Volume 17, Number 8—August 2011
Dispatch
Enterovirus 68 in Children with Acute Respiratory Tract Infections, Osaka, Japan
Cite This Article
Citation for Media
Abstract
Enterovirus 68 strains were detected in 14 specimens from children with respiratory tract infections and 1 specimen from a child with febrile convulsions during 2010 in Osaka, Japan. These strains had deletions in the 5′ untranslated region and were genetically different from reported strains. This virus is associated with respiratory tract infections in Japan.
Enterovirus 68 (EV68) belongs to the family Picornaviridae, genus Enterovirus, and species Human enterovirus D (1). EV68 was isolated from 4 children with pneumonia and bronchiolitis in the United States in 1962 (prototype Fermon strain) (2,3) and is associated with respiratory tract infections (RTIs) (3–5). The most common age group for infection with EV68 is 1–4 years of age, but ≈25% of EV68 cases occur in adults >20 years of age (5).
Because of its acid sensitivity and low optimum growth temperature (33°C), EV68 shares characteristics with human rhinovirus (HRV) (3,6) and is genetically and antigenically similar to HRV 87 (6,7). During 1970–2005, only 26 EV68 strains were detected in the United States (5). Fourteen detections of EV68 were reported during 2006–2009 in Japan: 2 in 2006, 8 in 2007, and 4 in 2009 (8). EV68 is rarely detected in Japan, and no epidemics have been reported. We report deletions in genomes of EV68 strains detected in Japan.
During October 2009–October 2010, a total of 448 respiratory specimens were obtained from 448 patients (258 male patients and 190 female patients) with RTIs and fevers in a virus surveillance system in Osaka, Japan (9). The mean ± SD age of the patients was 41.4 ± 53.7 months (range <1–404 months), and 351 (78.3%) were <5 years of age.
Procedures for viral nucleic acid extraction and cDNA synthesis have been reported (9). PCR for detecting HRV and enterovirus was conducted by using EVP4 and OL68-1 primers, which detected HRV and human enterovirus, respectively, in amplicons of ≈530 and 650 bp, respectively (7).
Results showed 178 positive specimens (140 for HRV, 16 for human enterovirus, 7 for HRV and human enterovirus, and 15 for an unexpected amplicon of ≈600 bp). To identify the 600-bp amplicon, we sequenced viral protein 4 (VP4) and VP1 genes. BLAST analysis (www.ncbi.nlm.nih.gov/) showed that these isolates had high identity with EV68 VP4 (98.5%–99.5% with the Pav254–26868 strain [GenBank accession no. HM370293]) and VP1 (96.7%–97.5% with the MD02–1 strain [GenBank accession no. AY426491]). Therefore, these isolates were EV68 positive.
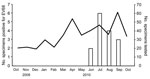
EV68 was not detected in virus isolation tests with Vero and RD-18S cells. EV68 was detected during June–September 2010 (Figure 1). Characteristics of 15 EV68-positive patients are shown in Table 1. Phylogenetic analysis using VP1 sequences (14 of 15 Osaka strains were sequenced) demonstrated that Osaka strains were clustered in 1 group and differed from previously reported strains (Figure 2).
Nucleotide and amino acid identities among 4 Osaka EV68 (JPOC10-290, 378, 396, and 404 strains; nt 501–7265 corresponding to the 37–99 strain), Fermon, and 37–99 strains were determined. To determine sequences, we synthesized cDNA by using specific primers and amplified 4 segments (nt 160–1153, 543–3391, 3132–4032, and 3747–7333 corresponding to the 37–99 strain). The Fermon and 37–99 strains are the only EV68 strains for which complete genome sequences are available. The 37–99 strain was isolated from a 6-year-old girl with pneumonia in 1998 (H. Norder, pers. comm.). The sequenced region coded partial 5′ untranslated regions (UTRs) and all structural and nonstructural viral proteins (VP4–3D). Identities between strains were calculated by using BioEdit version 7.09 (www.mbio.ncsu.edu/bioedit/bioedit.html) (Table 2).
