Volume 26, Number 10—October 2020
CME ACTIVITY - Synopsis
Healthcare-Associated Legionnaires’ Disease, Europe, 2008−2017
Introduction

Medscape CME ACTIVITY
In support of improving patient care, this activity has been planned and implemented by Medscape, LLC and Emerging Infectious Diseases. Medscape, LLC is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1.00 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.0 MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) program. Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider's responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 75% minimum passing score and complete the evaluation at http://www.medscape.org/journal/eid; and (4) view/print certificate.
Release date: September 17, 2020; Expiration date: September 17, 2021
Learning Objectives
Upon completion of this activity, participants will be able to:
• Compare different sources of LD in the European Union
• Analyze temporal trends in LD in the European Union
• Assess demographic variables among patients with LD
• Evaluate the microbiology and prognosis of healthcare-associated LD
CME Editor
Deanna Altomara, BA, Copyeditor, Emerging Infectious Diseases. Disclosure: Deanna Altomara, BA, has disclosed no relevant financial relationships.
CME Author
Charles P. Vega, MD, Health Sciences Clinical Professor of Family Medicine, University of California, Irvine School of Medicine, Irvine, California. Disclosure: Charles P. Vega, MD, has disclosed the following relevant financial relationships: served as an advisor or consultant for Johnson & Johnson Pharmaceutical Research & Development, LLC; GlaxoSmithKline; served as a speaker or a member of a speakers bureau for Genentech; GlaxoSmithKline.
Authors
Disclosures: Julien Beauté, PhD; Diamantis Plachouras, PhD; Sven Sandin, PhD; Johan Giesecke, PhD; and Pär Sparén, PhD, have disclosed no relevant financial relationships.
Abstract
Healthcare-associated Legionnaires’ disease (HCA LD) can cause nosocomial outbreaks with high death rates. We compared community-acquired LD cases with HCA LD cases in Europe during 2008−2017 using data from The European Surveillance System. A total of 29 countries reported 40,411 community-acquired and 4,315 HCA LD cases. Of the HCA LD cases, 2,937 (68.1%) were hospital-acquired and 1,378 (31.9%) were linked to other healthcare facilities. The odds of having HCA LD were higher for women, children and persons <20 years of age, and persons >60 years of age. Out of the cases caused by Legionella pneumophila with a known serotype, community-acquired LD was more likely to be caused by L. pneumophila serogroup 1 (92.3%) than was HCA LD (85.1%). HCA LD patients were more likely to die. HCA LD is associated with specific patient demographics, causative strains, and outcomes. Healthcare facilities should consider these characteristics when designing HCA LD prevention strategies.
Legionnaires’ disease (LD) is a severe pneumonia caused by Legionella, a genus of gram-negative bacteria found in aquatic environments and human-made water systems (1). LD is a notifiable condition in all 30 European Union (EU) and European Economic Area (EEA) countries, where ≈70% of reported cases are community-acquired, ≈20% are travel-associated, and ≈10% are healthcare-associated (HCA) (2). In 2015, HCA LD accounted for 20% of all cases in the United States reported to the Centers for Disease Control and Prevention (3). The overall EU–EEA LD notification rate increased during 2011–2017 for unknown reasons (2,4).
Public health professionals should not overlook HCA LD; although it is relatively uncommon, it is associated with nosocomial outbreaks, underdiagnosis, and a high death rate of ≈30% (5–7). During 2006–2017, nearly 25% of identified outbreaks in the United States and several countries in Europe occurred in hospital or healthcare settings (6). During 2005–2009 in the United Kingdom and 2008–2010 in Spain, ≈3%–4% of HCA pneumonia cases were caused by Legionella (8,9). Hospital patients and residents of long-term care facilities are more likely to have LD risk factors, such as older age, chronic conditions, history of organ transplantation, or immunodeficiency (7). As such, hospital patients and residents of long-term care facilities might be more susceptible to Legionella (10).
