem; doxycycline to 10 (7%); at least 1 of these drugs to 122 (82%); and all 3 drugs to 4 (3%). A total of 15 (10%) patients died.
With regard to hospital testing, blood culture was performed for 129 (87%), CSF culture for 141 (95%), and both cultures for 123 (83%). Growth occurred on 21 (16%) blood cultures and 19 (13%) CSF cultures (Table 2); pathogens grew on both cultures for 7 patients. No patients had positive malaria testing results, and 8 (5.4%) had positive HIV results.
For most patients, specimens were available for additional testing at the reference laboratories (Thailand National Institute of Health and CDC). CSF specimens were available for 147 (99%) (median 3.1, range 0.8–13 mL), acute-phase serum for 145 (97%) and convalescent-phase serum for 129 (87%) (median time between sample collection 24 [range 14–39] days), oropharyngeal swab samples for 141 (95%), saliva for 138 (93%), feces for 119 (80%), and urine for 143 (96%) patients.
Case Designation by Etiologic Classification
Of the 149 cases, etiology was confirmed for 37 (25%), probable for 17 (11%), possible for 44 (30%), and unknown for 51 (34%) (Table 3). Among confirmed etiologies, JEV was identified in 15 patients and dengue virus in 2. In >1 patient, infection with the following was also identified: enteroviruses (n = 6), Cryptococcus spp. (n = 3), Haemophilus influenzae (n = 3), Streptococcus pneumoniae (n = 3), and varicella-zoster virus (VZV; n = 2). Among case-patients whose illness met the definition for confirmed etiology, a bacterial pathogen commonly associated with meningitis was confirmed for 8 patients (H. influenzae for 3, S. pneumoniae for 3, Neisseria meningitidis for 1, and Escherichia coli for 1).
Among patients for whom etiology was probable, O. tsutsugamushi, which causes scrub typhus, was found in 6 patients (5 became ill while in central Thailand and were hospitalized in Bangkok); JEV in 6, EBV in 3 (concurrent with Cryptococcus spp. in 1 and VZV in 1); M. pneumoniae in 3; and Rickettsia conorii, which causes spotted fever, in 3 patients. Among the 54 patients for whom etiology was confirmed/probable, a potentially treatable pathogen was identified for 25 (46%) (C. neoformans, E. coli, herpes simplex virus, H. influenzae, influenza viruses, M. pneumoniae, N. meningitidis, O. tsutsugamushi, R. conorii, S. pneumoniae, and Treponema pallidum). We did not include the patient with confirmed JEV and Salmonella group D infection in the treatable category.
Among the 98 patients for whom at least 1 pathogen was identified, a total of 156 pathogens were detected (Table 3); of 40 (41%) patients for whom >1 pathogen was detected, etiology was classified as possible for most. Of the 54 patients for whom etiology was confirmed/probable, >1 pathogen was classified as confirmed/probable for 6 (11%): (JEV/O. tsutsugamushi/R. conorii, JEV/R. conorii, JEV/Salmonella, Cryptococcus spp./EBV, VZV/EBV, VZV/influenza virus), whereas at least 1 possible etiology was also detected for 28 (52%) (p<0.01). Of 44 patients for whom a possible etiology was identified, >1 possible pathogen was detected for 12 (27%).
Of the 149 patients, 68 (46%) met the definition for meningoencephalitis; for 38 (56%) of these patients, EEG or neuroimaging findings were abnormal, consistent with encephalitis. Of these 38 patients, pathogens considered confirmed/probable etiologic agents were detected for 12 (32%): JEV for 8 (also R. conorii for 2 and O. tsutsugamushi for 1), Cryptococcus for 2, M. pneumoniae for 1, and R. conorii for 1. Of the 30 remaining patients, pathogens that conferred a confirmed/probable etiologic classification were detected for 16 (53%): JEV for 6, O. tsutsugamushi for 4, enterovirus for 3, N. meningitidis for 1, herpes simplex virus 1/2 (not distinguished) for 1, and VZV/EBV (positive for both) for 1.
At admission, very few demographic and clinical differences between those with confirmed/probable and possible/unknown etiologies were found (Table 4). Among patients for whom etiology was confirmed/probable, median temperature was higher, loss of consciousness was less common, and stiff neck was more common. When the 8 patients with bacterial meningitis were excluded from analysis, patients for whom etiology was confirmed/probable had a higher median temperature than those for whom etiology was possible/unknown (37.9 vs. 37.7, p = 0.04) and were more likely to have a stiff neck (54% vs. 31%, p = 0.01). Among the 54 patients for whom etiology was confirmed or probable, no differences were found for demographic characteristics and only 1 difference was found for clinical characteristics at admission (Table 4) between those for whom etiology was or was not treatable; temperature was lower among those for whom etiology was treatable (37.9 vs. 39, p<0.01).
