Volume 27, Number 12—December 2021
CME ACTIVITY - Research
Trends in Incidence and Clinical Outcomes of Clostridioides difficile Infection, Hong Kong
Figure
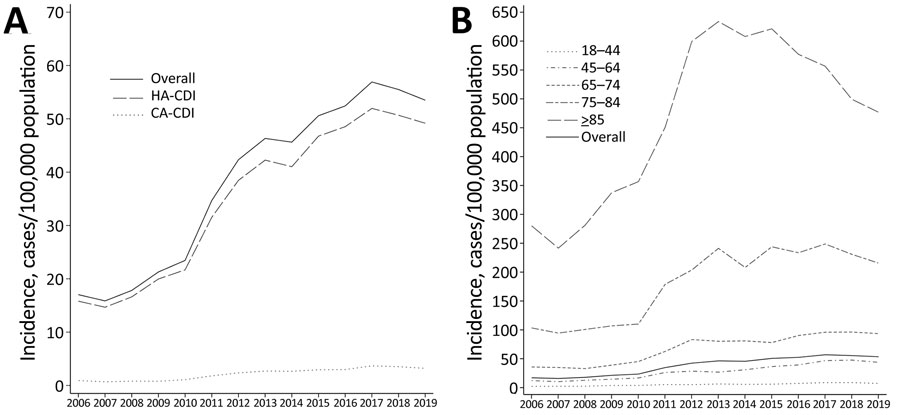
Figure. Clostridioides difficile infections in adults, Hong Kong, 2006–2019. Data for 2006–2014 were acquired from a previous study (13). A) Crude incidence of healthcare-associated and community-associated C. difficile infections. B) Incidence of infections by age group.
References
- Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015;372:1539–48. DOIPubMedGoogle Scholar
- Guh AY, Mu Y, Winston LG, Johnston H, Olson D, Farley MM, et al.; Emerging Infections Program Clostridioides difficile Infection Working Group. Emerging Infections Program Clostridioides difficile Infection Working Group. Trends in U.S. burden of Clostridioides difficile infection and outcomes. N Engl J Med. 2020;382:1320–30. DOIPubMedGoogle Scholar
- Heimann SM, Cruz Aguilar MR, Mellinghof S, Vehreschild MJGT. Economic burden and cost-effective management of Clostridium difficile infections. Med Mal Infect. 2018;48:23–9. DOIPubMedGoogle Scholar
- Rizzardi K, Norén T, Aspevall O, Mäkitalo B, Toepfer M, Johansson Å, et al. National surveillance for Clostridioides difficile infection, Sweden, 2009–2016. Emerg Infect Dis. 2018;24:1617–25. DOIPubMedGoogle Scholar
- Ofori E, Ramai D, Dhawan M, Mustafa F, Gasperino J, Reddy M. Community-acquired Clostridium difficile: epidemiology, ribotype, risk factors, hospital and intensive care unit outcomes, and current and emerging therapies. J Hosp Infect. 2018;99:436–42. DOIPubMedGoogle Scholar
- Valiente E, Cairns MD, Wren BW. The Clostridium difficile PCR ribotype 027 lineage: a pathogen on the move. Clin Microbiol Infect. 2014;20:396–404. DOIPubMedGoogle Scholar
- Collins DA, Sohn KM, Wu Y, Ouchi K, Ishii Y, Elliott B, et al.; Clostridioides difficile Asia-Pacific Study Group. Clostridioides difficile infection in the Asia-Pacific region. Emerg Microbes Infect. 2019;9:42–52. DOIPubMedGoogle Scholar
- Imwattana K, Knight DR, Kullin B, Collins DA, Putsathit P, Kiratisin P, et al. Clostridium difficile ribotype 017 - characterization, evolution and epidemiology of the dominant strain in Asia. Emerg Microbes Infect. 2019;8:796–807. DOIPubMedGoogle Scholar
- Collins DA, Riley TV. Clostridium difficile in Asia: opportunities for One Health management. Trop Med Infect Dis. 2018;4:
E7 . DOIPubMedGoogle Scholar - Kong KY, Kwong TNY, Chan H, Wong K, Wong SSY, Chaparala AP, et al. Biological characteristics associated with virulence in Clostridioides difficile ribotype 002 in Hong Kong. Emerg Microbes Infect. 2020;9:631–8. DOIPubMedGoogle Scholar
- Wong SH, Ip M, Hawkey PM, Lo N, Hardy K, Manzoor S, et al. High morbidity and mortality of Clostridium difficile infection and its associations with ribotype 002 in Hong Kong. J Infect. 2016;73:115–22. DOIPubMedGoogle Scholar
- Chow VCY, Kwong TNY, So EWM, Ho YII, Wong SH, Lai RWM, et al. Surveillance of antibiotic resistance among common Clostridium difficile ribotypes in Hong Kong. Sci Rep. 2017;7:17218. DOIPubMedGoogle Scholar
- Ho J, Dai RZW, Kwong TNY, Wang X, Zhang L, Ip M, et al. Disease burden of Clostridium difficile infections in adults, Hong Kong, China, 2006–2014. Emerg Infect Dis. 2017;23:1671–9. DOIPubMedGoogle Scholar
- Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57:1288–94. DOIPubMedGoogle Scholar
- Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, et al.; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31:431–55. DOIPubMedGoogle Scholar
- Thelwall S, Nsonwu O, Rooney G, Wasti S, Anselmo J, Hope R; Public Health England. Clostridium difficile infection: mandatory surveillance 2017/18. London: Public Health England; 2018.
- Wilcox MH. Clostridium difficile surveillance in England. Infectious Agents Surveillance Report. 2020;41:39–41.
- US Centers for Disease Control and Prevention. 2017 annual report for the Emerging Infections Program for Clostridioides difficile infection. 2017 [cited 2021 Oct 15]. https://www.cdc.gov/hai/eip/pdf/cdiff/2017-CDI-Report-H.pdf
- Liao F, Li W, Gu W, Zhang W, Liu X, Fu X, et al. A retrospective study of community-acquired Clostridium difficile infection in southwest China. Sci Rep. 2018;8:3992. DOIPubMedGoogle Scholar
- Tariq R, Cho J, Kapoor S, Orenstein R, Singh S, Pardi DS, et al. Low risk of primary Clostridium difficile infection with tetracyclines: a systematic review and metaanalysis. Clin Infect Dis. 2018;66:514–22. DOIPubMedGoogle Scholar
- Ho P, Wu T, Chao DV, Hung IF, Lui L, Lung DC, et al. Reducing bacterial resistance with IMPACT, 5th edition, Hong Kong. Hong Kong: Centre for Health Protection—Department of Health; 2017.
- Lui RN, Wong SH, Lau LHS, Chan TT, Cheung KCY, Li A, et al. Faecal microbiota transplantation for treatment of recurrent or refractory Clostridioides difficile infection in Hong Kong. Hong Kong Med J. 2019;25:178–82.PubMedGoogle Scholar
- Gupta A, Khanna S. Community-acquired Clostridium difficile infection: an increasing public health threat. Infect Drug Resist. 2014;7:63–72.PubMedGoogle Scholar
- Ng SC, Leung WK, Shi HY, Li MK, Leung CM, Ng CK, et al. Epidemiology of inflammatory bowel disease from 1981 to 2014: results from a territory-wide population-based registry in Hong Kong. Inflamm Bowel Dis. 2016;22:1954–60. DOIPubMedGoogle Scholar
1These authors contributed equally to this work.
2These authors were co–principal investigators.
Page created: November 17, 2021
Page updated: November 17, 2021
Page reviewed: November 17, 2021
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.