Volume 29, Number 2—February 2023
Synopsis
Streptococcus dysgalactiae Bloodstream Infections, Norway, 1999–2021
Figure 6
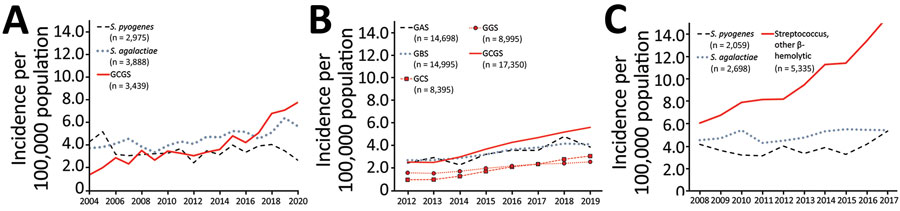
Figure 6. National surveillance data for β-hemolytic streptococcal bloodstream infections in 3 countries: A) Norway, 2004–2020; B) United Kingdom, 2012–2019; C) Finland, 2008–2017. We compiled data from annual surveillance reports published during the given time periods (6,25–27). The 3 countries use different surveillance methods. UK surveillance is based on voluntary reporting from the microbiology laboratories, whereas in Norway and Finland, surveillance data are collected electronically from the laboratories’ information systems. We calculated incidence rates by acquiring contemporary population data from Norway (https://www.ssb.no), the United Kingdom (https://www.ons.gov.uk), and Finland (https://www.stat.fi). We used taxonomic labels that appeared in the original publications, except GCGS, which we constructed for the purpose of this study by combining incidence data for GCS and GGS. GAS, group A Streptococcus; GBS, group B Streptococcus; GCS, group C Streptococcus; GGS, group G Streptococcus; GCGS, group C and G Streptococcus.
References
- Oppegaard O, Mylvaganam H, Kittang BR. Beta-haemolytic group A, C and G streptococcal infections in Western Norway: a 15-year retrospective survey. Clin Microbiol Infect. 2015;21:171–8. DOIPubMedGoogle Scholar
- Rantala S, Vuopio-Varkila J, Vuento R, Huhtala H, Syrjänen J. Clinical presentations and epidemiology of β-haemolytic streptococcal bacteraemia: a population-based study. Clin Microbiol Infect. 2009;15:286–8. DOIPubMedGoogle Scholar
- Wajima T, Morozumi M, Hanada S, Sunaoshi K, Chiba N, Iwata S, et al. Molecular Characterization of Invasive Streptococcus dysgalactiae subsp. equisimilis, Japan. Emerg Infect Dis. 2016;22:247–54. DOIPubMedGoogle Scholar
- US Centers for Disease Control and Prevention. Active bacterial core surveillance [cited 2022 Nov 16]. www.cdc.gov/abcs/reports-findings/surv-reports.html
- Australian Government, Department of Health and Aged Care. Australian national notifiable diseases case definition [cited 2022 Nov 16]. https://www.health.gov.au/resources/publications/invasive-group-a-streptococcal-disease-igas-surveillance-case-definition
- Finnish Institute for Health and Welfare. Infectious diseases in Finland 2017. Helsinki: The Institute; 2017.
- Vandamme P, Pot B, Falsen E, Kersters K, Devriese LA. Taxonomic study of lancefield streptococcal groups C, G, and L (Streptococcus dysgalactiae) and proposal of S. dysgalactiae subsp. equisimilis subsp. nov. Int J Syst Bacteriol. 1996;46:774–81. DOIPubMedGoogle Scholar
- Facklam R. What happened to the streptococci: overview of taxonomic and nomenclature changes. Clin Microbiol Rev. 2002;15:613–30. DOIPubMedGoogle Scholar
- Bradley SF, Gordon JJ, Baumgartner DD, Marasco WA, Kauffman CA. Group C streptococcal bacteremia: analysis of 88 cases. Rev Infect Dis. 1991;13:270–80. DOIPubMedGoogle Scholar
- Leitner E, Zollner-Schwetz I, Zarfel G, Masoud-Landgraf L, Gehrer M, Wagner-Eibel U, et al. Prevalence of emm types and antimicrobial susceptibility of Streptococcus dysgalactiae subsp. equisimilis in Austria. Int J Med Microbiol. 2015;305:918–24. DOIPubMedGoogle Scholar
- Lo HH, Cheng WS. Distribution of virulence factors and association with emm polymorphism or isolation site among beta-hemolytic group G Streptococcus dysgalactiae subspecies equisimilis. APMIS. 2015;123:45–52. DOIPubMedGoogle Scholar
- UK Health Security Agency. Laboratory surveillance of pyogenic and non-pyogenic streptococcal bacteraemia in England: 2020 update. Health Protection Report, vol. 15, no. 19. London: The Agency; 2021.