Outcomes
A total of 15 (10%) patients died. The mortality rate was lower, but not significantly, among patients for whom etiology was confirmed/probable than for those for whom etiology was possible/unknown (3.9% vs. 14%, p = 0.09; Table 4). When the 8 patients for whom only a confirmed bacterial etiology was found were excluded from analysis, this difference was similar (4.3% vs. 14%, p = 0.14). Among those who died, etiology was confirmed for 2 (Cryptococcus spp. in a 5-year-old boy and VZV in a 51-year-old HIV-infected woman). Among those who died, 9 (60%) were male and the median age was 34 years of age (1 was <1 year, 1 was 1–4 years, 4 were 5–18 years, 8 were 19–64 years, and 1 was ≥65 years). The median interval between hospital admission and death (or discharge for survivors) was 6 days (vs. 16 days to discharge, p = 0.3), between onset of neurologic symptoms and death was 10 days (vs. 18.5 days to discharge, p = 0.3), and between fever onset and death was 10 days (vs. 20 to discharge, p = 0.2). Among the 134 patients who survived, 43 (32%) remained hospitalized at the time of the convalescent-phase interview, 86 (64%) had returned home, and 5 (3.7%) were lost to follow-up; 5 patients had a seizure after discharge. Of the 86 persons who returned home, 52 (60%) reported complete cognitive recovery; of these, 45 (87%) of these functioned independently or at the same level of care as before hospitalization.
In Thailand, a wide range of pathogens cause acute encephalitis. In this study, by using a comprehensive approach and advanced diagnostic methods, we identified a confirmed/probable etiology for only 36% of 149 patients, and >1 confirmed/probable pathogen was detected for 11% of these patients. Detection of possible pathogens was so common as to make interpretation challenging. Ten percent of patients died; highest mortality rate was among patients for whom etiology was classified as possible/unknown.
In our study, the most frequently identified pathogen (39% of all confirmed/probable etiologies) was JEV, which is endemic to Thailand; routine infant vaccination was introduced in 2001 (28). JEV data from our study have been published (29). Among patients for whom etiology was confirmed/probable, the etiologic pathogen was potentially treatable for 48%. Most of these 12 treatable pathogens, except herpes simplex virus, influenza viruses, M. pneumoniae, O. tsutsugamushi, and R. conorii, can be diagnosed in the study hospital laboratories in Thailand through routine CSF and blood culture, Venereal Disease Research Laboratory testing, or rapid antigen tests of CSF. The clinical features did not enable differentiation of specific etiologic agents. For many patients, a standard empiric treatment regimen consisting of a third- or fourth-generation cephalosporin, acyclovir, and doxycycline might be appropriate. The national reference laboratory in Thailand is able to test for all confirmed/probable etiologic agents.
This study highlights the clinical overlap between encephalitis and meningoencephalitis. Almost half of the patients met the definition for meningoencephalitis, yet for half of those patients, abnormalities detected by EEG or neuroimaging were consistent with encephalitis, and their illnesses were associated with a range of pathogens, some not typically associated with meningitis. Furthermore, we found that patients whose meningitis was caused by common bacteria, such as S. pneumoniae or H. influenzae, sometimes met the case definition but did not meet the criteria for meningoencephalitis (pleocytosis and stiff neck). We reported laboratory results for all patients who met the encephalitis case definition, and we also repeated the analyses excluding the 8 patients with only a confirmed etiology of bacteria commonly associated with meningitis, which minimally affected the results. It could be argued that including pleocytosis in the case definition may have resulted in a predilection for enrolling patients with meningoencephalitis and/or meningitis; however, pleocytosis has commonly been included in the case definition for studies of encephalitis (24), and including it was necessary for our study because we were uncertain whether neuroimaging would be routinely performed.
Several pathogens that cause encephalitis were notably absent, including chikungunya, Nipah, and West Nile viruses; B. henselae; and malaria parasites. B. henselae infection occurs in Thailand, although it has not been widely studied (30). Because of extensive vector control efforts in Thailand, malaria parasite transmission is limited to areas along Thailand’s borders with Burma and Cambodia, so it was not surprising that no cases of malaria were identified in Bangkok and Songkhla (31). Nipah virus has caused outbreaks of encephalitis in humans in Malaysia and Bangladesh; although it has been found in bats in Thailand, it has not yet been identified in humans (32,33). West Nile virus has also not yet been identified in Thailand.
