Volume 30, Number 11—November 2024
Research
Estimating Influenza Illnesses Averted by Year-Round and Seasonal Campaign Vaccination for Young Children, Kenya
Cite This Article
Citation for Media
Abstract
In Kenya, influenza virus circulates year-round, raising questions about optimum strategies for vaccination. Given national interest in introducing influenza vaccination for young children 6–23 months of age, we modeled total influenza-associated illnesses (inclusive of hospitalizations, outpatient illnesses, and non‒medically attended illnesses) averted by multiple potential vaccination strategies: year-round versus seasonal-campaign vaccination, and vaccination starting in April (Southern Hemisphere influenza vaccine availability) versus October (Northern Hemisphere availability). We modeled average vaccine effectiveness of 50% and annual vaccination coverage of 60%. In the introduction year, year-round vaccination averted 6,410 total illnesses when introduced in October and 7,202 illnesses when introduced in April, whereas seasonal-campaign vaccination averted 10,236 (October) to 11,612 (April) illnesses. In the year after introduction, both strategies averted comparable numbers of illnesses (10,831–10,868 for year-round, 10,175–11,282 for campaign). Campaign-style vaccination would likely have a greater effect during initial pediatric influenza vaccine introduction in Kenya; however, either strategy could achieve similar longer-term effects.
Influenza causes a substantial number of respiratory illnesses among young children in Kenya (1). The best time to vaccinate against seasonal influenza is before influenza viruses circulate, but because there are multiple periods of increased influenza activity each year in Kenya, the optimum timing and approach for influenza vaccination remains unclear (2‒4). In 2016, the Kenya National Immunization Technical Advisory Group issued a provisionary recommendation to introduce seasonal influenza vaccination among children 6–23 months of age on the basis of national evidence demonstrating substantial disease in this age group and advised that a pilot vaccination project should be conducted to inform a potential national vaccination rollout (5). As a result, a subnational pediatric vaccination pilot was conducted in Kenya during 2019–2021 to compare 2 potential delivery strategies: year-round vaccination, in which influenza vaccine is offered all months of the year, and a once-yearly seasonal vaccination campaign, in which influenza vaccine is offered only for 4 consecutive months (6,7). Results of the pilot indicated that both strategies might achieve similar vaccine coverage and incur a similar cost per dose for delivery but that the seasonal campaign could require considerable operational needs (e.g., workforce and cold chain capacity) compared with the year-round strategy (6,7).
In addition to those pilot data on the real-world performance of the proposed strategies, estimating the number of illnesses averted through influenza vaccination can provide additional, relevant evidence to inform pediatric influenza vaccination policy deliberations in Kenya. In other settings, averted illness estimates have provided actionable public health data for influenza vaccine implementation, such as optimizing campaign timing (8). In fact, a similar averted illness analysis was previously conducted for pregnant women and young children in Kenya and found that, given the year-round circulation of influenza, both year-round and twice-yearly vaccination strategies might avert a comparable number of illnesses compared with a single annual campaign (9). In this analysis, we adapted an existing model (8,10) to estimate the number of influenza illnesses and hospitalizations averted by influenza vaccine introduction for children 6–23 months of age in Kenya, comparing year-round to seasonal campaign vaccine delivery.
Base Model and Modifications
We adapted a static compartmental model jointly developed by the World Health Organization (WHO), US Centers for Disease Control and Prevention (CDC), and Pan American Health Organization (PAHO) to estimate the number of total influenza-associated illnesses (including hospitalized illnesses, outpatient illnesses, and non‒medically attended illnesses) averted by vaccination. Model methods have been published previously (8); in brief, we first estimated the burden of disease among children 6–23 months of age in Kenya in the absence of an influenza vaccination program and then calculated the number of illnesses averted through a counterfactual vaccination program.
We made 3 major modifications to the model described in Chard et al. (8) (Appendix Table 1, Figure 1). First, we expanded the time horizon from 12 months to 24 months (as years 1 and 2) to better simulate the effect of residual vaccine protection from the prior year, which was of particular interest for longer-term implementation of year-round vaccine delivery. Second, whereas the original model assumed constant vaccine effectiveness (VE) over the model timeframe, we assumed VE waned in the months after vaccination, as described previously in evaluating influenza vaccination among children and older adults (11,12). Finally, because we expanded the time period for the new model, we assumed that natural immunity from infection lasted for 12 months, meaning infected persons could recover within the model’s 24-month timeframe and return to the susceptible compartment for their remaining time. In addition, persons infected in the 12 months before the model’s start (year 0) were also systematically returned to the susceptible population as their 12-month immunity expired.
