Volume 14, Number 11—November 2008
Dispatch
Successful Treatment of Disseminated Acanthamoeba sp. Infection with Miltefosine
Abstract
We report on an HIV-negative but immunocompromised patient with disseminated acanthamoebiasis, granulomatous amoebic encephalitis, and underlying miliary tuberculosis and tuberculous meningitis. The patient responded favorably to treatment with miltefosine, an alkylphosphocholine. The patient remained well with no signs of infection 2 years after treatment cessation.
A 25-year-old man from India, who had been living in Austria for 7 years and had no previous history of major illnesses, was brought by ambulance to the hospital for dyspnea, cough, fever, and weight loss. During neurologic examination, a hearing impairment was suspected. The patient was unable to walk because of severe ataxia. Skin examination showed several necrotic ulcers with purulent discharge and black eschars, measuring 0.5 cm to 3 cm, located on the skull, back, neck, and arms (Figure 1, panels A and B). Miliary tuberculosis (TB) of the lungs, liver, spleen, and kidneys was suspected on the basis of chest radiography and computed tomography (CT) of chest and abdomen. Ziehl-Nielsen (ZN) staining for acid-fast bacilli in sputum, bronchial secretions, and lavage obtained through bronchoscopy was negative. PCR for Mycobacterium tuberculosis in bronchial secretions and serum was positive. Culture on Loewenstein agar resulted in growth of nonresistant M. tuberculosis after 31 days. Blood cultures were negative for aerobic/anaerobic bacteria, mycobacteria, and fungi. Results of serologic tests were negative for Aspergillus, Candida, Cryptococcus, Histoplasma, Blastomyces, and Coccidioides spp. Severe immunosuppression with a CD4+ lymphocyte count of 182 cells/μL made HIV infection probable, but HIV testing results were negative. Cranial CT showed multiple small enhancing lesions in cerebral cortex and underlying white matter, pons, midbrain, and around most of the cisterns. On magnetic resonance imaging (MRI), the lesions appeared as high T2 signal areas that enhanced heterogeneously or in a ringlike manner. These findings were compatible with the diagnosis of meningoencephalitis with intracerebellar abscess formation.
Cerebrospinal fluid (CSF) obtained through lumbar puncture was negative for Toxoplasma gondii, Encephalitozoon cuniculi, and Enterocytozoon bieneusi by PCR and for Trypanosoma gambiense by indirect hemagglutination assay. Staining and antigen testing (enzyme immunoassay) for Cryptococcus neoformans was negative, as was Treponema pallidum antibody testing. No viruses (herpes simplex 1 and 2, varicella zoster, enterovirus) could be detected by PCR. Cultures were negative for aerobic/anaerobic bacteria and fungi. ZN staining detected acid-fast bacilli that were confirmed to be nonresistant M. tuberculosis after culture for 38 days. PCR for M. tuberculosis was positive. An Acanthamoeba–specific PCR (1) and DNA sequencing of the PCR product showed Acanthamoeba genotype T2 (corresponding to group III). High immunoglobulin (Ig) G (2,000) and IgM (1,000) titers against Acanthamoeba spp. could be demonstrated serologically. The organism could not be grown in culture (2).
Two skin-biopsy specimens were obtained; they showed necrotizing granulomatous inflammation affecting the entire dermal thickness and subcutis. Stains and culture were negative for Mycobacterium spp., fungi, and Acanthamoeba spp. but tested positive for acanthamoebae by PCR. In addition to a standard tuberculostatic 5-drug regimen including intravenous streptomycin, empiric anti-amoebic treatment based on data retrieved from the few case reports of successful treatment of systemic Acanthamoeba infections (3–5) was initiated. The regimen included a combination of parenteral trimethoprim/sulfamethoxazole (later changed to oral sulfadiazine) and parenteral fluconazole. CSF samples drawn 2 and 8 weeks after initiation of therapy tested negative for mycobacteria by ZN staining, PCR, and culture but remained positive for Acanthamoeba spp. by PCR.
Transbronchial lung biopsy specimens from a second bronchoscopy performed 1 month after admission tested negative for mycobacteria by ZN staining, PCR, and culture but positive for Acanthamoeba spp. by PCR. Acanthamoebae could not be cultivated from bronchial secretions or biopsy sample; immunostaining that used a polyclonal rabbit anti–A. castellanii (genotype T4) serum was negative.
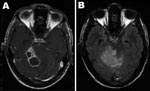
Within 12 weeks after initiation of tuberculostatic therapy, complete clinical and radiologic resolution of miliary TB of lungs, liver, spleen, and kidneys could be achieved, and the CD4+ lymphocyte count increased to 421 cells/μL. Nevertheless, the neurologic status of the patient deteriorated, even after liposomal amphotericin B and flucytosine had been added to the regimen. Consecutive cranial CT and cranial MRI scans demonstrated progression of the lesions, with the biggest lesion (1.8 cm in diameter) located in the right cerebellopontine angle and cerebellum (Figure 2, panels A and B).
