Volume 18, Number 6—June 2012
Dispatch
Accuracy of ICD-10 Codes for Surveillance of Clostridium difficile Infections, France
Abstract
The sensitivity and specificity of surveillance for Clostridium difficile infections according to International Classification of Diseases, 10th revision, codes were compared with laboratory results as standard. Sensitivity was 35.6%; specificity was 99.9%. Concordance between the 2 methods was moderate. Surveillance based on ICD-10 codes underestimated the rate based on laboratory results.
Clostridium difficile causes 15%–25% of diarrhea after antimicrobial drug therapy and is the leading cause of nosocomial diarrhea in adults (1). Studies in the United States, Canada, and Europe have documented the increased rate and severity of C. difficile infections highlighting the need for efficient and accurate methods of surveillance (2–7). The use of International Classification of Diseases (ICD) codes for surveillance of C. difficile infections has been studied in the United States and in Singapore and showed discordant results (8–12). Our objective was to compare the sensitivity and specificity of surveillance for C. difficile infections on the basis of ICD, 10th revision (ICD-10), codes with surveillance based on laboratory results.
The study was conducted at Saint-Antoine Hospital, a 750-bed university-affiliated public hospital in Paris, France. The study population comprised all patients hospitalized during January 1, 2000–December 31, 2010. C. difficile testing was performed only on unformed fecal samples of patients clinically suspected to have C. difficile infection. Laboratory diagnosis of C. difficile infection did not vary during the study period and was based on the stool cytotoxicity assay coupled with the toxigenic culture. A bacteriologic case of C. difficile infection was defined as a positive cytotoxicity assay result and/or a positive toxigenic culture.
Data were collected retrospectively from the electronic discharge summaries (French medico-administrative database) and from the hospital microbiology laboratory. All patients with a positive laboratory result for C. difficile (Bact+) and/or the ICD-10 discharge code for C. difficile infection, A04.7, as principal or associated diagnosis (ICD10+), were identified. For patients with multiple laboratory results during the same hospitalization, we used only the initial result.
We classified cases as concordant (Bact+/ICD10+) or discordant (Bact+/ICD10– or Bact–/ICD10+). Bact+/ICD10– discordant cases were compared with concordant cases to identify factors predictive of missing codes. Medical records were reviewed for Bact–/ICD10+ case-patients.
Statistical analysis included κ, χ2, and the Mann-Whitney U test. We used the Spearman test to measure the correlation between the 2 methods for yearly incidence of C. difficile infection. Data were analyzed with Epi Info version 6.01 (Centers for Disease Control and Prevention, Atlanta, GA, USA), GraphPad Prism version 4.03 (GraphPad Software, Inc., La Jolla, CA, USA) and R version 2.0 (R Foundation for Statistical Computing, Vienna, Austria).
During 2000–2010, of 317,040 hospitalizations, laboratory results and/or the ICD-10 code for C. difficile infection were positive for 698 (Figure 1). Sensitivity of the ICD-10 code, with laboratory results as the standard, was 35.6% (95% CI 31.9%–39.5%), and specificity was 99.9% (95% CI 99.9%–100.0%). The positive and negative predictive values were 79.2% (95% CI 73.9%–83.7%) and 99.9% (95% CI 99.8%–99.9%), respectively (Table). The sensitivity of ICD-10 codes varied among hospital wards. For wards with >50 cases of C. difficile infections during 2000–2010, sensitivity ranged from 14% to 71.6%. Average sensitivity increased from 26% for 2000–2005 to 39% for 2006–2010 (p = 0.02). Overall, concordance between the 2 methods was moderate (κ = 0.49, p<0.0001).
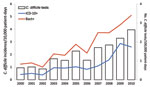
The incidence of C. difficile infection determined by ICD-10 codes underestimated the incidence determined by laboratory results. The relationship between methods for yearly incidence during the 11-year period was strong (Spearman correlation coefficient r = 0.95, 95% CI 0.81–0.98, p<0.0001). The rate of C. difficile infection by ICD-10 codes and laboratory results increased during 2000–2010 (Figure 2). The incidence of C. difficile infection also increased across all age groups. During 2000–2010, incidence increased by a factor of 3.3 for patients 15–44 years of age, by 2.9 for patients 45–64 years of age, and by 4.2 for patients >65 years of age.
Concordant cases (Bact+/ICD10+) and discordant cases (Bact+/ICD10–) did not differ significantly by mean age, sex, or proportion of patients >65 years of age. Diagnosis by positive toxigenic culture (with negative stool cytotoxicity assay result) was predictive for missing ICD-10 codes (χ2 = 19.22, p<0.0001), as was sample collection within 48 hours before discharge (χ2 = 16.57, p<0.0001). Patients with concordant results were more likely than patients with discordant results to have sample collection within 48 hours after admission (χ2 = 23.7, p<0.0001).
Review of medical records was possible for 34 (58%) of 59 discordant cases Bact–/ICD10+. Potential explanations for coding in the absence of a positive laboratory result included diagnosis outside the hospital (8 cases), positive result for a nontoxigenic strain of C. difficile (7 cases), diagnosis by endoscopy (6 cases), strong clinical suspicion of disease in patients with a history of C. difficile infection but no positive laboratory result (5 cases), and initial positive result subsequently corrected to a negative result by the laboratory (2 cases). No explanation could be found for the ICD-10 code in 6 cases: 5 had a negative laboratory result for C. difficile in the medical record, and 1 had no record of clinical suspicion or fecal sample collection.
This study covers an 11-year period and provides a large study population and more comprehensive analysis of the performance of ICD-10 codes. Our results indicate that surveillance for C. difficile infections based on ICD-10 codes underestimates the rate of C. difficile infections based on microbiological findings at Saint-Antoine Hospital. Even though trends in C. difficile infections incidence for the 2 methods correlated strongly, concordance was moderate.
