Volume 29, Number 12—December 2023
Research Letter
Microfilaremic Dirofilaria repens Infection in Patient from Serbia
Cite This Article
Citation for Media
Abstract
We report a case of Dirofilaria repens infection causing microfilaremia in a patient from Serbia. Serum samples tested positive for D. repens IgG by ELISA. Our findings and those of others suggest the parasite's progressive adaptation to humans. Clinicians should be aware that microfilaremia can develop during Dirofilaria spp. infections.
Dirofilaria repens is a vectorborne filarial helminth of carnivores, mainly domesticated dogs (1). Humans are considered accidental hosts, in which the parasite induces local inflammation causing granulomatous reactions primarily detected in subcutaneous and ocular tissues. Because humans are not natural hosts, microfilariae are typically absent from peripheral blood; thus, diagnostic procedures require morphologic and molecular analyses of removed worms (2). Immunodiagnostic tests are being designed as potential alternatives to invasive diagnostic procedures (3). This parasite rarely evades the human host’s immune system to reach sexual maturity. The literature reports 22 cases of human D. repens microfilaremia, of which several have been confirmed through molecular examination (3,4). We describe a case of human dirofilariasis with circulating microfilariae in a patient from Serbia.
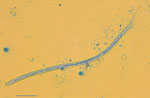
A 43-year-old professional soldier in the army of Serbia was first seen for a walnut-sized swelling accompanied by itching on the inner side of his thigh, which we promptly treated with ciprofloxacin (1 g/d) for 14 days. Two months after the initial swelling, the patient noted another similar protuberance on his inner thigh that migrated toward the back of the thigh every 2–3 days. An ultrasound detected a 13.5 × 8 mm subcutaneous nodule. Biochemical analyses of the patient’s blood and blood cell counts were within reference ranges, including eosinophil levels; however, surgical intervention was required 1 month after the ultrasound to excise the nodule and investigate its origin. Examination of the removed nodule revealed a Dirofilaria repens–like specimen. Twenty days after nodule removal, the percentage of eosinophils in the patient’s peripheral blood increased to 14%. We performed a modified Knotts test on EDTA blood, which revealed the presence of 2 microfilariae/mL. The mean microfilaria body length was 377–378 µm and mean width was 7.35–7.6 µm; they had no sheath but had obtuse cervical ends, 2–3 separate nuclei in the head space, and nuclei-free filiform tails (Figure).
We used species-specific PCR that amplified a portion of the cytochrome oxidase subunit 1 gene, cox1, to confirm the microfilariae were D. repens (Appendix). BLAST (https://blast.ncbi.nlm.nih.gov) analysis of the nucleotide sequence revealed a 97%–100% identity with published sequences of D. repens (Appendix Figure). We deposited the sequence in GenBank (accession no. OR426928.1). We constructed a maximum-likelihood phylogenetic tree of cox1 sequences from this study and representative D. repens isolates from animals and humans in Europe by using MEGA version 11 software (5) and the Kimura 2-parameter distance model. We assessed the robustness of nodes by using 500 bootstrap replicates; Ascaris lumbricoides (GenBank accession no. AB591801.1) was the outgroup (Appendix Figure).
We used ELISAs to detect Dirofilaria spp. IgG. Cutoff optical densities were 1.8 for the commercial Acanthocheilonema viteae IgG ELISA kit (Bordier, http://www.bordier.ch), which detects IgG against various filarial nematodes in human serum, and 2.3 for an in-house ELISA (Appendix).
Two months after the D. repens diagnosis, the patient had an eosinophil count within reference ranges. No further microfilariae were detected in peripheral blood smears during monitoring.
Dirofilaria spp. infections are increasing globally, posing a substantial threat to pets, particularly dogs (1). The rising number of human dirofilariasis cases underscores the need for large-scale epidemiologic studies to establish effective preventive measures (1,4). Although humans are generally regarded as unsuitable hosts for D. repens, detection of single subadult or adult worms in humans is not uncommon (3). The worms can infrequently develop into mature adults, mate, and produce microfilariae, which can potentially enter the bloodstream in human hosts. Diagnosis involves morphologic and molecular analyses, but surgical removal of the worm and specialized equipment are required (2). Serologic tests detect specific antibodies, providing a more reliable epidemiologic picture of the zoonosis within a study area (3).