As skin lesions were also gaining size, treatment with miltefosine, a phosphocholine analog that has proven successful in treating visceral leishmaniasis (6) and is highly effective against acanthamoebae in vitro (7,8), was initiated topically as a solution, 60 mg/mL, 1 drop applied directly to each skin lesion 2 times a day. After dramatic improvements of the skin lesions were observed within only 3 weeks (Figure 1, panel C), our patient began peroral miltefosine 100 mg/day (2.5 mg/kg); all other drugs except the tuberculostatic 5-drug regimen were stopped.
On MRI scan, performed 8 weeks after admission, the brain abscess located in the right cerebellopontine angle had reached a size of 4 cm, leading to a rise of intracranial pressure that could not be controlled by intravenous administration of mannitol and dexamethasone. Nine weeks after admission, an Ommaya Reservoir was implanted, and up to 100 mL of CSF was drained daily to control intracranial pressure. Amikacin, the only other drug that seemed to have some efficacy against Acanthamoeba spp. in vitro (2), was given intrathecally and intravenously (20 mg/2 mL intrathecally + 1,000 mg/d intravenously) in place of the streptomycin originally included in the 5-drug regimen, under continuous monitoring of peak and trough levels in CSF and blood. A surgical excision of the abscess was performed 3 weeks later. The histologic specimen of this lesion was again positive for Acanthamoeba spp. by PCR but negative by immunostaining. Neither acanthamoebae nor mycobacteria could be grown in culture, despite positive ZN staining of the specimen (Table).
Under ongoing therapy with miltefosine, amikacin, and 4 more tuberculostatic drugs, the patient improved. The remaining cerebral lesions regressed in size. Healing of the dermal lesions was achieved within 6 weeks; topical miltefosine treatment was stopped after 8 weeks. Intrathecal amikacin and oral miltefosine therapy was halted 6 and 12 weeks, respectively, after initiation.
A 2-drug tuberculostatic therapy was maintained for 1 year after the patient had been discharged from hospital. Two more lumbar punctures were performed 23 and 29 weeks after the patient was initially evaluated. For the first time neither mycobacteria nor acanthamoebae could be detected. CT scan and MR imaging of the brain showed no major pathology. Serologic titers, which had gradually declined after initiation of miltefosine therapy, reached normal levels. The patient was transferred to a specialized neurologic institution for rehabilitation. Ataxia and hearing impairment did not improve. During the next 24 months, the patient was regularly seen in our outpatient clinic. No signs of infection could be found, and Acanthamoeba immunoreactivity remained below cutoff.
Disseminated Acanthamoeba infection is a rare disease characterized by widespread granulomatous infiltration of the skin and extracerebral organs; it usually occurs in immunocompromised patients. Most reported cases have progressed to granulomatous amoebic encephalitis (GAE). The incidence of GAE is low in spite of the ubiquity of these amoebae. Although <200 cases of GAE have been described worldwide, it is still of substantial medical relevance because it is usually fatal due to diagnostic difficulties (9,10) and lack of effective treatment.
In our patient, co-infection with M. tuberculosis with severe immunosuppression may have contributed to his susceptibility to Acanthamoeba infection but not to the disease progression and clinical deterioration seen even after TB could be controlled. Problems in culturing acanthamoebae from clinical specimens have been reported frequently, and isolation of amoebae from CSF is generally uncommon (11). In our case no reactivity to immunofluorescence was seen, either because the biopsy missed the area of active infection or because of the low sensitivity of polyclonal antibodies available. Nevertheless, early diagnosis of Acanthamoeba infection in our patient was achieved by molecular methods that proved to be more sensitive than microscopy and culture.
GAE and cutaneous Acanthamoeba infections have been empirically treated with a wide array of antimicrobial agents. The outcome has been mostly failure (3,11,12), except for a few cases that occurred in immunocompetent patients (10,13–15). Few case studies reported successful treatment of patients with a solitary brain lesion or initiation of therapy before the infection entered the brain (5,10). The first successful treatment of AIDS-related GAE was reported in 2000 (4).
The condition of our patient deteriorated under empirical treatment with antimicrobial agents previously used to treat Acanthamoeba infection. When anti-amoebic therapy was changed to peroral and topical miltefosine, the skin lesions healed and the brain lesions regressed. After the remaining brain lesion had been surgically excised, the patient could be discharged from the hospital. Two years after treatment ended, the patient is partly rehabilitated with no signs of amoebic or mycobacterial infection.
Dr Aichelburg is a respiratory and infectious diseases physician at the Otto Wagner Hospital in Vienna. He specializes in HIV medicine. His other research interests include tuberculosis, malaria, and opportunistic infections.