Vaccination Strategies Modeled
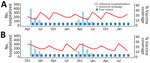
We modeled 2 distinct vaccination strategies: seasonal campaigns, as traditionally used in countries with a Southern or Northern Hemisphere influenza season (13), and year-round vaccination, as has been proposed for countries with no clear influenza season (14). Although the 2019–2021 demonstration project included campaigns starting in June and July (6), we modeled 2 variations of the seasonal campaign with starting months of April (corresponding to the usual timing of Southern Hemisphere influenza vaccine availability) and October (corresponding to Northern Hemisphere vaccine availability) (13) (Figure). We assumed each vaccination campaign would last 4 months, as in the demonstration project (6). For year-round vaccination, we similarly modeled initial introduction of the vaccine in both April and October for comparability across the 24-month analysis timeframe. As a sensitivity analysis, we included 2 additional start times for the seasonal campaign: June (halfway between Southern and Northern Hemisphere vaccine availability) and January (halfway between Northern and Southern Hemisphere vaccine availability).
Model Data Inputs
We estimated the 2022 population size for children 6–23 months of age in Kenya (n = 1,809,394) based on growth projections from 2019 census data (15,16) (Table 1). We used a previously published incidence of influenza-associated severe acute respiratory illness hospitalizations among children 0–23 months of age in Kenya during 2011–2014 (146.6/100,000 population; 17) to calculate the annual expected number of hospitalizations (n = 2,653). In addition, we derived an average seasonal curve of influenza-associated disease burden from influenza surveillance data reported to the WHO Global Influenza Surveillance and Response System FluNet data platform (21) from Kenya for all ages during 2011–2019. Using an aggregate average method (22), we calculated a 3-week moving proportion of samples positive for influenza (Appendix Figure 2). We then distributed the 2,653 annual hospitalizations across weeks of the year using this seasonal curve and summed weekly counts to generate monthly hospitalizations; all years of the model (0‒3) used the same hospitalization curve (Figure).
To estimate the number of influenza-associated events by different strata of severity of illness and care-seeking (i.e., hospitalized illnesses, outpatient illnesses, and total illnesses inclusive of non‒medically attended), the model uses multipliers for the ratio of nonhospitalized to hospitalized illnesses and for the proportion of illnesses medically attended. We calculated a multiplier for the ratio of nonhospitalized to hospitalized cases based on a combination of sentinel surveillance data from Siaya County among children 6–23 months of age during 2011–2013 and a 2018 healthcare utilization survey of children <2 years of age in Kenya (18) (Appendix Figure 3). We obtained a multiplier for the proportion of illnesses that were medically attended using the same healthcare utilization survey (18).
On the basis of results of the demonstration project comparing year-round and campaign vaccine delivery in 2 counties during 2019–2021 (6), we assumed that both delivery strategies would achieve equal cumulative vaccine coverage; we set this value to 60% annually for both strategies. We allocated monthly coverage for the year-round strategy evenly across the year and coverage for the seasonal campaign according to the distribution of monthly coverage achieved during the demonstration project (Figure). We assumed that children would receive 2 doses of influenza vaccine >4 weeks apart, in accordance with recommendations for the age group (23), to be considered fully vaccinated; thus, no children were considered fully vaccinated at month 1 of vaccine introduction. However, for the first year after introduction (postintroduction year) of the seasonal campaign, we assumed that one third of children who were previously vaccinated would remain in the eligible age group (6–11 months of age in the first year and 18–23 months in the second year), receiving only 1 dose of vaccine and considered fully vaccinated in the first month of the postintroduction year campaign.
For influenza VE inputs, we used an average VE of 50% against any influenza-associated illness, consistent with 2010–2012 clinical trial data for trivalent influenza vaccine in children <5 years of age in Kenya (19), as well as a meta-analysis of influenza VE among children 6–23 months of age (20). The base scenario incorporated cubic waning of VE as previously described (11), with a starting VE of 70% in month 1 and an average VE of 50% over 8 months (Appendix Table 2). We explored 2 additional patterns: scenario A modeled a constant of 50% with vaccine protection lasting 8 months and then 0% VE (no protection) thereafter, and scenario B modeled a constant VE of 50% with protection lasting 12 months (Appendix Table 2).
