Volume 16, Number 5—May 2010
Dispatch
Vitamin D Deficiency and Tuberculosis Progression
Abstract
To assess the association between vitamin D deficiency and tuberculosis disease progression, we studied vitamin D levels in a cohort of tuberculosis patients and their contacts (N = 129) in Pakistan. Most (79%) persons showed deficiency. Low vitamin D levels were associated with a 5-fold increased risk for progression to tuberculosis.
Deficiency of vitamin D (25-hydroxycholecalciferol) has long been implicated in activation of tuberculosis (TB) (1). Serum levels of vitamin D in TB patients are lower than in healthy controls (2,3). Paradoxically, prolonged treatment of TB also causes a decline in serum vitamin D levels (2). Several studies have suggested that vitamin D is a potent immunomodulator of innate immune responses (4,5) by acting as a cofactor for induction of antimycobacterial activity (6). Of the 22 countries that have the highest TB incidence, Pakistan ranks eighth. In a previous study in Karachi, we observed that active disease developed in 7 (6.4%) of 109 TB case-contacts within 2 years (7). In the present study, we explored the role of vitamin D deficiency in TB disease progression within this cohort.
Household contacts (n = 109) of 20 patients with recently diagnosed sputum-positive pulmonary TB (index case-patients) were enrolled at Masoomeen General Hospital, in Karachi during 2001–2004 for a TB household cohort study (7). Blood samples were collected at baseline and at 6, 12, and 24 months follow-up. Visiting health workers reviewed clinical charts every 3 months for the first 24 months and at a final home study visit during November 2007–January 2008 (45–74 months from baseline). Persons with secondary cases were referred to a consultant at Masoomeen General Hospital for additional investigation, including assessment of physical signs and symptoms, laboratory tests, chest radiographs, and sputum smear microscopy (7). For the present study, 129 de-identified, plasma samples preserved at –70°C from the baseline visit were shipped to Stanford University (Stanford, CA, USA) for analysis of vitamin D levels. Total circulating serum 25[OH] vitamin D was measured with ELISA by using the Immuno Diagnostic System Ltd (IDS, Fountain Hill, AZ, USA). All protocols were followed according to manufacturer’s instructions. Each test was run in duplicate, with mean absorbance computed from the average for 2 wells normalized to a zero calibrator well. Levels of vitamin D in test samples were derived by fitting a 2-parameter logistic curve to 6 standard levels and expressed as ng/mL (1 nmol/L × 0.4 = 1 ng/mL). All R2 values were >95%. The assay detection range was 6–360 nmol/L (2.4–144 ng/mL). Levels in 1 person were below the detection limit and were excluded from analysis. The ethical review committees of Aga Khan and Stanford universities approved the study protocol.
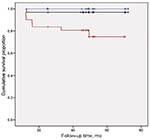
We used Kaplan-Meier analysis to evaluate the association of vitamin D levels with outcome of TB disease in 100 household contacts completing >1 follow-up visit. Vitamin D levels in the cohort were classified in population-based tertiles (low, middle, high). We used SAS version 9.3 (SAS Institute, Cary, NC, USA) for statistical analyses.
Median vitamin D level for the 128 cohort participants was 9.1 ng/mL (interquatrile range [IQR] 5.3–14.7); levels were 9.6 ng/mL (IQR 5.8–19.1) for 100 disease-free contacts, 7.9 ng/mL (IQR 4.7–10.3) for 20 TB index case-patients, 4.6 ng/mL (IQR 4.0–5.2) for 2 co-prevalent TB case-patients who were receiving antituberculous treatment at recruitment, and 5.1 ng/mL (IQR 3.4–14.3) in 6 household contacts with a history of TB treatment (2–10 years) (Figure 1, panel A). In the 100 disease-free household contacts, vitamin D levels were significantly higher than in the 28 participants with a history of TB diagnosis at baseline (p = 0.02; Mann-Whitney U test) (Figure 1, panel B). Median vitamin D levels were significantly lower in the 74 female patients than in the 54 male patients (7.8 vs. 11.9, Mann-Whitney U test, p = 0.0004) (Figure 1, panel C). When we stratified the cohort by vitamin D level, 79% had deficient (<20 ng/mL), 14% had insufficient (20–30 ng/mL), and 7% had sufficient (>30 ng/mL) levels of vitamin D (Table).