Acknowledgment
We thank Maximilian C. Aichelburg for his valuable comments and editorial assistance with the preparation of this article.
References
- Schroeder JM, Booton GC, Hay J, Niszl IA, Seal DV, Markus MB, Use of subgenic 18S ribosomal DNA PCR and sequencing for genus and genotype identification of acanthamoebae from humans with keratitis and from sewage sludge. J Clin Microbiol. 2001;39:1903–11. DOIPubMedGoogle Scholar
- Walochnik J, Aichelburg A, Assadian O, Steuer A, Visvesvara G, Vetter N, Granulomatous amoebic encephalitis caused by Acanthamoeba amoebae of genotype T2 in a human immunodeficiency virus-negative patient. J Clin Microbiol. 2008;46:338–40. Epub 2007 Nov 14. DOIPubMedGoogle Scholar
- Marciano-Cabral F, Cabral G. Acanthamoeba spp. as agents of disease in humans. Clin Microbiol Rev. 2003;16:273–307. DOIPubMedGoogle Scholar
- Seijo Martinez M, Gonzalez-Mediero G, Santiago P, Rodriguez de Lope A, Diz J, Conde C, Granulomatous amebic encephalitis in a patient with AIDS: isolation of Acanthamoeba sp. Group II from brain tissue and successful treatment with sulfadiazine and fluconazole. J Clin Microbiol. 2000;38:3892–5.PubMedGoogle Scholar
- Slater CA, Sickel JZ, Visvesvara GS, Pabico RC, Gaspari AA. Successful treatment of disseminated acanthamoeba infection in an immunocompromised patient. N Engl J Med. 1994;331:85–7. DOIPubMedGoogle Scholar
- Jha TK, Sundar S, Thakur CP, Bachmann P, Karbwang J, Fischer C, Miltefosine, an oral agent, for the treatment of Indian visceral leishmaniasis. N Engl J Med. 1999;341:1795–800. DOIPubMedGoogle Scholar
- Walochnik J, Duchene M, Seifert K, Obwaller A, Hottkowitz T, Wiedermann G, Cytotoxic activities of alkylphosphocholines against clinical isolates of Acanthamoeba spp. Antimicrob Agents Chemother. 2002;46:695–701. DOIPubMedGoogle Scholar
- Schuster FL, Guglielmo BJ, Visvesvara GS. In-vitro activity of miltefosine and voriconazole on clinical isolates of free-living amebas: Balamuthia mandrillaris, Acanthamoeba spp., and Naegleria fowleri. J Eukaryot Microbiol. 2006;53:121–6. DOIPubMedGoogle Scholar
- Bloch KC, Schuster FL. Inability to make a premortem diagnosis of Acanthamoeba species infection in a patient with fatal granulomatous amebic encephalitis. J Clin Microbiol. 2005;43:3003–6. DOIPubMedGoogle Scholar
- Petry F, Torzewski M, Bohl J, Wilhelm-Schwenkmezger T, Scheid P, Walochnik J, Early diagnosis of Acanthamoeba infection during routine cytological examination of cerebrospinal fluid. J Clin Microbiol. 2006;44:1903–4. DOIPubMedGoogle Scholar
- Schuster FL, Visvesvara GS. Opportunistic amoebae: challenges in prophylaxis and treatment. Drug Resist Updat. 2004;7:41–51. DOIPubMedGoogle Scholar
- Shirwadkar CG, Samant R, Sankhe M, Deshpande R, Yagi S, Schuster FL, Acanthamoeba encephalitis in patient with systemic lupus, India. Emerg Infect Dis. 2006;12:984–6.PubMedGoogle Scholar
- Barete S, Combes A, de Jonckheere JF, Datry A, Varnous S, Martinez V, Fatal disseminated Acanthamoeba lenticulata infection in a heart transplant patient. Emerg Infect Dis. 2007;13:736–8.PubMedGoogle Scholar
- Ofori-Kwakye SK, Sidebottom DG, Herbert J, Fischer EG, Visvesvara GS. Granulomatous brain tumor caused by Acanthamoeba. Case report. J Neurosurg. 1986;64:505–9.PubMedGoogle Scholar
- Lalitha MK, Anandi V, Srivastava A, Thomas K, Cherian AM, Chandi SM. Isolation of Acanthamoeba culbertsoni from a patient with meningitis. J Clin Microbiol. 1985;21:666–7.PubMedGoogle Scholar
Figures
Table
Cite This ArticleTable of Contents – Volume 14, Number 11—November 2008
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Alexander C. Aichelburg, Pulmonological Centre, SMZ Baumgartner Hoehe, Otto Wagner Hospital, Sanatoriumsstrasse 2, A-1140 Vienna, Austria;
Top