Inhalation and aspiration are major modes of HCA LD transmission (11); potable water is a common source of infection (7). Because Legionella can colonize hospital water systems, possible sources of nosocomial infection include bathing, steam-heated towels, humidifiers, decorative fountains, and some medical devices (12,13). In children, HCA LD has been reported in association with heated birthing pools (14). HCA LD can be prevented by reducing the colonization of Legionella in hospitals (15). We describe the epidemiology of HCA LD in Europe using EU surveillance data to determine its differences from community‐acquired LD in terms of seasonality, demographics, causative pathogens, and outcomes.
LD Data
The European Legionnaires’ disease Surveillance Network, which comprises Iceland, Norway, and all 28 EU member states, including the United Kingdom, operates under the European Centre for Disease Prevention and Control (Stockholm, Sweden). Each state annually reports its LD cases to The European Surveillance System database hosted by the European Centre for Disease Prevention and Control. Countries report their LD cases with variables such as patient age, patient sex, date of disease onset, probable setting of infection (e.g. travel-associated), whether the case-patient is part of a cluster, laboratory method used for diagnosis, causative pathogen, and clinical outcome. LD patients who travelled (abroad or domestically) 2–10 days before disease onset are considered to have travel-associated LD. Many EU–EEA countries define HCA LD on the basis of whether the patient was in a hospital or healthcare facility <10 days before disease onset (16–18). Community-acquired LD is a diagnosis of exclusion (i.e., non-HCA, non–travel-associated). We defined a locally acquired case as any case not associated with travel.
Our analysis included all locally acquired cases reported during 2008–2017 that met the 2012 EU–EEA case definition of confirmed and probable cases of LD (19). We excluded travel-associated cases because they encompass heterogeneous exposures. We reclassified LD cases reported before 2012 according to the 2012 EU–EEA case definition. We defined hospital-acquired cases as those reported from a hospital, whereas HCA LD cases comprised hospital-acquired cases and cases reported from other healthcare facilities (e.g., nursing homes). We made this distinction for 2 main reasons. First, hospital patients, independent of age, might be immunocompromised and therefore more susceptible to LD. Second, the duration of Legionella exposure might be shorter for patients admitted to the hospital for acute care than for residents of long-term care facilities.
Statistical Analyses
We compared the characteristics of HCA LD patients and community-acquired LD patients. We sorted patients into 8 groups by age at diagnosis (2). We compared their characteristics by using the χ2 test with a 2-sided p value of <0.05. In addition, we used logistic regression to analyze the odds of acquiring HCA or community-acquired LD, the odds of death, and the confounding effects of age and sex.
In a subanalysis of culture-confirmed cases (i.e., cases ascertained by isolation of Legionella spp. from respiratory secretions or any normally sterile site), we compared the causative pathogens of HCA LD patients with community-acquired LD patients. We grouped Legionella isolates by species and monoclonal subtypes; we further classified monoclonal subtypes by the virulence-associated epitope recognized by monoclonal antibody (mAb) 3/1 of the Dresden Panel (10). We further explored the factors associated with outcome in a subset analysis of culture-confirmed cases with information about the causative strain. We used Stata 14 (StataCorp LLC, https://www.stata.com) for all statistical analyses.
During 2008−2017, a total of 30 countries in Europe reported 64,409 LD cases. We excluded 446 (0.7%) of these case-patients because a laboratory method for diagnosis was not reported. We further excluded 6,788 (10.5%) LD patients, including all case-patients from Sweden, because setting of infection was not reported. These exclusions resulted in a preliminary analysis dataset of 57,175 LD patients. Of these, LD for 40,411 (70.7%) were reported as community-acquired, 11,512 (20.1%) as travel-associated, 4,315 (7.5%) as HCA, and 937 (1.6%) as associated with other settings. We then excluded travel-associated cases and those associated with other settings, resulting in our analysis dataset of 44,726 LD patients reported by 29 countries, of whom 40,411 (90.4%) had community-acquired LD and 4,315 (9.6%) had HCA LD (Table 1).
