Volume 30, Number 5—May 2024
Research
Cross-Sectional Study of Q Fever Seroprevalence among Blood Donors, Israel, 2021
Abstract
We evaluated Q fever prevalence in blood donors and assessed the epidemiologic features of the disease in Israel in 2021. We tested serum samples for Coxeilla burnetii phase I and II IgG using immunofluorescent assay, defining a result of >200 as seropositive. We compared geographic and demographic data. We included 1,473 participants; 188 (12.7%) were seropositive. The calculated sex- and age-adjusted national seroprevalence was 13.9% (95% CI 12.2%–15.7%). Male sex and age were independently associated with seropositivity (odds ratio [OR] 1.6, 95% CI 1.1–2.2; p = 0.005 for male sex; OR 1.2, 95% CI 1.01–1.03; p<0.001 for age). Residence in the coastal plain was independently associated with seropositivity for Q fever (OR 1.6, 95% CI 1.2–2.3; p<0.001); residence in rural and farming regions was not. Q fever is highly prevalent in Israel. The unexpected spatial distribution in the nonrural coastal plain suggests an unrecognized mode of transmission.
Q fever, caused by infection with the bacterium Coxeilla burnetii, is an endemic disease in Israel. In 2021, a total of 341 cases of Q fever were reported to the Epidemiology Division, Ministry of Health (1), representing an estimated incidence of 3.6/100,000 population. For comparison, the highest incidence of Q fever in recent years in the European Union was reported from Spain, reaching 0.7/100,000 population in 2019 (2). Despite the longstanding endemicity of Q fever in Israel, little is known about the actual epidemiology, geographic distribution, and groups at highest risk for the disease (3–6). Ministry of Health data are based on passive notifications, relying on reporting by the treating physician and laboratory staff where the diagnostic test suggestive of Q fever was performed. This reporting system is known to be highly affected by the awareness and motivation of medical staff (both physicians and laboratory workers). Almost half of acute Q fever cases are asymptomatic (7), but infections can progress years later to the more severe, chronic form of the disease. Thus, the actual population incidence of Q fever, including events missed by the passive surveillance system, has not been documented in Israel. In this study, we evaluated the prevalence of Q fever in adult healthy volunteer blood donors in Israel and assessed the epidemiologic features of the disease.
Study Design and Setting
We conducted a cross-sectional nationwide prevalence study using blood samples collected during January 1–October 8, 2021. Samples were collected by Magen David Adom (MDA) National Blood Service. Blood donations were performed in locations across the country. Samples were collected and stored from donors who signed an informed consent agreeing to participate in the study. Participants completed an obligatory donor health questionnaire that included their demographic details and health status. The study was performed in line with the principles of the Declaration of Helsinki. The study was approved by the ethics committees of Rambam Health Care Campus and MDA’s research committee. Informed consent was obtained from all individual participants included in the study.
Participants
Participants were male and nonpregnant female adult blood donors >18 years of age (pregnant women are excluded from blood donation) who completed the donor health questionnaire and signed the MDA consent form for use of blood donations in research. Samples for this study were selected randomly from the full sample pool (≈1,000 donations/day) by donation site from all districts in Israel. To achieve a study group representative of the whole population, we enriched the final study set with samples taken from female donors and from Arab-populated locations; however, sample selection was performed randomly from the respective sample pools.
Study Flow and Data Collection
We centrifuged specimens obtained from blood donors, saved serum samples at 4°C, and transferred samples to the reference laboratory for antibody testing. We kept samples anonymous and did not convey results to the blood donors.
We collected demographic data on date of donation, date and country of birth, sex, and location of residence. We extracted data on the residence localities’ sociodemographic characteristics from the Israeli Central Bureau of Statistics (CBS) website. Those data consisted of population size, ethnicity of population, and socioeconomic index cluster (categorized as 1–10 on the basis of multiple social and economic variables). We defined Arab localities as localities in which >80% of the population were Arab. Localities were classified by socioeconomic cluster as low (1–3), middle (4–7), or high (8–10) status. Rural localities were defined as those with <5,000 inhabitants.
Microbiological Methods
We performed screening for presence of phase I and phase II C. burnetii IgG by using an in-house indirect immunofluorescence assay at the National Central Laboratory for Rickettsiosis in the Israel Institute for Biologic Research. We performed the test by using antigens of phase I Ohio strain and phase II Nine Mile strain of Coxiella burnetii. This test has been used clinically for many years as the standard for Q fever diagnosis in Israel. The test was externally validated upon its introduction and continues to be under periodic internal and external quality assurance control programs. Results were reported as borderline if positive in a titer of 100 and seropositive with antibody titers of phase I or phase II IgG >200.