The sensitivity of ICD-10 codes in this study is inferior to values previously reported in the United States (71%–78%) and in Singapore (49.6%) (8–11). Poor sensitivity and variability among wards could be attributed to differences in awareness by health care professionals of C. difficile infections and to differences in coding practices. At Saint-Antoine Hospital, coding is performed by physicians with limited training, not by trained medical coders. Therefore, the quality of coding can vary from 1 physician to another and among wards. In addition,, differences in sensitivity could be explained by changes in hospital financing. As of 2006, funding for hospitals in France has been connected to coding through Activity Based Payment (13). Comparison of average sensitivity before and after 2006 showed an overall increase, indicating that coding practices might improve with time as hospitals adapt to this system.
Our finding that sample collection within 48 hours before hospital discharge was predictive of missing ICD-10 codes is consistent with findings from previous studies and suggests that results obtained after patient discharge are less frequently coded (8,9,12). Diagnosis by toxigenic culture was also significantly associated with missing ICD-10 codes. The toxigenic culture is a long test requiring up to several days for results. At Saint-Antoine Hospital, results are provided at each step of analysis (stool cytotoxicity assay in 24 h, culture in 48 h, toxigenic culture within 5 d), which might introduce misinterpretation of preliminary results before the final comprehensive result.
Analysis of medical records for patients coded for C. difficile infections but lacking a positive laboratory result suggested several potential explanations for coding. Diagnoses made outside the hospital and those made by endoscopy are coded, indicating that cases diagnosed by methods other than in-hospital laboratory testing are captured by ICD-10 codes.
This study was limited to a single institution, and our findings might not necessarily apply to other institutions in France. The sensitivity of ICD-10 codes can be highly variable, and this method should be validated in different health care settings before being used for surveillance.
Use of ICD-10 codes underestimates the incidence of C. difficile infections compared with microbiological data. However, it may be an effective indicator for monitoring general trends in the rate of C. difficile infection.
Ms Jones is a master’s student in public health and epidemiology at René Descartes University in Paris. Her primary research interest is in the epidemiologic surveillance of infectious diseases.
Acknowledgment
We thank Bruno Coignard for his valuable comments and suggestions.
References
- Karen CC, Bartlett JG. Biology of Clostridium difficile: implications for epidemiology and diagnosis. Annu Rev Microbiol. 2011;65:501–21. DOIPubMedGoogle Scholar
- Pépin J, Valiquette L, Alary ME, Villemure P, Pelletier A, Forget K, Clostridium difficile—associated diarrhea in a region or Quebec from 1991 to 2003: a changing pattern of disease severity. CMAJ. 2004;171:466–72. DOIPubMedGoogle Scholar
- Loo VG, Poirier L, Miller MA, Oughton M, Libman MD, Michaud S, A predominantly clonal multi-institutional outbreak of Clostridium difficile–associated diarrhea with high morbidity and mortality. N Engl J Med. 2005;353:2442–9. DOIPubMedGoogle Scholar
- Archibald LK, Banerjee SN, Jarvis WR. Secular trends in hospital-acquired Clostridium difficile disease in the United States, 1987–2001. J Infect Dis. 2004;189:1585–9. DOIPubMedGoogle Scholar
- McDonald LC, Owings M, Jernigan DB. Clostridium difficile infection in patients discharged from US short-stay hospitals, 1996–2003. Emerg Infect Dis. 2006;12:409–15. DOIPubMedGoogle Scholar
- Kuijper EJ, Coignard B, Tüll P. Emergence of Clostridium difficile-associated disease in North America and Europe. Clin Microbiol Infect. 2006;12(Suppl 6):2–18. DOIPubMedGoogle Scholar
- Gerding DN. Global epidemiology of Clostridium difficile infection in 2010. Infect Control Hosp Epidemiol. 2010;31(Suppl 1):S32–4. DOIPubMedGoogle Scholar
- Dubberke ER, Reske KA, McDonald LC, Fraser VJ. ICD-9 codes and surveillance for Clostridium difficile–associated disease. Emerg Infect Dis. 2006;12:1576–9. DOIPubMedGoogle Scholar
- Scheurer DB, Hicks LS, Cook EF, Schnipper JL. Accuracy of ICD-9 coding for Clostridium difficile infections: a retrospective cohort. Epidemiol Infect. 2007;135:1010–3. DOIPubMedGoogle Scholar
- Chan M, Lim PL, Chow A, Win MK, Barkham TM. Surveillance for Clostridium difficile Infection: ICD-9 coding has poor sensitivity compared to laboratory diagnosis in hospital patients, Singapore. PloS ONE. 2011;6:e15603. DOIPubMedGoogle Scholar
- Dubberke ER, Butler AM, Yokoe DS, Mayer J, Hota B, Mangino JE, Multicenter study of durveillance for hospital-onset Clostridium difficile infection by the use of ICD-9-CM diagnosis codes. Infect Control Hosp Epidemiol. 2010;31:262–8. DOIPubMedGoogle Scholar
- Benoit SR, McDonald C, English R, Tokars JI. Automated surveillance of Clostridium difficile infections using BioSense. Infect Control Hosp Epidemiol. 2011;32:26–33. DOIPubMedGoogle Scholar
- Or Z. Activity based payment in France. Euro Observer: The Health Policy Bulletin of the European Observatory on Health Systems and Policy. 2009;11:5–6.
Figures
Table
Cite This ArticleTable of Contents – Volume 18, Number 6—June 2012
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Gabrielle Jones, Hôpital Saint-Antoine, UHLIN, 184 Rue du Faubourg Saint-Antoine, 75012 Paris, France
Top