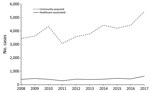
The annual number of locally acquired LD cases fluctuated from 3,357 cases in 2011 to 6,074 in 2017 (Figure 1). During 2011−2017, diagnoses of community-acquired LD and HCA LD increased. The average proportion of HCA LD among all LD cases was 10.7%, fluctuating between 9.3% in 2010 and 12.7% in 2009.
The highest proportions of HCA LD cases occurred in countries that reported <200 locally acquired cases. In Cyprus, Estonia, Hungary, Iceland, Luxembourg, and Poland, this proportion was >25%. Of the countries that reported >200 cases, the highest proportions of HCA LD occurred in Belgium (23.5%), France (15.5%), and Denmark (14.4%). Latvia and Norway did not report any HCA LD cases. Of the 4,315 HCA LD cases, 2,937 (68.1%) were hospital-acquired and 1,378 (31.9%) were linked to other healthcare facilities. Confirmation was slightly higher for community-acquired cases than for HCA LD (94.8% vs. 94.1%; p<0.05). France and Italy reported 2,763 (64.0%) HCA LD cases.
Demographic Data
Of the 4,310 HCA LD patients for whom sex was known, 2,499 (58.0%) were male, resulting in a male:female ratio of 1.4:1. However, the proportion of HCA LD was higher for female LD patients than for male LD patients (14.2% vs. 7.8%; p<0.01). The male:female ratio was lower (0.9:1) for both younger (<20 years of age) and older (>80 years of age) patients; the ratio peaked at 2.2:1 for patients 40–49 years of age. Of the 4,313 HCA LD patients for whom age was known, 2,650 (61.4%) were >70 years of age. The proportion of HCA LD patients >70 years of age was higher for patients linked to other healthcare facilities than for those linked to hospitals (80.0% vs. 52.8%; p<0.01). After adjustment for age, year, and reporting country, women were more likely than men to have acquired their infection in a healthcare facility (odds ratio [OR] 1.60, 95% CI 1.49–1.71) (Table 2). Patients <20 years of age of were twice as likely as patients 50–59 years of age to have HCA LD (OR 2.04, 95% CI 1.25–3.33). The risk for an HCA LD diagnosis increased with age for patients >60 years of age, peaking for patients >80 years of age (OR 4.58, 95% CI 4.11–5.12).
Seasonality
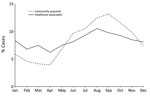
The monthly distribution of onset peaked in August and September for both community-acquired and HCA LD (Figure 2). The proportion of community-acquired LD cases that developed during June–November was greater than that of HCA LD (66.9% vs. 55.8%; p<0.01).
Laboratory Test Results
During 2008–2017, The European Surveillance System recorded 48,197 laboratory test results for the 44,726 LD patients included in this analysis. LD diagnosis by urinary antigen test (UAT) was more common for community-acquired than HCA LD cases (88.7% vs. 84.3%; p<0.01). On the other hand, culture confirmation of LD was more common for HCA LD than community-acquired cases (15.9% vs. 10.4%; p<0.01) (Table 2). Of the 4,884 culture-confirmed cases, 2,205 (45.1%) were also ascertained by UAT.
Among HCA LD cases, the proportion of culture-confirmed cases was higher for hospital-acquired cases than cases linked to other healthcare settings (18.8% vs. 9.7%; p<0.01). PCR diagnosis was more likely for HCA LD than for community-acquired LD (6.8% vs. 5.0%; p<0.01). For both community-acquired and HCA LD, the proportion of cases ascertained on the basis of a single high titer of a specific serum antibody was similar (≈2.5%). The proportion of cases diagnosed by a 4-fold rise in titer or by direct immunofluorescence assay also was similar for both groups (<1% for both tests).