Model Outputs
We estimated the number of hospitalizations, outpatient visits, medically attended illnesses (inclusive of both outpatient visits and hospitalizations), and total illnesses (inclusive of medically attended and non–medically attended illnesses) averted by each vaccination strategy and stratified results by year. We also calculated the prevented fraction, defined as the number of illnesses averted by vaccination divided by the number of illnesses in the absence of vaccine. We used Monte Carlo simulation with 5,000 iterations to sample parameter values at random from their distributions and obtained confidence intervals for all estimates. Monte Carlo simulation assumed a Poisson distribution for monthly hospitalizations, a uniform distribution for the ratio of nonhospitalized to hospitalized influenza illnesses, and normal distributions for the proportion of influenza illnesses non‒medically attended, VE, and vaccine coverage. We performed all analyses in R version 4.0.2 (The R Project for Statistical Computing, https://www.r-project.org).
From the modeled estimates, during the first year that seasonal influenza vaccination was introduced (introduction year), year-round vaccination starting in April averted an estimated 7,202 (95% CI 5,898–8,616) total influenza-associated illnesses in children 6–23 months of age, including 3,450 (95% CI 2,751–4,251) medically attended illnesses and 349 (95% CI 286–416) hospitalizations (Table 2). Year-round vaccination starting in October averted an estimated 6,410 (95% CI 5,218–7,692) total illnesses, including 3,066 (95% CI 2,431–3,769) medically attended illnesses and 311 (95% CI 254–371) hospitalizations (Table 2). The prevented fraction of total illnesses in the introduction year was 13% (95% CI 11%–16%) when year-round vaccination was introduced in April and 12% (95% CI 10%–14%) when introduced in October. In comparison, an April–July (Southern Hemisphere) seasonal campaign averted an estimated 11,612 (95% CI 9,220–14,478) total illnesses, including 5,546 (95% CI 4,287–7,090) medically attended illnesses and 562 (95% CI 448–695) hospitalizations; an October–January seasonal campaign (corresponding to Northern Hemisphere vaccine availability) averted an estimated 10,236 (95% CI 8,082–12,837) total influenza-associated illnesses, including 4,894 (95% CI 3,787–6,286) medically attended illnesses and 497 (95% CI 394–621) hospitalizations. The prevented fraction of total illnesses was 21% (95% CI 17%–26%) for the April–July campaign and 19% (95% CI 15%–23%) for October–January.
In the second year after influenza vaccination was introduced (postintroduction year), year-round vaccination averted an estimated 10,831 (95% CI 8,748–13,106) total illnesses, including 5,188 (95% CI 4,077–6,464) medically attended illnesses and 526 (95% CI 426–635) hospitalizations when introduced in April and 10,868 (95% CI 8,726–13,162) total illnesses, including 5,187 (95% CI 4,079–6,486) medically attended illnesses and 528 (95% CI 425–636) hospitalizations when introduced in October (Table 3). The prevented fraction of total illnesses was 20% (95% CI 16%–24%) for year-round vaccination regardless of the starting month. An April–July seasonal campaign averted an estimated 11,282 (95% CI 8,752–14,099) total illnesses, including 5,392 (95% CI 4,130–6,890) medically attended illnesses and 547 (95% CI 425–684) hospitalizations, and an October–January seasonal campaign averted an estimated 10,175 (95% CI 7,891–12,876) total illnesses, including 4,869 (95% CI 3,703–6,253) medically attended illnesses and 493 (95% CI 384–622) hospitalizations. The prevented fraction was 21% (95% CI 16–26) for the April–July campaign and 19% (95% CI 14–23) for October–January.
Sensitivity analyses indicated that assuming a constant 8-month VE without waning (scenario A) did not significantly change the estimate of averted illness for any strategy in the introduction or postintroduction years compared with the base scenario (Appendix Table 3, Figure 4). Assuming a constant 12-month VE (scenario B) increased the absolute number of averted illnesses for all strategies in the postintroduction year, but 95% CIs overlapped with the base scenario for the April seasonal campaign and year-round strategy with October introduction (Appendix Table 4, Figure 4). In addition, sensitivity analyses that changed the starting month of the seasonal campaign to January or June did not significantly affect the estimates of averted illnesses (Appendix Figure 5).