Enteroviruses were found in CSF of 6 children 3 months to 10 years of age. Enteroviruses commonly cause aseptic meningitis and have also been clearly demonstrated to cause encephalitis. In Asia, epidemics of enterovirus 71 infection causing severe central nervous disease have occurred (34); however, enterovirus 71 was not detected in the CSF of any patient in our study. Consistent with reports in the literature, we found 2 cases of dengue virus infection (35). We found 6 cases of infection with O. tsutsugamushi, the etiologic agent of scrub typhus, which is prevalent in Southeast Asia although not thought to be common in Bangkok. Thus, the fact that 5 patients became ill while in central Thailand suggests that physicians should consider this pathogen in areas outside the known disease-endemic southern provinces. Most cases of scrub typhus, and spotted fever caused by R. conorii (which we identified in 3 patients), can be treated effectively with doxycycline (36). Unfortunately, most hospital laboratories do not routinely perform diagnostic serologic testing for these infections, so they might often not be suspected unless a prominent eschar or rash is visible. EBV was found in the CSF of 3 patients, concomitant with another pathogen for 2 patients. In these cases, EBV detection probably represented reactivation of latent EBV in the setting of a primary central nervous system infectious agent (37). Three cases of encephalitis were associated with M. pneumoniae, all in children 6–14 years of age, consistent with other study findings (38,39).
Comprehensive etiologic studies present many challenges and have limitations. In this study, CSF diagnostics were the most compelling approach for identifying an etiology; yet in some patients, CSF or other specimens were inadequate for complete testing for all agents. We used consensus primers to detect herpesviruses by PCR, but this method is probably less sensitive than one that uses specific primers for each herpesvirus. Feces and oropharyngeal swabs samples were not tested for enteroviruses, but these samples can be more likely to yield this pathogen. Last, we did not investigate noninfectious forms of encephalitis, such as anti–N-methyl-D-aspartate receptor and voltage-gated potassium channel antibody encephalitis, which have been shown in recent studies to cause encephalitis with poor outcomes (7,40).
Encephalitis is a severe disease that can cause substantial illness and death. Despite the high proportion of patients for whom large volumes of CSF and acute- and late convalescent–phase serum were tested and a broad range of routine and sophisticated diagnostic testing was performed, the etiology for one-third of the patients remained unknown and for another one-third was classified only as possible. The proportion of cases for which etiology was unknown in this study was slightly lower than that in other studies, perhaps because so many diagnostic tests were used (1,10–12,26). Because laboratory testing was performed simultaneously rather than sequentially, testing bias was reduced; however, because of multiple positive results, the complexity of interpretation was increased.
Although Thailand is a middle-income country with trained neurologists and more sophisticated medical and laboratory tools for diagnosing encephalitis than are found in many other countries in Southeast Asia, it still lacks the ability to routinely identify major causes of encephalitis. This study highlights the continuing role of Japanese encephalitis and other potentially preventable or treatable diseases in Thailand, such as those caused by the rickettsiae O. tsutsugamushi and R. conorii. Despite intensive efforts to diagnose cases, this study also emphasizes the need for improved diagnostic strategies and geographically appropriate clinical testing algorithms for adults and children with encephalitis in Southeast Asia. Such strategies and algorithms were recently presented by the International Encephalitis Consortium (24) to provide a standardized approach for the evaluation of patients suspected of having encephalitis. Such an approach will facilitate worldwide research collaboration and enable clinicians to provide appropriate clinical care for patients with this severe and often devastating neurologic syndrome.
Dr. Olsen is an epidemiologist with the US CDC; her research interests are infectious disease issues of importance to Southeast Asia and the global public health community. Dr Campbell is a pediatric infectious disease physician and medical epidemiologist at US CDC; her research focuses on studies of influenza antiviral treatment and antiviral effectiveness, and she develops CDC clinical guidance related to treatment and prevention of seasonal and novel influenza viruses.
Acknowledgments
We gratefully acknowledge Sirinya Somsaen, Patsada Somkuntod, and Pakaymas Kittiwittayakul for assistance with data collection; Saithip Sutthirattana for assistance with coordination; Mark Simmerman for assistance with logistics; Pongpun Sawatwong for assistance with laboratory results; Prasong Srisaengchai for assistance merging the databases; and Robert Breiman for providing advice on the study approach. In addition, we acknowledge the support and assistance of the case-patients, their family members, and all hospital and laboratory personnel who participated in this study. We also thank Michael Dillon for specimen management across CDC laboratories.