- Lother SA, Demczuk W, Martin I, Mulvey M, Dufault B, Lagacé-Wiens P, et al. Clonal clusters and virulence factors of group C and G Streptococcus causing severe infections, Manitoba, Canada, 2012–2014. Emerg Infect Dis. 2017;23:1079–88. DOIPubMedGoogle Scholar
- Ruppen C, Rasmussen M, Casanova C, Sendi P. A 10-year observational study of Streptococcus dysgalactiae bacteraemia in adults: frequent occurrence among female intravenous drug users. Swiss Med Wkly. 2017;147:
w14469 .PubMedGoogle Scholar - Rößler S, Berner R, Jacobs E, Toepfner N. Prevalence and molecular diversity of invasive Streptococcus dysgalactiae and Streptococcus pyogenes in a German tertiary care medical centre. Eur J Clin Microbiol Infect Dis. 2018;37:1325–32. DOIPubMedGoogle Scholar
- Kittang BR, Langeland N, Mylvaganam H. Distribution of emm types and subtypes among noninvasive group A, C and G streptococcal isolates in western Norway. APMIS. 2008;116:457–64. DOIPubMedGoogle Scholar
- Oppegaard O, Mylvaganam H, Skrede S, Lindemann PC, Kittang BR. Emergence of a Streptococcus dysgalactiae subspecies equisimilis stG62647-lineage associated with severe clinical manifestations. Sci Rep. 2017;7:7589. DOIPubMedGoogle Scholar
- Jordal S, Glambek M, Oppegaard O, Kittang BR. New tricks from an old cow: infective endocarditis caused by Streptococcus dysgalactiae subsp. dysgalactiae. J Clin Microbiol. 2015;53:731–4. DOIPubMedGoogle Scholar
- Gajdács M, Ábrók M, Lázár A, Burián K. Beta-haemolytic group A, C and G streptococcal infections in Southern Hungary: a 10-year population-based retrospective survey (2008–2017) and a review of the literature. Infect Drug Resist. 2020;13:4739–49. DOIPubMedGoogle Scholar
- Lambertsen LM, Ingels H, Schønheyder HC, Hoffmann S; Danish Streptococcal Surveillance Collaboration Group 2011. Nationwide laboratory-based surveillance of invasive beta-haemolytic streptococci in Denmark from 2005 to 2011. Clin Microbiol Infect. 2014;20:O216–23. DOIPubMedGoogle Scholar
- Harris P, Siew DA, Proud M, Buettner P, Norton R. Bacteraemia caused by beta-haemolytic streptococci in North Queensland: changing trends over a 14-year period. Clin Microbiol Infect. 2011;17:1216–22. DOIPubMedGoogle Scholar
- Couture-Cossette A, Carignan A, Mercier A, Desruisseaux C, Valiquette L, Pépin J. Secular trends in incidence of invasive beta-hemolytic streptococci and efficacy of adjunctive therapy in Quebec, Canada, 1996-2016. PLoS One. 2018;13:
e0206289 . DOIPubMedGoogle Scholar - Trell K, Nilson B, Rasmussen M. Species and emm-type distribution of group C and G streptococci from different sites of isolation. Diagn Microbiol Infect Dis. 2016;86:467–9. DOIPubMedGoogle Scholar
- Schwartz IS, Keynan Y, Gilmour MW, Dufault B, Lagacé-Wiens P. Changing trends in β-hemolytic streptococcal bacteremia in Manitoba, Canada: 2007-2012. Int J Infect Dis. 2014;28:211–3. DOIPubMedGoogle Scholar
- NORM and NORM-VET. Usage of antimicrobial agents and occurrence of antimicrobial resistance in Norway, 2004–2020 [cited 2022 Nov 16]. https://unn.no/fag-og-forskning/norm-norsk-overvakingssystem-for-antibiotikaresistens-hos-mikrober#rapporter
- Public Health England. Laboratory surveillance of pyogenic and non-pyogenic streptococcal bacteraemia in England: 2019 update. Health protection report; vol. 14, no. 24. London: The Agency; 2020.
- Public Health England. Voluntary surveillance of pyogenic and non-pyogenic streptococcal bacteraemia 2016: appendix data for England only. Health protection report; vol. 11, no. 41. London: The Agency; 2017.
- Jensen CS, Dam-Nielsen C, Arpi M. Matrix-assisted laser desorption/ionization-time of flight mass spectrometry identification of large colony beta-hemolytic streptococci containing Lancefield groups A, C, and G. Infect Dis (Lond). 2015;47:575–9. DOIPubMedGoogle Scholar
- Nybakken EJ, Oppegaard O, Gilhuus M, Jensen CS, Mylvaganam H. Identification of Streptococcus dysgalactiae using matrix-assisted laser desorption/ionization-time of flight mass spectrometry; refining the database for improved identification. Diagn Microbiol Infect Dis. 2021;99:
115207 . DOIPubMedGoogle Scholar - Oppegaard O, Skrede S, Mylvaganam H, Kittang BR. Temporal trends of β-haemolytic streptococcal osteoarticular infections in western Norway. BMC Infect Dis. 2016;16:535. DOIPubMedGoogle Scholar
- Michael-Gayego A, Dan-Goor M, Jaffe J, Hidalgo-Grass C, Moses AE. Characterization of sil in invasive group A and G streptococci: antibodies against bacterial pheromone peptide SilCR result in severe infection. Infect Immun. 2013;81:4121–7. DOIPubMedGoogle Scholar
- Bruun T, Rath E, Madsen MB, Oppegaard O, Nekludov M, Arnell P, et al.; INFECT Study Group. Risk factors and predictors of mortality in streptococcal necrotizing soft-tissue infections: a multicenter prospective study. Clin Infect Dis. 2021;72:293–300. DOIPubMedGoogle Scholar
- Bläckberg A, Nilson B, Özenci V, Olaison L, Rasmussen M. Infective endocarditis due to Streptococcus dysgalactiae: clinical presentation and microbiological features. Eur J Clin Microbiol Infect Dis. 2018;37:2261–72. DOIPubMedGoogle Scholar
- Steens A, Knol MJ, Freudenburg-de Graaf W, de Melker HE, van der Ende A, van Sorge NM. Pathogen- and type-specific changes in invasive bacterial disease epidemiology during the first year of the COVID-19 pandemic in the Netherlands. Microorganisms. 2022;10:972. DOIPubMedGoogle Scholar