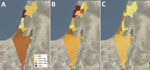
Seroprevalence Spatial Distribution
We calculated Q fever seroprevalence rate by locality, natural region, and subdistrict and district level. Israel is divided into districts and subdistricts on the basis of administrative considerations and into natural regions on the basis of regional geographic features. We used the natural regions to divide the country into 4 areas: the coastal plain and the inner regions of the north, center, and south. We created prevalence choropleth maps according to district, subdistrict, and natural region classification. We created maps using ArcGIS Desktop software (Esri, https://www.esri.com) to display spatial prevalence data.
Statistical Methods
We expressed seroprevalence rates as an overall rate and in geographic and demographic groups. We calculated the sex- and age-adjusted seroprevalence to estimate national Q fever prevalence in adults >18 years of age using the sex and age distribution of the population of Israel according to 2019 CBS data. We used the χ2 test to assess the association between available epidemiologic characteristics and seropositivity for Q fever. We used binary logistic regression for multivariate analysis. We included variables with p<0.05 in bivariate analysis in the binary regression. All statistical tests were 2-tailed.
The sample size needed for prevalence estimation was calculated targeting a 95% CI and assuming a Q fever prevalence in Israel of 4% (on the basis of previous studies from Q fever–endemic developed countries that reported a prevalence range of 3%–5%). We targeted a precision of 1%. The sample size needed was calculated to be 1,476.
During January 1–October 8, 2021, samples were collected from 1,600 blood donors; we tested 1,473 samples with complete epidemiologic data. Of those, 188 (12.7%) samples were positive for C. burnetii antibodies. Phase II IgG >200 was detected in 187 participants; concomitant phase I IgG >200 was detected in 57 (30%) of those participants’ samples. Only 1 sample was found with positive phase I IgG and negative phase II IgG (Table 1).
The mean age of the participants was 36.6 + 13.9 years; 859 (58.3%) were men and 614 (41.7%) women. The sex- and age-adjusted prevalence rate was 13.9% (95% CI 12.2%–15.7%).
The seroprevalence of Q fever was higher among men (14.9% [128/859]) than women (9.8% [60/614]) (Table 2). In addition, seroprevalence increased with age, reaching a rate of 17.4% (52/299) among participants >50 years of age. Participants living in rural locations had seropositivity of 10.6% (51/480). Seroprevalence rates were similar in Arab and Jewish localities and in low, middle, and high socioeconomic status localities.
Seropositive cases were widely distributed across all parts of the country. Prevalence rates varied among regions; rates were highest in the coastal plain (15.9% [100/629]) and lowest in the noncoastal central region (8.8% [37/419]) (Figure; Appendix Table 1).
In bivariate comparison, older age, male sex, and residence in the coastal plain were more prevalent in the seropositive group than the seronegative one (Table 3). Residence in a rural area was less prevalent in the seropositive group but did reach statistical significance. In multivariate logistic regression analysis, variables that were independently associated with Q fever seropositivity were age (odds ratio [OR] 1.2, 95% CI 1.01–1.03; p<0.001), male sex (OR 1.6, 95% CI 1.1–2.2; p = 0.005), and residence in the coastal plain (OR 1.6, 95% CI 1.2–2.3; p<0.001).
We found high Q fever seroprevalence at an estimated rate of 13.9% among healthy adults in Israel, with wide geographic distribution. Seropositive status was independently associated with male sex, older age, and residence in the coastal plain.
National seroprevalence studies of Q fever from the past 2 decades have been conducted in several countries. In the United States (8), the Netherlands (before the large outbreak in 2007) (9), and Chile (10), prevalence was ≈3%. Higher prevalence rates were reported from Australia (5.6%) (11), French Guiana (9.6%) (12), and Northern Ireland (12.8%) (13). Smaller studies from other countries demonstrated a broad range of Q fever prevalence: 6.9% in Bhutan (14), 6.9% in Reunion Islands (15), 24.2% in Jordan (16), and 52.7% in Cyprus (17). Those studies used different testing methods and different cutoff titers to define seropositivity, which could have contributed to differences in reported prevalence rates.