This study was supported by funding from the US CDC.
Members of the Thailand Encephalitis Surveillance Team: Sununta Henchaichon, Khanchit Limpakarnjanarat (International Emerging Infections Program, Thailand Ministry of Public Health [MOPH]–US CDC Collaboration, Nonthaburi, Thailand); Pathom Sawanpanyalert, Yaowapa Pongsuwanna, Rungrueng Kijphati, Surang Dejsirilert, Pranee Thawatsupha, Surapee Anantapreecha, Sirima Pattamadilok, Mongkol Chenchittikul, Wattanapong Wootha (Thailand National Institutes of Health, Thailand MOPH, Nonthaburi); Surapee Ruangsuwan (Queen Sirikit National Institute of Child Health, Bangkok, Thailand); Surawit Techatuwanan (Rajvithi Hospital, Bangkok); Apirom Watchaputi, Pathra Angsuwan, Kanlaya Dhiravibulya, Apasri Lusawat, Maiyadhaj Samsen (Prasat Neurological Institute of Thailand, Bangkok); Rawiphan Witoonpanich, Surang Chiemchanya (Ramathibodi Hospital, Mahidol University, Bangkok); Kamol Veerapradist, Weerapatn Ngaothamatasn, Boonyarat Warachit, Soonthorn Peeraputhi, Jareerat Yodsawat (Hat Yai Hospital, Hat Yai, Thailand); Sutham Pinjaroen, Pornchai Sathirapanya, Suwanna Setthawatcharawanich, Prasit Ruengrairattanaroj (Prince Songkhla University Hospital, Hat Yai); Charcrin Nabangchang, Danabhand Phiboonbanakit (Phramongkutklao Hospital, Bangkok); Joe Bresee, Jairam Lingappa, Mark Pallansch, M. Steven Oberste, Dean Erdman, William J. Bellini, Paul Rota, Suxiang Tong, D. Scott Schmid, Vladimir Loparev, Gregory Dasch, Lyle Petersen, Anthony A. Marfin, Grant L. Campbell, Ann Powers, Susan Montgomery, Marc Fischer, Janeen Laven, Olga Kosoy, Amanda Panella, Christine Ellis, Leonard Mayer, Peter Dull, Anne Whitney, Barry Fields, Deborah Talkington, Lanier Thacker, James Maguire, Thomas Ksiazek, James A. Comer, Alexander Klimov, Tim Uyeki, Stephen Lindstrom, Nancy Cox, Alison Siwek, Janine Douglass, Suzette Bartley (US CDC); Charles E. Rupprecht (The Global Alliance for Rabies Control; Ross University School of Veterinary Medicine, St. Kitts, West Indies).
References
- Glaser CA, Gilliam S, Schnurr D. Forghani B, Honarmand S, Khetsuriani N, et al. In search of encephalitis etiologies: diagnostic challenges in the California Encephalitis Project, 1998–2000. Clin Infect Dis. 2003;36:731–42. PMID: 12627357
- Solomon T. Exotic and emerging viral encephalitides. Curr Opin Neurol. 2003;16:411–8 . DOIPubMedGoogle Scholar
- Whitley RJ, Gnann JW. Viral encephalitis: familiar infections and emerging pathogens. Lancet. 2002;359:507–13. DOIPubMedGoogle Scholar
- Mailles A, Stahl JP. Infectious encephalitis in France in 2007: a national prospective study. Clin Infect Dis. 2009;49:1838–47. DOIPubMedGoogle Scholar
- Granerod J, Ambrose HE, Davies NW. Clewley JP, Walsh AL, Morgan D, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010;10:835–44.
- Ho Dang Trung N, Le Thi Phuong T, Wolbers M. Nguyen Van Minh H, Nguyen Thanh V, Van MP, et al. Aetiologies of central nervous system infection in Viet Nam: a prospective provincial hospital-based descriptive surveillance study. PLoS ONE. 2012;7:e37825.
- Chokephaibulkit K, Kankirawatana P, Apintanapong S. Pongthapisit V, Yoksan S, Kositanont U, et al. Viral etiologies of encephalitis in Thai children. Pediatr Infect Dis J. 2001;20:216–8.