Among Osaka strains, nucleotide and amino acid sequences were highly conserved (nt identity 96.5%–100% and aa identity 98.6%–100%). In contrast, Osaka strains had lower similarities with the Fermon strain (nt identity 83.5%–91.7% and aa identity 90.6%–100%) than with the 37–99 strain (nt identity 91.9%–98.4% and aa identity 95.4%–100%). When we compared individual viral proteins in Osaka strains with those in the Fermon strain, no gene except for VP4 showed >90% nt sequence identity; gene 2B showed the lowest identity (83.5%–85.8%). In contrast, the 37–99 strain had >91.9% nt identity with Osaka strains.
Regarding amino acids, <95% identity was observed in VP1, VP2, and VP3 in the Fermon strain, and no genes with <95% aa identity were found in the 37–99 strain in contrast with Osaka strains. Moreover, no integration or deletion of nucleotides was observed in VP4–3D sequences among Osaka, Fermon, and 37–99 strains.
To clarify why EV68 Osaka strain genomes were smaller than those of other enteroviruses and the EV68 Fermon strain (7), we aligned the partial 5′ UTR sequences (nt 541–820 corresponding to the Fermon strain) of 4 Osaka, Fermon, and 37–99 strains (Figure A1). Results showed that the Osaka and 37–99 strains had deletions at nt 681–704 and 717–727 in contrast with the Fermon strain. Moreover, a 1-nt deletion in Osaka strains was identified at nt 641 in contrast with the Fermon and 37–99 strains. Only the JPOC10–378 strain had a 1-nt deletion at nt 670.
Because 14 patients with EV68 were detected during 2006–2009 (8), detection of 15 patients with EV68 during a 4-month period suggests an EV68 epidemic in the summer of 2010 in Japan. Phylogenetic analysis with VP1 sequences showed that Osaka strains differed genetically from previously reported strains.
For precise analysis of Osaka, Fermon, and 37–99 strains, nucleotide and amino acid sequences were compared in all viral proteins. Results showed that Osaka strains more closely resembled the 37–99 strain than the Fermon strain. Alignment of partial 5′ UTR sequences showed that Osaka and 37–99 strains had deletions in 2 regions in contrast with the Fermon strain, and the amplicon was shorter than expected. Moreover, Osaka strains had 1-nt deletions in contrast with the 37–99 strain.
The 5′ UTR of enterovirus contains an internal ribosome entry site (10) that is associated with translational efficiency and virulence of the enterovirus (11,12). Deleted regions of Osaka strains appear to be in the flanking region between the internal ribosome entry site and an open reading frame (1). Detection of EV68 in numerous patients was reported in France during 2008 (4) and Italy during 2008–2009 (13). Because this deletion was found in the 37–99 strain in 1998, recent detection of EV68 in Japan might be associated with this change in the viral genome. Smura et al. reported that serum samples from 281 pregnant women in Finland in 1983, 1993, and 2002 had high titers of neutralizing antibody against EV68 (14). This result indicates that EV68 has been in Finland since 1983.
All EV68-positive patients in this study were <5 years of age and had lower respiratory tract inflammation. Seroepidemiologic studies in Finland showed that most adults might have been previously infected with EV68 and therefore might have neutralizing antibodies (14). Increased detection of EV68, especially in infants and children, will provide useful epidemiologic data.
Recent studies showed that EV68-infected human leukocytes produced infectious progeny virus (14). This result indicates that EV68 can replicate in blood and may damage the central nervous system. EV68 was detected in cerebrospinal fluid of a young adult patient with acute flaccid paralysis (5). Epidemiologic data for EV68 are lacking, and little information is available regarding virologic characteristics. If one considers results of phylogenetic analyses and nucleotide and amino acid identities, evolutionary changes might have occurred in EV68. Our results show the potential role of EV68 infection in infants and children with RTIs.
Dr Kaida is a research scientist at Osaka City Institute of Public Health and Environmental Sciences. His primary research interest is acute viral RTIs in young children.
Acknowledgments
We thank Kaoru Goto and Atsushi Hase for their support during the study.
This study was supported in part by a Grant-in-Aid for Young Scientists (B) (21790600) from The Ministry of Education, Culture, Sports, Science, and Technology of Japan.