In this study, we used a relatively high cutoff titer to define seropositivity, which could have led to an underestimation of seroprevalence rate. For example, if we had used a cutoff of 100 instead of 200 to define seropositivity, the crude overall prevalence rate would have increased from 12.7% to 21.8%. Nevertheless, the high seroprevalence rate we found seems to correlate with reported ongoing and increasing incidence of the disease, as reflected in clinical reports in the national surveillance (1) (Appendix Figure). The increase in incidence observed in recent years had been preceded by several outbreaks reported in different areas (18–20).
Increasing age and male sex as risk factors for Q fever have been reported in various countries in both clinical and epidemiological studies (8,11,21,22); possible explanations have been related to increased exposure from living in endemic places and certain occupational exposures. We did not have occupational data for participants in this study, but previous local reports have frequently mentioned that animal exposure does not seem to be a risk factor (23–25). Similarly, residence in a rural area was not associated with Q fever seroprevalence in our study, contrary to previous reports (11,15,17,26). Yet, the significance of male sex as a risk factor might be related to exposure factors that should be further investigated.
Residence in the coastal plain was significantly associated with Q fever prevalence in our study. Of note, the coastal plain region in Israel contains more urban and highly populated localities than other regions, whereas livestock farms are more prevalent in noncoastal areas, mainly in the south and north (27). For example, the subdistrict with the highest seroprevalence rate in our study was Hadera (26%); only 7.2% of sheep farms and 4.2% of cattle farms in Israel are located in that subdistrict (27). Wind can carry sporelike forms of C. burnetii to distances of up to 18 km, as documented in previous studies (28,29). The short 17-km distance of Hadera subdistrict from the eastern border (an area for which data are missing) should be taken into consideration in further studies. However, those factors alone cannot explain the unique spatial pattern of prevalence depicted in our study; in those circumstances, we would have expected a decreasing gradient of prevalence in which the highest rates would be observed in rural and inner noncoastal regions. Our spatial prevalence data point to an unknown mode of transmission of the disease that seems to play a major role in current epidemiology in Israel. The possibility of an unrecognized animal that might be a reservoir for the bacterium in the urban environment should be investigated. Special attention should be paid to stray cats and wild boars, particularly because wild boars have become a frequent observation inside Haifa, the largest city in the northern coastal plain. In addition, rivers and streams could theoretically play a role in the transmission of the bacterium from the inner areas of the country to the coastal plain; in 1 study, C. burnetii was detected in contaminated river water (30).
Compared with brucellosis, another endemic zoonotic disease in Israel, in which most cases occur among Arabs (31), in this study, Q fever seems to affect Arab and Jewish locations at similar rates. The transmission mode of brucellosis is clearly associated with consumption of unpasteurized dairy products and direct contact with infected sheep (32). The fact that sheep herds, which are most likely the common source of both diseases, are found mostly inside or in close proximity to Arab locations (27) supports a different transmission mode of Q fever.
The first limitation of our study is the epidemiologic differences between healthy blood donors and the general population. We did not include persons <18 years of age, pregnant women, and persons who were not qualified to donate blood because of responses on the donor health questionnaire or results of physical tests performed before donation (i.e., blood pressure, heart rate, hemoglobin levels). For estimating national prevalence, we adjusted our results to age and sex distribution of the general population. Still, underrepresentation of Arab population in our cohort was prominent and might have missed prevalence ethnic differences. Another limitation is the absence of data on individual risk factors such as occupation and animal exposure. As mentioned previously, those data were not found to be associated with clinical illness in reports from Israel (23) but should be further studied prospectively.
In conclusion, our study presents key data on the epidemiology of Q fever in Israel, demonstrating high seroprevalence throughout the country, with predominance in the coastal plain for unknown reasons and no association with rural areas or livestock farms. Future studies should further investigate environmental factors that seem to play a major role in the transmission of this endemic disease. Improving our knowledge of disease transmission is critical in planning prevention programs for this highly endemic disease with significant consequences for public health.
Dr. Ghanem-Zoubi is an infectious diseases and internal medicine specialist and the deputy director of the Infectious Diseases Institute, Rambam Health Care Campus, Haifa, Israel. Her primary research interest in recent years is infective endocarditis and zoonoses, including brucellosis and Q fever.
Acknowledgments
We thank Faris Jahshan for the advice and assistance in map creation. We thank Sharon Eliyahu and Michal Bitan for administrative and technical assistance. We also thank Dina Gohaman, Yafa Afrimov, and Ayala Itzik for the laboratory technical work.