- Cam BV, Fonsmark L, Hue NB, Phuong NT, Poulsen A, Heegaard ED. Prospective case–control study of encephalopathy in children with dengue hemorrhagic fever. Am J Trop Med Hyg. 2001;65:848–51 .PubMedGoogle Scholar
- Kankirawatana P, Chokephaibulkit K, Puthavathana P, Yoksan S, Apintanapong S, Pongthapisit V. Dengue infection presenting with central nervous system manifestation. J Child Neurol. 2000;15:544–7. DOIPubMedGoogle Scholar
- Solomon T, Dung NM, Vaughn DW. Kneen R, Thao LT, Raengsakulrach B, et al. Neurological manifestations of dengue infection. Lancet. 2000;355:1053–9.
- Lam SK, Chua KB. Nipah virus encephalitis outbreak in Malaysia. Clin Infect Dis. 2002;34(Suppl 2):S48–51. DOIPubMedGoogle Scholar
- Chan KP, Goh KT, Chong CY, Teo ES, Lau G, Ling AE. Epidemic hand, foot and mouth disease caused by human enterovirus 71, Singapore. Emerg Infect Dis. 2003;9:78–85. DOIPubMedGoogle Scholar
- Rao BL, Basu A, Wairagkar NS. Gore MM, Arankalle VA, Thakare JP, et al. A large outbreak of acute encephalitis with high fatality rate in children in Andhra Pradesh, India, in 2003, associated with Chandipura virus. Lancet. 2004;364:869–74.
- Hsu VP, Hossain MJ, Parashar UD. Ali MM, Ksiazek TG, Kuzmin I, et al. Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis. 2004;10:2082–7.
- Ho M. Enterovirus 71: the virus, its infections and outbreaks. J Microbiol Immunol Infect. 2000;33:205–16 .PubMedGoogle Scholar
- Venkatesan A, Tunkel AR, Bloch KC. Lauring AS, Sejvar J, Bitnun A, et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the International Encephalitis Consortium. Clin Infect Dis. 2013;57:1114–28. PMID: 23861361 DOIGoogle Scholar
- Khetsuriani N, Holman RC, Anderson LJ. Burden of encephalitis-associated hospitalizations in the United States, 1988–1997. Clin Infect Dis. 2002;35:175–82. DOIPubMedGoogle Scholar
- Khetsuriani N, Tong S, Lu X. Reed S, Erdman D, Campbell A, et al. Systemic infection with enteric adenovirus in immunocompetent child with Haemophilus influenzae disease. Emerg Infect Dis. 2009;15:355–7.
- Chunsuttiwat S, Warachit P. Japanese encephalitis in Thailand. Southeast Asian J Trop Med Public Health. 1995;26(Suppl 3):43–6.PubMedGoogle Scholar
- Olsen SJ, Supawat K, Campbell AP. Anantapreecha S, Liamsuwan S, Tunlayadechanont S, et al. Japanese encephalitis virus remains an important cause of encephalitis in Thailand. Int J Infect Dis. 2010;14:e888–92.
- Saisongkorh W, Rolain JM, Suputtamongkol Y, Raoult D. Emerging Bartonella in humans and animals in Asia and Australia. J Med Assoc Thai. 2009;92:707–31 .PubMedGoogle Scholar
- Na-Bangchang K, Congpuong K. Current malaria status and distribution of drug resistance in East and Southeast Asia with special focus to Thailand. Tohoku J Exp Med. 2007;211:99–113. DOIPubMedGoogle Scholar
- Luby SP, Gurley ES, Hossain MJ. Transmission of human infection with Nipah virus. Clin Infect Dis. 2009;49:1743–8 .DOIPubMedGoogle Scholar
- Wacharapluesadee S, Boongird K, Wanghongsa S. Ratanasetyuth N, Supavonwong P, Saengsen D, et al. A longitudinal study of the prevalence of Nipah virus in Pteropus lylei bats in Thailand: evidence for seasonal preference in disease transmission. Vector Borne Zoonotic Dis. 2010;10:183–90.
- Palacios G, Oberste MS. Enteroviruses as agents of emerging infectious diseases. J Neurovirol. 2005;11:424–33 and. DOIPubMedGoogle Scholar
- Lum LC, Lam SK, Choy YS, George R, Harun F. Dengue encephalitis: a true entity? Am J Trop Med Hyg. 1996;54:256–9 .PubMedGoogle Scholar
- Rajapakse S, Rodrigo C, Fernando D. Scrub typhus: pathophysiology, clinical manifestations and prognosis. Asian Pac J Trop Med. 2012;5:261–4.
