Volume 31, Number 3—March 2025
Research Letter
Identification of 2 Novel Species, Mycobacterium novusgordonae and M. shingordonae
Abstract
We identified 2 novel species, Mycobacterium novusgordonae and M. shingordonae, from sputum specimens of pulmonary disease patients in Japan. Genetic and biochemical analyses revealed a close relationship with M. paragordonae. One M. shingordonae case-patient experienced severe progressive infection, highlighting the variation in pathogenicity of the M. gordonae clade species.
We report identification of Mycobacterium novusgordonae and M. shingordonae, 2 novel species in the M. gordonae clade, in sputum specimens from 5 patients with chronic respiratory disease in Japan. Written informed consent was obtained from all the participants at enrollment. The ethics board of the National Hospital Organization, Osaka Toneyama Medical Center approved the whole-genome sequencing (WGS) analysis of Mycobacterium culture isolates (TNH-R-2020020).
During 2021–2024, staff of Toneyama Medical Center (Osaka, Japan), detected novel mycobacteria strains from 3 patients receiving treatment or follow-up for nontuberculous mycobacterial pulmonary disease caused by other species, 1 patient with a clinical diagnosis of nontuberculous mycobacterial pulmonary disease, and 1 immunocompetent patient with progressive pulmonary infectious disease. Here, we discuss the course of illness and testing for the immunocompetent patient (strain MS1); the other patients are described in the Appendix.
A 68-year-old woman with a history of chronic gastritis and allergic rhinitis sought care for a chronic productive cough. Chest computed tomography revealed centrilobular nodules and bronchiectasis in the middle and bilateral lower lobes (Appendix Figure 2). Acid-fast bacilli were detected in 61 sputum culture tests. M. gordonae was identified 3 times with DNA–DNA hybridization assays (Kyokuto Pharmaceutical Industrial, https://www.kyokutoseiyaku.co.jp), 13 times using AccuProbe (Gen-Probe Inc., https://www.hologic.com), and 1 time using matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry (Bruker Daltonics, https://www.bruker.com). No other pathogenic bacteria were detected.
The patient initially started clarithromycin monotherapy; her condition progressively worsened. When she was 75 years of age, a left pneumothorax developed that required drainage. At 77 years of age, her providers switched her treatment to erythromycin from clarithromycin because of gastrointestinal intolerance. Despite worsening respiratory symptoms (productive cough, hemoptysis, and dyspnea) and radiologic findings (Appendix Figure 2), she declined the recommended multidrug therapy because of concerns about adverse effects.
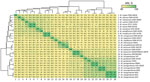
We performed MALDI-TOF mass spectrometry, culture of sputum samples, whole-genome sequencing (WGS), and phylogenetic analysis on all 5 identified strains. MALDI-TOF mass spectrometry identified 2 of the strains as M. gordonae and the other 3 strains as unidentified. We processed sputum samples in accordance with the guidance in Clinical Microbiology Procedures Handbook, 5th edition (1). After processing, we cultured sputum samples on Ogawa medium at 36°C or in mycobacteria growth indicator tube (MGIT) media at 37°C using a BACTEC MGIT 960 system (BD, https://www.bd.com) (2). We subsequently pure-cultured 5 strains on Ogawa medium, analyzed them by WGS, and classified them into 2 groups, MN1/MN2 and MS1/MS2/MS3. Genetic similarity was 99.9%–100% between MN1 and MN2 and 99.1%–100% among MS1, MS2, and MS3. All 5 strains showed an average nucleotide identity (ANI) <95% with the closest known species, M. paragordonae (Figure). Phylogenetic analysis showed that the 5 strains and M. paragordonae belong to different lineages from M. gordonae; however, their mutual relationships are unclear (Appendix Table 1, Figure 1).
WGS confirmed that the MS1 isolates collected at 3 different time points and the MS2 isolates collected at 2 different time points belong to the same species (ANI of MS1, 99.1%–100.0%; of MS2, 100.0%). The new species to which MN1 and MN2 belong was named M. novusgordonae, strain type MN1 (TY813, RIMD 1378001, and CIP 11419T), and the other new species to which MS1, MS2, and MS3 belong was named M. shingordonae strain type MS1 (TY814; RIMD 1379001; CIP 11420T) (Appendix). Novus in Latin and shin in Japanese both mean new.
M. gordonae is an environmental acid-fast bacterium traditionally considered to have low virulence and pathogenicity; it primarily causes opportunistic infections in immunocompromised persons (3). However, recent studies have identified diverse novel species within this clade, revealing distinct patterns of pathogenicity (4–7).
We determined MICs on the basis of recommendations of the Clinical and Laboratory Standards Institute (8). Of note, the MN1–2 and MS2–3 strains exhibit low MICs for clarithromycin, ethambutol, and rifampin, whereas the MS1 strain showed high MIC for clarithromycin, in parallel with the detection of an A2058G mutation in the rrl gene. We performed biochemical tests on 4 strains: MN1 (M. novusgordonae type strain), MS1 (M. shingordonae type strain), M. paragordonae (RIMD 1369002, CIP 112418), and M. gordonae (ATCC 14470T) (Table; Appendix Table 3). The MN1 and MS1 strains were nearly identical; they had similar characteristics as M. paragordonae but were distinct in their ability to grow at 37°C. MN1 and MS1 isolates and M. paragordonae were positive for nitrate reduction. All strains showed positive reactions for catalase, 3-day arylsulfatase, and telluric acid reduction tests.