We next analyzed risk for progression to active TB in relation to plasma vitamin D levels. Of the 100 disease-free household contacts, 8 (8%) progressed to active disease during 4 years of follow-up. TB progression was significantly associated with relatively lower plasma vitamin D levels (Figure 2). Disease progressed in 7 (23%) of 30 patients with plasma vitamin D levels in the lowest tertile (<7 ng/mL), 1 (3%) of 32 with vitamin D levels in the middle tertile (7–13 ng/mL), and none of 30 in the highest tertile (>13 ng/mL) (p = 0.002, log rank). Six (75%) of 8 patients whose TB progressed were female patients with vitamin D levels in the lowest tertile. Further adjustment for age and sex yielded a relative risk for progression of 5.1 (1.2–21.3, p = 0.03) for a relative 1-log decrement in vitamin D levels, which suggests that vitamin D deficiency might be a strong risk factor for TB disease.
In this cohort follow-up study from Pakistan, low vitamin D levels were associated with progression to active TB disease in healthy household contacts. No deaths occurred during the follow-up period from either TB or unrelated causes. Our findings also suggest that vitamin D deficiency may explain the higher susceptibility of women to disease progression in our cohort. A high prevalence of vitamin D deficiency in female patients also was reported in ambulatory patients at Aga Khan University (8). Factors such as low socioeconomic status, poor nutrition, traditional/cultural traits, and little exposure to sunlight may further explain vitamin D deficiency in female patients in this cohort. Despite several limitations to our study, such as information about diet, body mass index, exposure to sunlight and the relatively small number of study participants, our results are supported by a meta-analysis of 7 case-control studies in different ethnic populations (including an Indian population) that showed 70% of healthy controls had higher vitamin D levels than did untreated TB patients (3). Previously in African immigrants in Melbourne, Victoria, Australia (9), lower mean vitamin D levels were associated with high probability of latent, current, or past TB infection. Cross-sectional studies are needed in Pakistan to appreciate this association with sex and susceptibility to TB with larger sample size. Most of the South Asian population, including Pakistani immigrants to European countries and South Indians, had <10 ng/mL of serum vitamin D level (10) and is consistent with reports from Aga Khan Hospital (8,11). Vitamin D plays an important role in activation of 1 α-hydroxylase to convert 25(OH) D to its active form [1, 25 (OH) 2D] that leads to expression of cathelicidin, a microbicidal peptide for Mycobacterium tuberculosis (5,12). Serum levels >30 ng/mL provide an adequate substrate for the enzyme. Serum levels <20 ng/mL may therefore impair the macrophage-initiated innate immune response to M. tuberculosis and offer a possible explanation for geographic and ethnic (13) variations in susceptibility to TB.
Vitamin D supplementation during TB treatment remains controversial; a few studies have reported clinical improvement in pulmonary TB (14) and 1 study reported no effect (15). However, our findings indicate that further studies should be conducted regarding use of vitamin D as a supplement for persons undergoing treatment for TB and those with latent TB infection.
Ms Talat is a PhD student at Aga Khan University. Her research interests include identification of immune biomarkers in TB.
Acknowledgments
We gratefully acknowledge Farida Talat and Farzana Sohan for their excellent support with follow up and documentation of families. We also thank Ayesha Habib and Romaina Iqbal for their constructive comments, Maqboola Dojki and Firdaus Shahid for administrative and logistic support and shipment of samples to Stanford University, Regina Dsouza for secretarial help, and Mohammed Anwar for excellent technical support in collection of samples.