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by N.G.-Z. and M.P. The first draft of the manuscript was written by N.G.-Z. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
References
- Israeli Ministry of Health. Epidemiological weekly report [cited 2022 Nov 16]. https://www.gov.il/he/Departments/DynamicCollectors/weekly-epidemiological-report
- European Food Safety Authority and European Centre for Disease Control and Prevention. The European Union summary report on trends and sources of zoonoses, zoonotic agents and food‐borne outbreaks in 2014. EFSA J. 2015;13:4329.
- Ergas D, Keysari A, Edelstein V, Sthoeger ZM. Acute Q fever in Israel: clinical and laboratory study of 100 hospitalized patients. Isr Med Assoc J. 2006;8:337–41.PubMedGoogle Scholar
- Reisfeld S, Mhamed SH, Stein M, Chowers M. Acute Q fever in Israel: clinical and demographic data 2006–2016. Open Forum Infect Dis. 2017;4(suppl_1):S124. DOIGoogle Scholar
- Siegman-Igra Y, Kaufman O, Keysary A, Rzotkiewicz S, Shalit I. Q fever endocarditis in Israel and a worldwide review. Scand J Infect Dis. 1997;29:41–9. DOIPubMedGoogle Scholar
- Bishara J, Pitlik S, Yagupsky P, Hershkovitz D. Comparative incidence of acute Q fever in two ethnic groups in Israel. Eur J Clin Microbiol Infect Dis. 2004;23:224–5. DOIPubMedGoogle Scholar
- Anderson AD, Kruszon-Moran D, Loftis AD, McQuillan G, Nicholson WL, Priestley RA, et al. Seroprevalence of Q fever in the United States, 2003-2004. Am J Trop Med Hyg. 2009;81:691–4. DOIPubMedGoogle Scholar
- Schimmer B, Notermans DW, Harms MG, Reimerink JHJ, Bakker J, Schneeberger P, et al. Low seroprevalence of Q fever in The Netherlands prior to a series of large outbreaks. Epidemiol Infect. 2012;140:27–35. DOIPubMedGoogle Scholar
- Tapia T, Olivares MF, Stenos J, Iglesias R, Díaz N, Vergara N, et al. National seroprevalence of coxiella burnetii in Chile, 2016–2017. Pathogens. 2021;10:531. DOIPubMedGoogle Scholar
- Gidding HF, Peng CQ, Graves S, Massey PD, Nguyen C, Stenos J, et al. Q fever seroprevalence in Australia suggests one in twenty people have been exposed. Epidemiol Infect. 2020;148:
e18 . DOIPubMedGoogle Scholar - Bailly S, Hozé N, Bisser S, Zhu-Soubise A, Fritzell C, Fernandes-Pellerin S, et al. Transmission dynamics of Q fever in French Guiana: A population-based cross-sectional study. Lancet Reg Health Am. 2022;16:
100385 . DOIPubMedGoogle Scholar - McCaughey C, McKenna J, McKenna C, Coyle PV, O’Neill HJ, Wyatt DE, et al. Human seroprevalence to Coxiella burnetii (Q fever) in Northern Ireland. Zoonoses Public Health. 2008;55:189–94. DOIPubMedGoogle Scholar
- Tshokey T, Stenos J, Durrheim DN, Eastwood K, Nguyen C, Graves SR. Seroprevalence of rickettsial infections and Q fever in Bhutan. PLoS Negl Trop Dis. 2017;11:
e0006107 . DOIPubMedGoogle Scholar - Jaubert J, Naze F, Camuset G, Larrieu S, Pascalis H, Guernier V, et al. Seroprevalence of Coxiella burnetii (Q fever) exposure in humans on Reunion Island. Open Forum Infect Dis. 2019;6:
ofz227 . DOIPubMedGoogle Scholar - Obaidat MM, Malania L, Imnadze P, Roess AA, Bani Salman AE, Arner RJ. Seroprevalence and risk factors for Coxiella burnetii in Jordan. Am J Trop Med Hyg. 2019;101:40–4. DOIPubMedGoogle Scholar
- Psaroulaki A, Hadjichristodoulou C, Loukaides F, Soteriades E, Konstantinidis A, Papastergiou P, et al. Epidemiological study of Q fever in humans, ruminant animals, and ticks in Cyprus using a geographical information system. Eur J Clin Microbiol Infect Dis. 2006;25:576–86. DOIPubMedGoogle Scholar