References
- Pallansch M, Roos R. Enteroviruses: polioviruses, echoviruses, and newer enteroviruses. In: Fields BN, Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin MA, et al., editors. Fields virology. 5th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2007.
- Schieble JH, Fox VL, Lennette EH. A probable new human picornavirus associated with respiratory diseases. Am J Epidemiol. 1967;85:297–310.PubMedGoogle Scholar
- Oberste MS, Maher K, Schnurr D, Flemister MR, Lovchik JC, Peters H, Enterovirus 68 is associated with respiratory illness and shares biological features with both the enteroviruses and the rhinoviruses. J Gen Virol. 2004;85:2577–84. DOIPubMedGoogle Scholar
- Petitjean-Lecherbonnier J, Dina J, Nguyen E, Gouarin S, Lebigot E, Vabret A. Molecular diagnosis of respiratory enterovirus infections: use of PCR and molecular identification for a best approach of the main circulating strains during 2008 [in French]. Pathol Biol (Paris). 2011;59:113–21. DOIPubMedGoogle Scholar
- Khetsuriani N, Lamonte-Fowlkes A, Oberst S, Pallansch MA. Enterovirus surveillance—United States, 1970–2005. MMWR Surveill Summ. 2006;55:1–20.PubMedGoogle Scholar
- Blomqvist S, Savolainen C, Raman L, Roivainen M, Hovi T. Human rhinovirus 87 and enterovirus 68 represent a unique serotype with rhinovirus and enterovirus features. J Clin Microbiol. 2002;40:4218–23. DOIPubMedGoogle Scholar
- Ishiko H, Miura R, Shimada Y, Hayashi A, Nakajima H, Yamazaki S, Human rhinovirus 87 identified as human enterovirus 68 by VP4-based molecular diagnosis. Intervirology. 2002;45:136–41. DOIPubMedGoogle Scholar
- Infectious Agents Surveillance Report. Yearly reports of virus isolation/detection from human sources, 2006–2010 [cited 2011 Jan 2]. http://hasseidoko.mhlw.go.jp/Byogentai/Pdf/data60e.pdf
- Kaida A, Kubo H, Shiomi M, Kohdera U, Iritani N. Evaluation of real-time RT-PCR compared with conventional RT-PCR for detecting human metapneumovirus RNA from clinical specimens. Jpn J Infect Dis. 2008;61:461–4.PubMedGoogle Scholar
- Martínez-Salas E, Pacheco A, Serrano P, Fernandez N. New insights into internal ribosome entry site elements relevant for viral gene expression. J Gen Virol. 2008;89:611–26. DOIPubMedGoogle Scholar
- De Jesus N, Franco D, Paul A, Wimmer E, Cello J. Mutation of a single conserved nucleotide between the cloverleaf and internal ribosome entry site attenuates poliovirus neurovirulence. J Virol. 2005;79:14235–43. DOIPubMedGoogle Scholar
- Dunn JJ, Bradrick SS, Chapman NM, Tracy SM, Romero JR. The stem loop II within the 5′ nontranslated region of clinical coxsackievirus B3 genomes determines cardiovirulence phenotype in a murine model. J Infect Dis. 2003;187:1552–61. DOIPubMedGoogle Scholar
- Piralla A, Baldanti F, Gerna G. Phylogenetic patterns of human respiratory picornavirus species, including the newly identified group C rhinoviruses, during 1-year surveillance of a hospitalized patient population in Italy. J Clin Microbiol. 2011;49:373–6. DOIPubMedGoogle Scholar
- Smura T, Ylipaasto P, Klemola P, Kaijalainen S, Kyllonen L, Sordi V, Cellular tropism of human enterovirus D species serotypes EV-94, EV-70, and EV-68 in vitro: implications for pathogenesis. J Med Virol. 2010;82:1940–9. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleTable of Contents – Volume 17, Number 8—August 2011
| EID Search Options |
|---|
|
|
|
|
|
|


Please use the form below to submit correspondence to the authors or contact them at the following address:
Atsushi Kaida, Department of Microbiology, Osaka City Institute of Public Health and Environmental Sciences, 8-34 Tojo-cho, Tennoji-ku, Osaka 543-0026, Japan
Top