- Weinberg A, Bloch KC, Li S, Tang YW, Palmer M, Tyler KL. Dual infections of the central nervous system with Epstein-Barr virus. J Infect Dis. 2005;191:234–7. DOIPubMedGoogle Scholar
- Bitnun A, Ford-Jones EL, Petric M. MacGregor D, Heurter H, Nelson S, et al. Acute childhood encephalitis and Mycoplasma pneumoniae. Clin Infect Dis. 2001;32:1674–84. PMID: 11360206
- Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA. The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California Encephalitis Project. Clin Infect Dis. 2012;54:899–904 .DOIPubMedGoogle Scholar
Figures
Tables
Follow Up
Earning CME Credit
To obtain credit, you should first read the journal article. After reading the article, you should be able to answer the following, related, multiple-choice questions. To complete the questions (with a minimum 75% passing score) and earn continuing medical education (CME) credit, please go to http://www.medscape.org/journal/eid. Credit cannot be obtained for tests completed on paper, although you may use the worksheet below to keep a record of your answers. You must be a registered user on Medscape.org. If you are not registered on Medscape.org, please click on the “Register” link on the right hand side of the website to register. Only one answer is correct for each question. Once you successfully answer all post-test questions you will be able to view and/or print your certificate. For questions regarding the content of this activity, contact the accredited provider, CME@medscape.net. For technical assistance, contact CME@webmd.net. American Medical Association’s Physician’s Recognition Award (AMA PRA) credits are accepted in the US as evidence of participation in CME activities. For further information on this award, please refer to http://www.ama-assn.org/ama/pub/about-ama/awards/ama-physicians-recognition-award.page. The AMA has determined that physicians not licensed in the US who participate in this CME activity are eligible for AMA PRA Category 1 Credits™. Through agreements that the AMA has made with agencies in some countries, AMA PRA credit may be acceptable as evidence of participation in CME activities. If you are not licensed in the US, please complete the questions online, print the certificate and present it to your national medical association for review.
Article Title:
Infectious Causes of Encephalitis and Meningoencephalitis in Thailand, 2003–2005
CME Questions
1. You are seeing a 16-year-old girl with a 3-day history of fever, severe headache, and confusion. She has just returned from travel to Thailand 2 days ago. Encephalitis is in your differential diagnosis. In the current study, what was the most common finding on ancillary studies among patients with encephalitis?
A. Cerebrospinal fluid (CSF) pleocytosis
B. Abnormal result on brain magnetic resonance imaging
C. Abnormal result on brain computed tomography scan
D. Electroencephalographic result consistent with encephalitis
2. As you evaluate this patient, what should you consider regarding the demographic and clinical backgrounds of patients with encephalitis in the current study?
A. Median age was 31 years
B. Nearly all patients were admitted to the hospital during summer months
C. Almost all patients were from rural areas
D. A minority of patients had a substantive co-morbid illness
3. The patient is admitted to the hospital, and you await test results to confirm the etiology of her encephalitis. What percentage of patients in the current study had a confirmed or probable etiology of encephalitis diagnosed?
A. 36%
B. 59%
C. 82%
D. 95%
4. What was the most commonly identified organism responsible for causing encephalitis in the current study?
A. West Nile virus
B. Japanese encephalitis virus
C. Chikungunya
D. Bartonella henselae
Activity Evaluation
|
1. The activity supported the learning objectives. |
||||
|
Strongly Disagree |
|
|
|
Strongly Agree |
|
1 |
2 |
3 |
4 |
5 |
|
2. The material was organized clearly for learning to occur. |
||||
|
Strongly Disagree |
|
|
|
Strongly Agree |
|
1 |
2 |
3 |
4 |
5 |
|
3. The content learned from this activity will impact my practice. |
||||
|
Strongly Disagree |
|
|
|
Strongly Agree |
|
1 |
2 |
3 |
4 |
5 |
|
4. The activity was presented objectively and free of commercial bias. |
||||
|
Strongly Disagree |
|
|
|
Strongly Agree |
|
1 |
2 |
3 |
4 |
5 |
1These authors contributed equally to this article.
2Members are listed at the end of this article.
Related Links
Table of Contents – Volume 21, Number 2—February 2015
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Sonja J. Olsen, Centers for Disease Control and Prevention, 1600 Clifton Rd NE, Mailstop A32, Atlanta, GA 30329-4027, USA
Top