Pathogens
Of the 4,859 culture-confirmed cases reported with a known causative pathogen species, 4,739 (97.5%) were caused by Legionella pneumophila. This proportion was similar for community-acquired and HCA LD cases (97.4% vs. 98.1%; p = 0.31) (Table 3). Of the 4,533 laboratory-confirmed cases of L. pneumophila reported with a known serogroup, 4,137 (91.3%) were caused by L. pneumophila serogroup 1. This proportion was higher for community-acquired cases than HCA LD cases (92.3% vs. 85.1%; p<0.01). Following L. pneumophila serogroup 1 (537/684 culture-confirmed HCA LD), the most common serogroups associated with culture-confirmed HCA LD were L. pneumophila serogroups 3 (33 cases), 6 (15 cases), and 5 (11 cases). Of the 107 community-acquired cases with culture confirmation of other Legionella species, 48 (44.9%) were caused by L. longbeachae. The European Surveillance System did not record any HCA cases of L. longbeachae.
Of the 856 culture-confirmed cases caused by L. pneumophila serogroup 1 for which isolates were subtyped using mAbs, 679 (79.3%) tested positive for mAb 3/1 (Table 4). This proportion was higher for community-acquired than HCA LD (83.6% vs. 43.3%; p<0.01).
Outcomes
Of the 32,379 case-patients with known outcomes, 3,448 (10.6%) died (Table 5). The proportion of patients who died was higher for those with HCA than community-acquired LD (28.8% vs. 8.6%; p<0.01). This proportion was similar for patients with hospital-acquired LD and LD linked to other healthcare facilities (29.2% vs. 28.1%; p = 0.52). After adjustment for age, sex, year, and reporting country, the death rate was higher for HCA than community-acquired LD (OR 3.02, 95% CI 2.75–3.32). The death rate was higher for hospital-acquired LD than for LD linked to other healthcare facilities (OR 3.50, 95% CI 3.14–3.91) (Table 5). After we restricted our analysis to the 4,121 culture-confirmed cases for which information was available about causative species and serogroups, the death rate for HCA LD remained higher than for community-acquired LD (OR 2.60, 95% CI 2.11–3.22). Patients infected by L. pneumophila nonserogroup 1 had a higher risk for death than those infected by L. pneumophila serogroup 1 (OR 2.17, 95% CI 1.61–2.92). Infection with other species was not associated with a higher death rate. Of the 690 culture-confirmed cases caused by L. pneumophila serogroup 1 for which information about monoclonal subtype was available, patients with HCA LD still had a higher death rate than those with community-acquired LD (OR 1.93, 95% CI 1.04–3.58); cases caused by mAb 3/1–negative strains were 4 times more likely to be fatal than those caused by mAb 3/1–positive strains (OR 4.20, 95% CI 2.32–7.61).
Clusters
Of the 31,973 LD patients with known cluster status, 2,039 (6.4%) were part of a cluster. This proportion was higher for HCA LD patients than community-acquired LD patients (10.6% vs. 6.0%; p<0.01).
In this surveillance sample from 29 EU–EEA countries, ≈10% of locally acquired LD cases were HCA. This analysis included >4,300 HCA LD cases reported during a 10-year period, providing a valuable overview of HCA LD epidemiology in Europe. A few countries accounted for most cases, a phenomenon that might limit the generalizability of the results (2,20). Although some countries might have more stringent preventive measures for hospitals, the characteristics of HCA LD patients themselves are unlikely to differ substantially across countries. In addition, we adjusted for the reporting countries in our statistical analyses. Most of the countries with a proportion of HCA LD >25% were also countries with low LD notification rates (<0.5 cases/100,000 population) during 2011–2015 (2). This finding suggests that these countries are better able to diagnose and report HCA than community-acquired LD cases. Some of these countries have reported challenges in ascertaining LD, including lack of clinical awareness, lack of testing, and lack of on-site diagnostic tests (2).
In Europe, HCA LD disproportionately affects older persons; 61.4% of case-patients are >70 years of age. However, HCA LD should not be overlooked in children. LD patients <20 years of age are twice as likely to have HCA LD than patients 50–59 years of age. Although the risk for HCA LD remains higher for men and boys than for women and girls (male:female ratio of 1.4:1), LD in female patients is 60% more likely to be HCA than it is in male patients. Some risk factors for community-acquired LD might be associated with sex. For example, activities that women might be less likely to engage in, such as home plumbing or working in transportation or construction, could be risk factors for LD (21,22).