- Amitai Z, Bromberg M, Bernstein M, Raveh D, Keysary A, David D, et al. A large Q fever outbreak in an urban school in central Israel. Clin Infect Dis. 2010;50:1433–8. DOIPubMedGoogle Scholar
- Steiner HA, Raveh D, Rudensky B, Paz E, Jerassi Z, Schlesinger Y, et al. Outbreak of Q fever among kitchen employees in an urban hospital. Eur J Clin Microbiol Infect Dis. 2001;20:898–900. DOIPubMedGoogle Scholar
- Oren I, Kraoz Z, Hadani Y, Kassis I, Zaltzman-Bershadsky N, Finkelstein R. An outbreak of Q fever in an urban area in Israel. Eur J Clin Microbiol Infect Dis. 2005;24:338–41. DOIPubMedGoogle Scholar
- Kampschreur LM, Dekker S, Hagenaars JCJP, Lestrade PJ, Renders NHM, de Jager-Leclercq MGL, et al. Identification of risk factors for chronic Q fever, the Netherlands. Emerg Infect Dis. 2012;18:563–70. DOIPubMedGoogle Scholar
- Melenotte C, Protopopescu C, Million M, Edouard S, Carrieri MP, Eldin C, et al. Clinical Features and Complications of Coxiella burnetii Infections From the French National Reference Center for Q Fever. JAMA Netw Open. 2018;1:
e181580 . DOIPubMedGoogle Scholar - Finn T, Babushkin F, Geller K, Alexander H, Paikin S, Lellouche J, et al. Epidemiological, clinical and laboratory features of acute Q fever in a cohort of hospitalized patients in a regional hospital, Israel, 2012-2018. PLoS Negl Trop Dis. 2021;15:
e0009573 . DOIPubMedGoogle Scholar - Ghanem-Zoubi N, Paul M, Szwarcwort M, Agmon Y, Kerner A. Screening for Q fever in patients undergoing transcatheter aortic valve implantation, Israel, June 2018–May 2020. Emerg Infect Dis. 2021;27:2205–7. DOIPubMedGoogle Scholar
- Ghanem-Zoubi N, Karram T, Kagna O, Merhav G, Keidar Z, Paul M. Q fever vertebral osteomyelitis among adults: a case series and literature review. Infect Dis (Lond). 2021;53:231–40. DOIPubMedGoogle Scholar
- Pijnacker R, Reimerink J, Smit LAM, van Gageldonk-Lafeber AB, Zock JP, Borlée F, et al. Remarkable spatial variation in the seroprevalence of Coxiella burnetii after a large Q fever epidemic. BMC Infect Dis. 2017;17:725. DOIPubMedGoogle Scholar
- Israelli Central Bureau of Statistics. Data from the Agricultural Census 2017 [cited 2023 Feb 13]. https://www.cbs.gov.il/en/publications/Pages/2021/Data-from-Agricultural-Census-2017.aspx
- Nusinovici S, Hoch T, Brahim ML, Joly A, Beaudeau F. The effect of wind on Coxiella burnetii transmission between cattle herds: a mechanistic approach. Transbound Emerg Dis. 2017;64:585–92. DOIPubMedGoogle Scholar
- Clark NJ, Soares Magalhães RJ. Airborne geographical dispersal of Q fever from livestock holdings to human communities: a systematic review and critical appraisal of evidence. BMC Infect Dis. 2018;18:218. DOIPubMedGoogle Scholar
- D’Ugo E, Sdanganelli M, Grasso C, Magurano F, Marcheggiani S, Boots B, et al. Detection of Coxiella burnetii in urban river water. Vector Borne Zoonotic Dis. 2017;17:514–6. DOIPubMedGoogle Scholar
- Ghanem-Zoubi N, Pessah Eljay S, Anis E, Paul M. Reemergence of human brucellosis in Israel. Isr Med Assoc J. 2019;21:10–2.PubMedGoogle Scholar
- Dabaja-Younis H, Atarieh M, Paul M, Nasrallah E, Geffen Y, Kassis I, et al. Predictive factors for focal disease in human brucellosis, an observational cohort study. Eur J Clin Microbiol Infect Dis. 2023;42:221–6. DOIPubMedGoogle Scholar
Figure
Tables
Cite This Article1These authors contributed equally to this article.
Table of Contents – Volume 30, Number 5—May 2024
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Nesrin Ghanem-Zoubi, Infectious Diseases Institute, Rambam Health Care Campus, Ha-Aliya 8 St, Haifa 3109601, Israel
Top