Volume 2, Number 4—October 1996
Dispatch
Experimental Inoculation of Plants and Animals with Ebola Virus
Cite This Article
Citation for Media
Abstract
Thirty-three varieties of 24 species of plants and 19 species of vertebrates and invertebrates were experimentally inoculated with Ebola Zaire virus. Fruit and insectivorous bats supported replication and circulation of high titers of virus without necessarily becoming ill; deaths occurred only among bats that had not adapted to the diet fed in the laboratory.
The taxonomy of the Filoviridae is in a state of flux; the family includes viruses currently designated Marburg, Ebola Zaire, Ebola Sudan, and Ebola Ivory Coast, which are believed to be endemic to Africa, and Ebola Reston, which putatively originates in the Philippines (1,2). The viruses are known particularly for their propensity to cause fatal hemorrhagic disease of humans with person-to-person spread, but their pathogenicity varies from asymptomatic infection (Ebola Reston) to epidemics with death rates of 77% to 88% (Ebola Zaire) (1,3). All of the viruses appear to be highly pathogenic for nonhuman primates. Outbreaks of disease have occurred in Europe and North America in monkeys imported from Africa and the Philippines, sometimes with spread of infection to humans (1). Contact with the tissues of dead nonhuman primates was a source of infection for humans on at least two occasions in Africa (2,4). Nevertheless, the lethality of the viruses for nonhuman primates suggests that, like humans, nonhuman primates are incidental victims of infection and are not true reservoir hosts (1). The source of filoviruses in nature remains unknown, but in some instances, bats roosted in buildings or a cave visited or frequented by people who subsequently were found to have primary cases of infection in outbreaks of disease in Africa; one patient was bitten or stung by what is presumed to have been an arthropod 7 days before coming down with Marburg disease (1). Informal speculation has included the suggestion that filoviruses may be plant viruses, perhaps even involving transmission by arthropod vectors.
The search for the source of the viruses in nature has been hampered by the erratic recognition of outbreaks of filovirus infection in widely separated geographic locations at unpredictable intervals; therefore, comparatively few field investigations have been reported (1). After the 1995 epidemic of Ebola fever in Kikwit, Zaire, teams of scientists coordinated by the Centers for Disease Control and Prevention, Atlanta, and the U.S. Army Medical Research Institute of Infectious Diseases, Fort Detrick, collected large numbers of vertebrate and arthropod specimens during June, July, and August, 1995. Because evidence indicated that the outbreak had actually started in January 1995, it was possible that the virus was no longer circulating in its natural hosts in the vicinity of Kikwit by the time ecologic studies were undertaken. To allow for the possibility that the filoviruses manifest seasonal activity in their natural hosts, a team from the National Institute for Virology (NIV) in South Africa visited Kikwit in January 1996, to trap wild vertebrates and arthropods in the sites investigated by the other teams in mid-1995. Testing of the field material is a lengthy process, and no filoviruses have been detected so far. We decided to narrow the search by performing pathogenicity studies with Ebola virus in representatives of different classes and orders of living things, including vertebrates, invertebrates, and even plants. The underlying assumptions were that if a group of species is either refractory or hypersusceptible to the virus, members of the taxon are unlikely reservoir hosts of the virus, whereas members of taxa capable of circulating virus for prolonged periods without becoming ill are suspected reservoirs.
The strain of Ebola Zaire virus used in the experiments, Zaire-95, had been isolated from the blood of a patient in the 1995 epidemic in Kikwit and designated as the prototype strain of the outbreak. Stocks were prepared from virus at pass level 4 in Vero V76 cell cultures by freeze-thawing infected cultures, clarifying the supernatant culture fluid at 3,000g, and storing it in small volumes at -70°C. Virus titers were determined by fluorescent focus assay in 8-chamber slide cultures as described for rabies (5), except that Vero cells were used, and cultures were stained with immune mouse ascitic fluid followed by fluorescein-labeled anti-mouse immunoglobulin and read on day 3 to 5 postinoculation to detect infected foci. Inoculum volumes of 10µl of 10-fold serial dilutions of stock virus or tissue suspensions were adsorbed to cultures, and titers were expressed as fluorescent focus-forming units (FFU) per ml.