The incidence of HCA LD varied less by season than it did for community-acquired LD, probably because healthcare facilities are less exposed to external environmental conditions. Legionella spp. often colonize hospital water systems (23). These water systems might offer year-round favorable conditions for Legionella, which multiplies at 25°C–42°C (24).
Legionella spp. causing HCA LD differ from those commonly observed in community-acquired LD. Although L. pneumophila caused most infections regardless of the setting, we observed a lower proportion of L. pneumophila serogroup 1 in HCA LD cases. This discrepancy may be of concern because UAT, the dominant laboratory method used to ascertain LD, has a poor sensitivity to non–L. pneumophila serogroup 1 strains (25). In our study, ≈45% of culture-confirmed cases were also ascertained by UAT. Because we could not determine whether the culture sequentially followed the UAT or whether the tests were performed independently, we might have overestimated the cases caused by L. pneumophila serogroup 1. Of the cases caused by L. pneumophila serogroup 1, mAb 3/1–negative strains were more common in HCA LD patients, whereas mAb 3/1–positive strains were more common in community-acquired LD patients. These results confirm earlier reports that mAb 3/1–negative strains were more frequent in hospital-acquired infections (10). The association of HCA LD with less virulent strains probably reflects patient demographic variables; immunocompromised patients might be more highly concentrated in healthcare facilities than in the general community. Although non–L. pneumophila species caused only a few cases, the proportion of cases caused by those species (except for L. longbeachae, which only causes community-acquired LD and is frequently associated with exposure to composts and potting soils [26]) was higher in patients with HCA than community-acquired LD. Patients with non–L. pneumophila infections might be more likely to be immunocompromised (27).
Nearly 30% of HCA LD patients in this analysis died. The risk for death was 2–3 times higher for HCA LD than for community-acquired LD. Some strains such as MAb 3/1–negative strains were also associated with a higher risk for death, probably because these strains of LD tend to infect more severely ill patients.
The HCA LD diagnosis might mask 2 different populations: younger but more severely ill patients who acquired infection in the hospital and older but less severely ill patients who acquired infection from other healthcare facilities. Hospital-acquired LD might be more likely to affect immunocompromised patients with underlying conditions. The large proportion of non–hospital-acquired LD in patients >70 years of age suggests that many might be residents of long-term care facilities. In these facilities, caretakers might have difficulty obtaining sputum samples or might not suspect LD. Furthermore, microbiology laboratory capacity might be limited (28), as suggested by the low proportion of culture-confirmed cases in these settings.
There is no European standard for defining HCA LD. Epidemiologists in charge of national LD surveillance report LD cases with the probable setting of infection. These reports might misclassify LD patients who were infected in the community but admitted to the hospital during the incubation period (as reported in a patient with a possible incubation of >20 days [29]). Because the LD attack rate is very low, this situation is highly unlikely. In addition, epidemiologists classifying these cases might follow some definition (either national or not publicly available) for HCA LD, most likely on the basis of time between date of symptom onset and date of admission to hospital. Assuming equal rates of infection for both community-acquired and HCA LD, a study estimated that a cutoff of 6 days would identify HCA LD with a predictive value of >77% (30).
In conclusion, HCA LD cases are responsible for a large proportion of LD diagnoses in Europe and differ from community-acquired cases in many aspects, including demographic characteristics, causative pathogens, and outcome. Given the severity of the disease, officials must identify cases and control outbreaks as quickly as possible. An agreed-on case definition for HCA LD might streamline the surveillance process.
Dr. Beauté is a medical epidemiologist in the Surveillance and Response Support Unit at the European Centre for Disease Prevention and Control. His research interests include the surveillance of infectious diseases, especially in specific settings, such as travel and healthcare.