Introducing influenza vaccination for children 6–23 months of age in Kenya would reduce the number of influenza-associated illnesses substantially. Our results indicate that campaign-style vaccination would likely have the greatest effect for initial introduction because it would most rapidly achieve high population protection in a vaccine-naive population. Our finding is consistent with recommendations for catch-up campaigns, or initial campaign-style rollout of vaccination to accelerate herd protection, for other vaccines; for example, modeling findings indicated that catch-up campaigns would increase the efficiency of pneumococcal conjugate vaccine introduction for children <5 years of age in Kenya (24). However, our results suggest that, after the initial introduction, either year-round vaccination or a seasonal campaign could have similar effects for long-term implementation. Therefore, national policy decisions regarding which strategy to implement for influenza vaccination should consider the full portfolio of evidence available from the demonstration project, including coverage, costs, effects on the wider health system, logistical feasibility, and perceptions from both the community and health workers (6,7,25). For example, implementation experiences from the vaccination pilot suggested greater operational demands within a short time for the campaign strategy (6), but year-round delivery could also be operationally complex (9,14); previously proposed options include using both Northern and Southern Hemisphere formulations during their respective influenza seasons or extending use of a single formulation for the entire year (14). More data are needed on clinical protection offered by those options and programmatic feasibility of changing formulations during a year to inform how year-round vaccination would be implemented. Prior analyses have also considered a twice-yearly vaccination campaign strategy which might offer an intermediate option to year-round and single annual vaccination (5,9); however, we did not include that strategy in this analysis for comparability with the 2019–2021 demonstration project (6).
The first limitation of our study is that the results from our analysis are greatly dependent on the 2011–2019 influenza seasonal curve that we calculated using FluNet data for Kenya. Because the seasonal curve we calculated from surveillance data showed no clear single seasonal peak, our results indicated that timing a vaccination program with either Southern or Northern Hemisphere vaccine availability might have similar results in Kenya. Previous analyses characterizing influenza seasonality in Kenya are not consistent; a recent analysis suggested that Kenya had 3 influenza seasons, occurring primarily during the Southern Hemisphere seasonal months (19), whereas others have suggested a primarily Northern Hemisphere epidemic (26), 2 major epidemics (3), or unascertainable seasonality (4). Even within the years included in the seasonal curve calculation, not all matched the average seasonality exactly; some years have larger peaks at different times, and, thus, use of a seasonal curve does not account for potential year-to-year variations in incidence or temporal distribution of influenza illnesses, which could influence the model results. In addition, to calculate the annual number of influenza hospitalizations, we used an estimate of incidence among children 0–23 months of age during 2011–2014, which might not be representative of all years; because incidence among children 0–5 months of age might be slightly lower than incidence for those 6–11 and 12–23 months (17), inclusion of this age group might have underestimated true incidence among the target population 6–23 months of age. Similarly, the results are dependent on the VE estimate used, which can also vary year-to-year based on the level of vaccine match with circulating viruses (23). We assumed the same VE for both the Northern and Southern Hemisphere vaccine formulations, as well as for both severe illness (i.e., hospitalization) and mild illness, which might in reality have differential VEs (27).
Second, we based our models on assumptions about duration of vaccine-induced immunity, which we modeled from earlier analysis of VE among older adults rather than young children. However, analyses have indicated similar patterns of waning of VE among children and older adults (12), and sensitivity analyses using a constant VE suggested that the base scenario might, in fact, be a conservative estimate of the vaccine’s impact. Similarly, we assumed that previous infection would confer 12 months of natural immunity, consistent with earlier models that did not include reinfections within a 12-month timeframe (8,10). Cohort studies have indicated that reinfections with influenza virus are possible within a single season (28,29); thus, our model assumptions might not fully reflect the duration of natural immunity and likelihood of reinfection in Kenya, particularly given year-round influenza circulation. Third, given the relatively short timeframe examined (24 months), we assumed a stable population and did not account for potential changes in population size (e.g., births, deaths, and migrations) within the model period. Fourth, results in the postintroduction year include residual immunity from the previous year. If a catch-up campaign were used for initial vaccine introduction and the program transitioned to year-round vaccination, the effect of the vaccine would not be equivalent to the postintroduction year results until >2 years of year-round vaccination had occurred. Fifth, we assumed that both strategies would achieve the same annual vaccine coverage based on results of the vaccination pilot (6), but it is possible that a year-round strategy could reach more children during noncampaign months and result in higher coverage, as previously modeled for maternal influenza vaccination (9), or that differences in vaccination program costs could result in differential coverage achieved (7).