Several protocols are available to investigate seroreactivity in humans (6,7), but antibody responses might not be detected until the nematode has migrated internally from subcutaneous tissue (8). Localization of larvae in ocular tissue might confer greater protection for the parasite, leading to a low predictive positive value for diagnosing Dirofilaria spp. infection (9).
No established treatment protocols exist for dirofilariasis or microfilaremia, leaving therapeutic decisions to physicians. Surgery is the primary treatment, accompanied by adjuvant therapy options, such as ivermectin, albendazole, or diethylcarbamazine. Doxycycline, a treatment for Wolbachia endosymbionts, has been used (9). In this case, we considered anthelmintics after surgical removal and microfilariae detection but chose continuous monitoring. Two months after diagnosis, the patient’s health was satisfactory, and he had no symptoms or complications from the infection.
In conclusion, we report a case of D. repens microfilaremia in a professional soldier frequently exposed to vector biting because of prolonged outdoor activities during military training in northern Serbia, a dirofilariasis-endemic area (10). The presence of circulating microfilariae highlighted by this and previous studies shows the parasite’s progressive adaptation to humans and suggests a potential role for humans as a definitive D. repens host. Although a role for humans as an infection reservoir remains to be clarified, clinicians should be aware that microfilaremia can develop during Dirofilaria spp. infections.
Dr. Tasić-Otasevic is a professor in the Department of Microbiology and Immunology, University of Niš, and Department of Microbiology and Parasitology, Public Health Institute. Her research interests are clinical and diagnostic microbiology, skin and genital infections, antimicrobial resistance, fungal pathogens, vectorborne zoonosis, and health promotion.
References
- Genchi C, Kramer LH. The prevalence of Dirofilaria immitis and D. repens in the Old World. Vet Parasitol. 2020;280:
108995 . DOIPubMedGoogle Scholar - Gabrielli S, Mangano V, Furzi F, Oliva A, Vita S, Poscia R, et al. Molecular identification of new cases of human dirofilariosis (Dirofilaria repens) in Italy. Pathogens. 2021;10:251. DOIPubMedGoogle Scholar
- Simón F, Diosdado A, Siles-Lucas M, Kartashev V, González-Miguel J. Human dirofilariosis in the 21st century: A scoping review of clinical cases reported in the literature. Transbound Emerg Dis. 2022;69:2424–39. DOIPubMedGoogle Scholar
- Pupić-Bakrač A, Pupić-Bakrač J, Beck A, Jurković D, Polkinghorne A, Beck R. Dirofilaria repens microfilaremia in humans: Case description and literature review. One Health. 2021;13:
100306 . DOIPubMedGoogle Scholar - Tamura K, Stecher G, Kumar S. MEGA11: molecular evolutionary genetics analysis version 11. Mol Biol Evol. 2021;38:3022–7. DOIPubMedGoogle Scholar
- Ciuca L, Simòn F, Rinaldi L, Kramer L, Genchi M, Cringoli G, et al. Seroepidemiological survey of human exposure to Dirofilaria spp. in Romania and Moldova. Acta Trop. 2018;187:169–74. DOIPubMedGoogle Scholar
- Savić S, Stosic MZ, Marcic D, Hernández I, Potkonjak A, Otasevic S, et al. Seroepidemiological study of canine and human dirofilariasis in the endemic region of northern Serbia. Front Vet Sci. 2020;7:571. DOIPubMedGoogle Scholar
- Otranto D, Eberhard ML. Zoonotic helminths affecting the human eye. Parasit Vectors. 2011;4:41. DOIPubMedGoogle Scholar
- Simón F, Siles-Lucas M, Morchón R, González-Miguel J, Mellado I, Carretón E, et al. Human and animal dirofilariasis: the emergence of a zoonotic mosaic. Clin Microbiol Rev. 2012;25:507–44. DOIPubMedGoogle Scholar
- Tasić-Otašević S, Savić S, Jurhar-Pavlova M, Stefanovska J, Stalević M, Ignjatović A, et al. Molecular survey of Dirofilaria and Leishmania species in dogs from central Balkan. Animals (Basel). 2022;12:911. DOIPubMedGoogle Scholar
Figure
Cite This ArticleOriginal Publication Date: October 31, 2023
Table of Contents – Volume 29, Number 12—December 2023
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Simona Gabrielli, Department of Public Health and Infectious Diseases, Sapienza University of Rome, Piazzale Aldo Moro 5, Rome 00185, Italy
Top