Acknowledgment
We thank our colleagues in the European Legionnaires’ disease Surveillance Network who provided the data. We thank Daniela Schmid, Günther Wewalka, Olivier Denis, Stéphanie Jacquinet, Denis Piérard, Sophie Quoilin, Iskra Tomova, Despo Pieridou, Ioanna Gregoriou, Maria Koliou, Vladimir Drašar, Irena Martinková, Charlotte Kjelsø, Søren Anker Uldum, Irina Dontsenko, Rita Peetso, Sari Jaakola, Jaana Kusnetsov, Outi Lyytikäinen, Silja Mentula, Christine Campese, Sophie Jarraud, Bonita Brodhun, Christian Lück, Anastasia Flountzi, Elisavet Mouratidou, Ágnes Fehér, Thorolfur Gudnason, Guðrún Sigmundsdóttir, Julie Arnott, Joan O’Donnell, Tara Mitchell, Maria Grazia Caporali, Maria Luisa Ricci, Maria Cristina Rota, Antra Bormane, Jelena Galajeva, Oksana Savicka, Migle Janulaitiene, Simona Zukauskaite-Sarapajeviene, Paul Reichert, Jackie Maistre Melillo, Tanya Melillo Fenech, Graziella Zahra, Petra Brandsema, Manon Haverkate, Dominique Caugant, Heidi Lange, Michal Czerwinski, Katarzyna Piekarska, Teresa Fernandes, Maria Teresa Marques, Marina Ramos, Daniela Badescu, Gratiana Chicin, Odette Popovici, Danka Šimonyiová, Margita Špaleková, Maja Sočan, Darja Kese, Rosa Cano-Portero, Carmen Pelaz Antolin, Margareta Löfdahl, Gavin Dabrera, Ross Cameron, Tim Harrison, Jim McMenamin, Falguni Naik, Nick Phin, Kevin Pollock, and Emmanuel Robesyn for providing data and reading the draft manuscript.
References
- Fields BS, Benson RF, Besser RE. Legionella and Legionnaires’ disease: 25 years of investigation. Clin Microbiol Rev. 2002;15:506–26. DOIPubMedGoogle Scholar
- Beauté J; The European Legionnaires’ Disease Surveillance Network. Legionnaires’ disease in Europe, 2011 to 2015. Euro Surveill. 2017;22. DOIPubMedGoogle Scholar
- Soda EA, Barskey AE, Shah PP, Schrag S, Whitney CG, Arduino MJ, et al. Vital signs: health care-associated Legionnaires’ disease surveillance data from 20 states and a large metropolitan area - United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66:584–9. DOIPubMedGoogle Scholar
- European Centre for Disease Prevention and Control. Annual epidemiological report for 2017—Legionnaires' disease. Stockholm: The Centre; 2019.
- European Centre for Disease Prevention and Control. Legionnaires’ disease in Europe, 2015. ECDC surveillance report. Stockholm: The Centre; 2017.
- Hamilton KA, Prussin AJ II, Ahmed W, Haas CN. Outbreaks of Legionnaires’ disease and Pontiac fever 2006-2017. Curr Environ Health Rep. 2018;5:263–71. DOIPubMedGoogle Scholar
- Sabria M, Yu VL. Hospital-acquired legionellosis: solutions for a preventable infection. Lancet Infect Dis. 2002;2:368–73. DOIPubMedGoogle Scholar
- Chalmers JD, Taylor JK, Singanayagam A, Fleming GB, Akram AR, Mandal P, et al. Epidemiology, antibiotic therapy, and clinical outcomes in health care-associated pneumonia: a UK cohort study. Clin Infect Dis. 2011;53:107–13. DOIPubMedGoogle Scholar
- Polverino E, Torres A, Menendez R, Cillóniz C, Valles JM, Capelastegui A, et al.; HCAP Study investigators. Microbial aetiology of healthcare associated pneumonia in Spain: a prospective, multicentre, case-control study. Thorax. 2013;68:1007–14. DOIPubMedGoogle Scholar
- Helbig JH, Bernander S, Castellani Pastoris M, Etienne J, Gaia V, Lauwers S, et al. Pan-European study on culture-proven Legionnaires’ disease: distribution of Legionella pneumophila serogroups and monoclonal subgroups. Eur J Clin Microbiol Infect Dis. 2002;21:710–6. DOIPubMedGoogle Scholar
- Blatt SP, Parkinson MD, Pace E, Hoffman P, Dolan D, Lauderdale P, et al. Nosocomial Legionnaires’ disease: aspiration as a primary mode of disease acquisition. Am J Med. 1993;95:16–22. DOIPubMedGoogle Scholar
- Decker BK, Palmore TN. The role of water in healthcare-associated infections. Curr Opin Infect Dis. 2013;26:345–51. DOIPubMedGoogle Scholar