Funding for recruitment of the cohort and plasma collection was provided by the National Commission on Biotechnology (PCST/NCB-AC3/2003) and the Higher Education Commission (HEC#20/796/ R&D/06). The International Research Support Initiative Program of the Higher Education Commission Government of Pakistan provided funding for travel and lodging. Vitamin D studies conducted at Stanford University were supported by funds from the Bill and Melinda Gates Foundation.
References
- Rook GA. The role of vitamin D in tuberculosis. Am Rev Respir Dis. 1988;138:768–70.PubMedGoogle Scholar
- Davies PD, Brown RC, Woodhead JS. Serum concentrations of vitamin D metabolites in untreated tuberculosis. Thorax. 1985;40:187–90. DOIPubMedGoogle Scholar
- Nnoaham KE, Clarke A. Low serum vitamin D levels and tuberculosis: a systematic review and meta-analysis. Int J Epidemiol. 2008;37:113–9. DOIPubMedGoogle Scholar
- Martineau AR, Wilkinson KA, Newton SM, Floto RA, Norman AW, Skolimowska K, IFN-gamma- and TNF-independent vitamin D-inducible human suppression of mycobacteria: the role of cathelicidin LL-37. J Immunol. 2007;178:7190–8.PubMedGoogle Scholar
- Ralph AP, Kelly PM, Anstey NM. L-arginine and vitamin D: novel adjunctive immunotherapies in tuberculosis. Trends Microbiol. 2008;16:336–44. DOIPubMedGoogle Scholar
- Crowle AJ, Ross EJ, May MH. Inhibition by 1,25(OH)2-vitamin D3 of the multiplication of virulent tubercle bacilli in cultured human macrophages. Infect Immun. 1987;55:2945–50.PubMedGoogle Scholar
- Hussain R, Talat N, Shahid F, Dawood G. Longitudinal tracking of cytokines after acute exposure to tuberculosis: association of distinct cytokine patterns with protection and disease development. Clin Vaccine Immunol. 2007;14:1578–86. DOIPubMedGoogle Scholar
- Zuberi LM, Habib A, Haque N, Jabbar A. Vitamin D deficiency in ambulatory patients. J Pak Med Assoc. 2008;58:482–4.PubMedGoogle Scholar
- Gibney KB, MacGregor L, Leder K, Torresi J, Marshall C, Ebeling PR, Vitamin D deficiency is associated with tuberculosis and latent tuberculosis infection in immigrants from sub-Saharan Africa. Clin Infect Dis. 2008;46:443–6. DOIPubMedGoogle Scholar
- Masood SH, Iqbal MP. Prevalence of vitamin D deficiency in South Asia. Pak J Med Sci. 2008;24:891–7.
- Khan AH, Iqbal R. Vitamin D deficiency in an ample sunlight country. J Coll Physicians Surg Pak. 2009;19:267–8.PubMedGoogle Scholar
- Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR, Toll-like receptor triggering of a vitamin D–mediated human antimicrobial response. Science. 2006;311:1770–3. DOIPubMedGoogle Scholar
- Martineau AR, Honecker FU, Wilkinson RJ, Griffiths CJ. Vitamin D in the treatment of pulmonary tuberculosis. J Steroid Biochem Mol Biol. 2007;103:793–8. DOIPubMedGoogle Scholar
- Wejse C, Gomes VF, Rabna P, Gustafson P, Aaby P, Lisse IM, Vitamin D as supplementary treatment for tuberculosis: a double-blind, randomized, placebo-controlled trial. Am J Respir Crit Care Med. 2009;179:843–50. DOIPubMedGoogle Scholar
Figures
Table
Cite This ArticleTable of Contents – Volume 16, Number 5—May 2010
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Rabia Hussain, Department of Pathology and Microbiology, Aga Khan University, Stadium Rd, PO Box 3500, Karachi-74800, Pakistan
Top