One-month-old potted seedlings of 33 varieties of 24 species of weeds and crop plants used in plant virology (Table 1), plus colonized leafhoppers, were obtained from Dr. G. Pietersen of the Plant Protection Research Institute (PPRI) at Rietondale, Pretoria, South Africa. The plants were selected because collectively they could provide culture substrates for a broad spectrum of the known viruses of economically important plants. They were kept under suitable lighting for 10 hours each day and watered as necessary to sustain growth in the laboratory. Pigeons were obtained from the South African Institute for Medical Research in Johannesburg; 1- to 3-month-old hatchling snakes from the Transvaal Snake Park, Midrand; cockroaches from a colony at the Bureau of Standards in Pretoria; and Mastomys natalensis and NIH mice from colonies at NIV. All other animals used in the studies (Table 2) were collected in the Kruger National Park, South Africa, with the permission of the National Parks Board as part of a long-standing research project on hemorrhagic fever viruses. The animals were translocated from the park under permit from the Department of Veterinary Services, and the experiments were conducted in a biosafety level 4 containment laboratory at NIV with clearance from the Department of Agriculture, Conservation and Environment of Gauteng Province, and the Animal Ethics Committee of NIV. All animals were fed a diet similar to their natural diets and were provided with fresh drinking water daily.
Vertebrates were inoculated subcutaneously with 0.1 ml of stock virus diluted 1:10 in cell culture medium, and back titration of the inoculum indicated that each animal received a dose of 40,000 or 104.6 FFU virus. Invertebrates were inoculated with undiluted stock virus and received approximately 1.0µl containing 4,000 or 103.6 FFU of virus, except for leafhoppers, which received about 0.3µl inoculum. The arthropods were inoculated intrathoracically (6), except for ants and millipedes, which were inoculated into the hemocoel through the membranous integument between tergites. To simulate mechanical transmission, undiluted stock virus mixed with Carborundum powder was rubbed gently with cotton buds onto two leaves on each of the plant varieties on experiment; to simulate vector-borne transmission, a second plant of each type was inoculated with 1.0µl virus suspension into the phloem of the stem, using the same apparatus as for arthropods. A third plant of each type served as control. Plants were observed daily and those that wilted or developed apparent lesions were harvested; some material was fixed in 2.5% glutaraldehyde in buffer for examination by electron microscopy, and the rest was stored at -70°C for virus assay. The process of embedding, sectioning, and examining the plant tissues by electron microscopy was performed by H.J. van Tonder of PPRI. Animals were sacrificed and assayed for virus content either in pools or individually, before inoculation and at intervals postinoculation (Table 2). Serum and pooled visceral organs were tested separately, and individual organ samples were preserved at -70°C and in Formalin fixative for more detailed study later. Urine and feces samples were tested on some occasions. Materials for virus assay were prepared as 10% suspensions in culture medium, and in parallel with attempts to titrate infectivity, 0.1 ml volumes were injected into Vero cell monolayers in 25 cm2 flasks, which were subcultured thrice at weekly intervals before specimens were recorded as negative.
Thirteen plants either wilted or developed lesions on the leaves ascribed to mechanical injury during the inoculation process, but no infectivity could be recovered from the tissues, and no evidence of virus infection was observed by electron microscopy. All animal experiments (Table 2) were performed in parallel on a single occasion except for a second experiment with insectivorous bats (Tadarida spp.). Insectivorous bats had difficulty in adapting to a laboratory diet, and consequently 10 of 18 died in the first experiment. Although virus was recovered from the blood and organs of some, no histopathologic lesions were observed, and no evidence of widespread infection was detected by immunohistochemical technique (7). All of the bats that died had not been eating well, and hence more insectivorous bats (T. pumila) were collected from the same colony as before and adapted to a diet of mealworms over a period of 3 weeks before inoculation. The bats in the second experiment received the same dose of virus as the previous group, and no deaths occurred before the 12 animals in the study, including nine that were kept 21 to 28 days, were sacrificed (Table 2). None of the other vertebrates died, although some of the ants, cockroaches, and spiders died, possibly from desiccation as a result of injury during inoculation.