- Stephens JH, Shaw DD, Koehler AP. Legionella pneumophila: probable transmission from a contaminated respiratory device. Commun Dis Intell Q Rep. 2015;39:E201–3.PubMedGoogle Scholar
- Collins SL, Afshar B, Walker JT, Aird H, Naik F, Parry-Ford F, et al. Heated birthing pools as a source of Legionnaires’ disease. Epidemiol Infect. 2016;144:796–802. DOIPubMedGoogle Scholar
- Almeida D, Cristovam E, Caldeira D, Ferreira JJ, Marques T. Are there effective interventions to prevent hospital-acquired Legionnaires’ disease or to reduce environmental reservoirs of Legionella in hospitals? A systematic review. Am J Infect Control. 2016;44:e183–8. DOIPubMedGoogle Scholar
- Santé Publique France. Legionellosis notification form [updated 2017 Feb 6] [cited 2020 Jul 16]. https://demarchesadministratives.fr/formulaires/cerfa-12202-02-maladie-a-declaration-obligatoire-legionellose
- Istituto Superiore di Sanità. Linee guida per la prevenzione ed il controllo della legionellosi. 2015 May 13 [cited 2020 Jul 16]. http://old.iss.it/binary/iss4/cont/C_17_pubblicazioni_2362.pdf
- Public Health England. Legionnaires’ disease: case definitions. [updated 2017 Feb 6] [cited 2020 Jul 16]. https://www.gov.uk/government/publications/legionnaires-disease-clinical-case-definitions
- European Commission. Commission Implementing Decision 2012/506/EU of 8 August 2012 amending Decision 2002/253/EC laying down case definitions for reporting communicable diseases to the community network under decision no 2119/98/EC of the European Parliament and of the Council [cited 2020 Jul 16]. https://op.europa.eu/en/publication-detail/-/publication/10ed460f-0711-11e2-8e28-01aa75ed71a1/language-en
- Beauté J, Zucs P, de Jong B, on behalf of the European Legionnai C; European Legionnaires’ Disease Surveillance Network. Legionnaires disease in Europe, 2009-2010. Euro Surveill. 2013;18:20417. DOIPubMedGoogle Scholar
- Farnham A, Alleyne L, Cimini D, Balter S. Legionnaires’ disease incidence and risk factors, New York, New York, USA, 2002-2011. Emerg Infect Dis. 2014;20:1795–802. DOIPubMedGoogle Scholar
- Straus WL, Plouffe JF, File TM Jr, Lipman HB, Hackman BH, Salstrom SJ, et al.; Ohio Legionnaires Disease Group. Risk factors for domestic acquisition of legionnaires disease. Ohio legionnaires Disease Group. Arch Intern Med. 1996;156:1685–92. DOIPubMedGoogle Scholar
- Goetz AM, Stout JE, Jacobs SL, Fisher MA, Ponzer RE, Drenning S, et al. Nosocomial legionnaires’ disease discovered in community hospitals following cultures of the water system: seek and ye shall find. Am J Infect Control. 1998;26:8–11. DOIPubMedGoogle Scholar
- Katz SM, Hammel JM. The effect of drying, heat, and pH on the survival of Legionella pneumophila. Ann Clin Lab Sci. 1987;17:150–6.PubMedGoogle Scholar
- Phin N, Parry-Ford F, Harrison T, Stagg HR, Zhang N, Kumar K, et al. Epidemiology and clinical management of Legionnaires’ disease. Lancet Infect Dis. 2014;14:1011–21. DOIPubMedGoogle Scholar
- Currie SL, Beattie TK. Compost and Legionella longbeachae: an emerging infection? Perspect Public Health. 2015;135:309–15. DOIPubMedGoogle Scholar
- Muder RR, Yu VL. Infection due to Legionella species other than L. pneumophila. Clin Infect Dis. 2002;35:990–8. DOIPubMedGoogle Scholar
- Seenivasan MH, Yu VL, Muder RR. Legionnaires’ disease in long-term care facilities: overview and proposed solutions. J Am Geriatr Soc. 2005;53:875–80. DOIPubMedGoogle Scholar
- Bargellini A, Marchesi I, Marchegiano P, Richeldi L, Cagarelli R, Ferranti G, et al. A culture-proven case of community-acquired legionella pneumonia apparently classified as nosocomial: diagnostic and public health implications. Case Rep Med. 2013;2013:
303712 . DOIPubMedGoogle Scholar - Lessler J, Brookmeyer R, Perl TM. An evaluation of classification rules based on date of symptom onset to identify health-care associated infections. Am J Epidemiol. 2007;166:1220–9. DOIPubMedGoogle Scholar
Figures
Tables
Follow Up
Earning CME Credit
To obtain credit, you should first read the journal article. After reading the article, you should be able to answer the following, related, multiple-choice questions. To complete the questions (with a minimum 75% passing score) and earn continuing medical education (CME) credit, please go to http://www.medscape.org/journal/eid. Credit cannot be obtained for tests completed on paper, although you may use the worksheet below to keep a record of your answers.
You must be a registered user on http://www.medscape.org. If you are not registered on http://www.medscape.org, please click on the “Register” link on the right hand side of the website.
Only one answer is correct for each question. Once you successfully answer all post-test questions, you will be able to view and/or print your certificate. For questions regarding this activity, contact the accredited provider, CME@medscape.net. For technical assistance, contact CME@medscape.net. American Medical Association’s Physician’s Recognition Award (AMA PRA) credits are accepted in the US as evidence of participation in CME activities. For further information on this award, please go to https://www.ama-assn.org. The AMA has determined that physicians not licensed in the US who participate in this CME activity are eligible for AMA PRA Category 1 Credits™. Through agreements that the AMA has made with agencies in some countries, AMA PRA credit may be acceptable as evidence of participation in CME activities. If you are not licensed in the US, please complete the questions online, print the AMA PRA CME credit certificate, and present it to your national medical association for review.
Article Title:
Healthcare-Associated Legionnaires’ Disease, Europe, 2008–2017
CME Questions
1. Which of the following settings is associated with the highest proportion of Legionnaires' disease (LD) cases in the European Union?
A. Animal-human transmission; farm-related
B. Healthcare-associated (HCA)
C. Travel-associated
D. Community-acquired
2. Which of the following statements regarding temporal trends in the prevalence of LD in the current study is most accurate?
A. Community-acquired cases increased over time whereas HCA cases declined
B. HCA cases increased over time whereas community-acquired cases declined
C. Community-acquired and HCA cases both increased over time
D. Community-acquired and HCA cases were both stable over time
3. Which of the following statements regarding the characteristics of LD infection in the current study is most accurate?
A. HCA LD was more common as a proportion of LD among individuals age < 20 years vs 50 to 59 years
B. HCA LD was more common as a proportion of LD among individuals age 50 to 59 years vs ≥ 60 years
C. In adjusted analyses, men were more likely to have HCA LD than women
D. HCA LD prevalence was highest in December and January
4. Which of the following statements regarding the laboratory tests for LD and clinical outcomes in the current study is most accurate?
A. Rates of culture-confirmed LD were lower in hospital-associated LD vs other healthcare settings
B. Most cases of HCA LD were linked to Legionella pneumophila serogroup 3
C. Nearly 30% of cases of HCA LD died
D. The highest risk for death was associated with L pneumophila serogroup 1
Original Publication Date: September 17, 2020
Related Links
Table of Contents – Volume 26, Number 10—October 2020
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Julien Beauté, European Centre for Disease Prevention and Control (ECDC), Gustav III:s boulevard 40, 169 73 Solna, Sweden
Top