In conclusion, we identified 2 novel mycobacteria species within the M. gordonae clade that are more closely related to M. paragordonae than to M. gordonae. One patient experienced a progressive infection, revealing the pathogenicity of this novel strain and diversity within the M. gordonae clade.
Dr. Hashimoto is a clinical fellow in respiratory medicine in the Respiratory Medicine department of Osaka University Medical Hospital, Osaka, Japan. His primary research interest is respiratory infections.
Acknowledgments
We thank the patients for granting permission to publish their information. We thank Lisa Oberding for editing a draft of this manuscript.
Availability of data and materials: The datasets supporting the conclusions of this article are included within the article. Whole-genome sequences were deposited in the National Center for Biotechnology Information RefSeq assembly database: MN1 (TY813), accession no. GCF_030755155.1; MN2, accession no. GCF_046643285.1; MS1 (TY814), accession no. GCF_030755175.1; MS2 (TY815), accession no. GCF_030755135.1; and MS3, accession no. GCF_046643305.1.
This work was supported in part by Japan Agency for Medical Research and Development (grant nos. JP20fk0108129, JP21fk0108129h0702, JP21lm0203007), a GlaxoSmithKline Research grant (grant no.A-32), JSPS KAKENHI (grant nos. JP21K16118, JP21K08194), Takeda Science Foundation, Uehara Memorial Foundation, MSD Life Science Foundation, Japanese Respiratory Society Boehringer Ingelheim Research Grant Program, Foundation of Kinoshita Memorial Enterprise, Senri Life Science Foundation, Inamori Foundation, and the Japan Intractable Diseases (Nanbyo) Research Foundation (grant no. 2020B02). The funders had no role in the study design, collection, analyses, or interpretation of data, writing of the manuscript, or decision to publish the results.
Author contributions: K.F. designed the study; H.S., J.Y., and T.N. performed mycobacterial culture and analysis of culture isolates; K.F., K.H., and Y.A. performed clinical and laboratory data extraction and analysis; Y.A., T.N., T.M., K.T., and K.M. assisted with data extraction and analysis; Y.M., D.M., and S.N. performed multilocus typing analysis and whole-genome analysis; M.T. analyzed biochemical profiles of the strain; K.H., Y.A., K.F., and S.N. wrote the manuscript; H.K. supervised the study. All authors read and approved the manuscript.
References
- Leber AL, Burnham C-AD. Mycobacteriology and antimycobacterial susceptibility testing. In: Clinical microbiology procedures handbook, 5th edition. Wayne (PA): Clinical and Laboratory Standards Institute; 2023.
- Lee JJ, Suo J, Lin CB, Wang JD, Lin TY, Tsai YC. Comparative evaluation of the BACTEC MGIT 960 system with solid medium for isolation of mycobacteria. Int J Tuberc Lung Dis. 2003;7:569–74.PubMedGoogle Scholar
- Eckburg PB, Buadu EO, Stark P, Sarinas PS, Chitkara RK, Kuschner WG. Clinical and chest radiographic findings among persons with sputum culture positive for Mycobacterium gordonae: a review of 19 cases. Chest. 2000;117:96–102. DOIPubMedGoogle Scholar
- Kim BJ, Hong SH, Kook YH, Kim BJ. Mycobacterium paragordonae sp. nov., a slowly growing, scotochromogenic species closely related to Mycobacterium gordonae. Int J Syst Evol Microbiol. 2014;64:39–45. DOIPubMedGoogle Scholar
- Mei YM, Zhang Q, Zhang WY, Jiang HQ, Shi Y, Xiong JS, et al. Isolation of novel Mycobacterium species from skin infection in an immunocompromised person. Emerg Infect Dis. 2021;27:2944–7. DOIPubMedGoogle Scholar
- Armstrong DT, Eisemann E, Parrish N. A brief update on mycobacterial taxonomy, 2020 to 2022. J Clin Microbiol. 2023;61:
e0033122 . DOIPubMedGoogle Scholar - Liu G, Yu X, Luo J, Hu Y, Dong L, Jiang G, et al. Mycobacterium vicinigordonae sp. nov., a slow-growing scotochromogenic species isolated from sputum. Int J Syst Evol Microbiol. 2021;71:71. DOIPubMedGoogle Scholar
- Woods GL, Brown-Elliott BA, Conville PS, Desmond EP, Hall GS, Lin G, et al. Susceptibility testing of Mycobacteria, Nocardiae, and other aerobic Actinomycetes. Wayne (PA): Clinical and Laboratory Standards Institute; 2011 Mar. Report no.: M24–A2.
Figure
Table
Cite This ArticleOriginal Publication Date: February 21, 2025
1These authors contributed equally to this article.
Table of Contents – Volume 31, Number 3—March 2025
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Kiyoharu Fukushima, Department of Respiratory Medicine and Clinical Immunology, Osaka University Graduate School of Medicine, 2-2 Yamadaoka, Suita, Osaka, Japan
Top