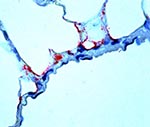
The virus replicated in bats: titers of 104.6-107.0 FFU/ml were recorded in sera and titers of 102.0-106.5 FFU/ml in pooled viscera of fruit bats. In addition, virus was recovered from the feces of a fruit bat on day 21 postinoculation. Virus was also recovered on a few occasions from snakes, and NIH mice and spiders (Table 2), but this was at a minimal titer of 101.0 FFU/ml and could represent residual infectivity from inoculation. Histopathologic and immunohistochemical investigations have thus far been limited to some sets of the bat organs, and the only virus antigen detected was present in the endothelial cells of lung tissue of a bat sacrificed on day 8 postinoculation (Figure). Four insectivorous bat sera collected on day 28 postinoculation and four samples from noninfected bats were tested for Ebola virus antigen or antibody by enzyme-linked immunoassay (8) using conjugated chicken anti-rodent immunoglobulin; antibody was found in only one of the infected bats.
Although they do not provide conclusive evidence that bats are potential reservoir hosts of filoviruses or that the other animals are not, the findings demonstrate the validity of the experimental approach to the search for the source of the viruses in nature. If it can be shown, for instance, that a further two to three species of birds of widely divergent orders or families are refractory to the virus, birds can be accorded low priority in field studies, and efforts can be concentrated on animals capable of circulating virus. Even if evidence is obtained that certain animals become infected in the field, it would remain desirable to study the nature of the infection they undergo in the laboratory to determine whether they can harbor virus for prolonged periods and transmit it to other animals. Additionally, materials derived from the experiments can be used to develop, test, and perfect methods for detecting infectious virus, viral antigen, nucleic acid, or antibodies in different species, and to establish whether or not demonstrable immune response develops in ostensibly refractory animals. There are no accepted methods for demonstrating antibody in many wild vertebrates; anti-bat immunoglobulin is being produced as part of the present project.
The two tadarids studied here, and many other bats, have a distribution that overlaps the sites of known filovirus outbreaks in Africa, and the migratory habits of some species would facilitate dissemination of virus (9). The presence of virus in lung tissue implies that respiratory or oral spread of infection could occur in the confined spaces where bats roost, and isolation of virus from feces suggests the existence of mechanisms for transmission of infection to other animals. However, much remains to be learned about the nature of the infection in bats, including the sites of virus replication, persistence, and the behavior of the virus in further genera and species.
References
- Peters CJ, Sanchez A, Rollin PE, Ksiazek TG, Murphy FA. Filoviridae: Marburg and Ebola viruses. In: Field's Virology, Philadelphia: Lippincott-Raven. 1996;1161-76.
- Le Guenno B, Formenty P, Wyers M, Gounon P, Walker F, Boesch C. Isolation and partial characterization of a new strain of Ebola virus. Lancet. 1995;345:1271–4. DOIPubMedGoogle Scholar
- Muyembe T, Kipasa M. Ebola haemorrhagic fever in Kikwit, Zaire. Lancet. 1995;345:1448. DOIPubMedGoogle Scholar
- World Health Organization. Outbreak of Ebola haemorrhagic fever in Gabon officially declared over. Wkly Epidemiol Rec. 1996;71:125–6.
- Smith JS, Yager PA, Baer GM. A rapid tissue culture test for determining rabies neutralizing antibody. In: Laboratory techniques in rabies, Geneva: World Health Organization. 1973;354-7.
- Rosen L, Gubler D. The use of mosquitoes to detect and propagate dengue viruses. Am J Trop Med Hyg. 1974;23:1153–60.PubMedGoogle Scholar
- Zaki SR, Greer PW, Goldsmith CS, Coffield LM, Rollin PE, Callain P, Ebola virus hemorrhagic fever: pathologic, immunopathologic and ultrastructural studies. Lab Invest. 1996;:74.
- Ksiazek TG, Rollin PE, Jahrling PB, Johnson E, Dalgard DW, Peters CJ. Enzyme immunosorbent assay for Ebola virus antigens in tissues of infected primates. J Clin Microbiol. 1992;30:947–50.PubMedGoogle Scholar
- Smithers RHN. Chiroptera. In: The mammals of the southern African region, Pretoria: University of Pretoria. 1983;51-137.
Figure
Tables
Cite This ArticleTable of Contents – Volume 2, Number 4—October 1996
| EID Search Options |
|---|
|
|
|
|
|
|