Finally, we assumed that vaccinated persons were either fully protected by their vaccine or unprotected. Alternative assumptions—for example, where all vaccinees experience a reduced rate of acquiring infection—might result in a higher estimated number of illnesses prevented by vaccination (30). In addition, the model did not include nonrespiratory manifestations of influenza illness (31), did not account for partial immunity received from a single dose of influenza vaccine among young children (23,32), and did not include indirect effects of the vaccine (33) or estimates of averted deaths (34). Furthermore, because less than one third (32%) of young children with severe pneumonia were hospitalized in a previous healthcare utilization survey in Kenya (20), a substantial burden of severe illness is missed by focusing on hospitalizations alone. Therefore, our results likely underestimate the full value and effect of influenza vaccination, which warrant further evaluation.
Our findings indicate that either year-round or seasonal campaign vaccination for influenza could substantially reduce influenza burden among children 6–23 months of age in Kenya, resulting in health and economic benefits to children and their families, as well as to the health system and broader society. The results of our analysis suggest that campaign-style vaccination would achieve the greatest impact for in the first year of introduction; however, longer-term implementation could employ either strategy to achieve similar effect. Our data can be used to inform additional analyses, such as estimating averted cost burden, cost-benefit, or cost-effectiveness of vaccination. Policy decisions regarding the most appropriate vaccination strategy should holistically weigh the available evidence and local implementation context.
Dr. Gharpure is an epidemiologist at the Coalition for Epidemic Preparedness Innovations; during the completion of this work, she was an epidemiologist in the Influenza Division at the US Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases. Her primary research interests are at the intersection of infectious disease epidemiology, vaccine implementation, and policy.
Acknowledgment
We thank Eduardo Azziz-Baumgartner, Anna Chard, and Vanessa Cozza for early input into the analysis design and conceptualization.
References
- Emukule GO, Paget J, van der Velden K, Mott JA. Influenza-associated disease burden in Kenya: a systematic review of literature. PLoS One. 2015;10:
e0138708 . DOIPubMedGoogle Scholar - Emukule GO, Mott JA, Spreeuwenberg P, Viboud C, Commanday A, Muthoka P, et al. Influenza activity in Kenya, 2007-2013: timing, association with climatic factors, and implications for vaccination campaigns. Influenza Other Respir Viruses. 2016;10:375–85. DOIPubMedGoogle Scholar
- Hirve S, Newman LP, Paget J, Azziz-Baumgartner E, Fitzner J, Bhat N, et al. Influenza seasonality in the tropics and subtropics—when to vaccinate? PLoS One. 2016;11:
e0153003 . DOIPubMedGoogle Scholar - Dawa J, Emukule GO, Barasa E, Widdowson MA, Anzala O, van Leeuwen E, et al. Seasonal influenza vaccination in Kenya: an economic evaluation using dynamic transmission modelling. BMC Med. 2020;18:223. DOIPubMedGoogle Scholar
- Dawa J, Chaves SS, Ba Nguz A, Kalani R, Anyango E, Mutie D, et al.; Kenya National Immunization Technical Advisory Group (KENITAG). Developing a seasonal influenza vaccine recommendation in Kenya: Process and challenges faced by the National Immunization Technical Advisory Group (NITAG). Vaccine. 2019;37:464–72. DOIPubMedGoogle Scholar
- Dawa J, Jalang’o R, Mirieri H, Kalani R, Marwanga D, Lafond KE, et al. Comparing performance of year-round and campaign-mode influenza vaccination strategies among children aged 6-23 months in Kenya: 2019-2021. Vaccine. 2024;42(Suppl 4):
125461 . DOIPubMedGoogle Scholar - Gharpure R, Akumu AO, Dawa J, Gobin S, Adhikari BB, Lafond KE, et al. Costs of seasonal influenza vaccine delivery in a pediatric demonstration project for children aged 6-23 months - Nakuru and Mombasa Counties, Kenya, 2019-2021. Vaccine. 2024;42(Suppl 4):
125519 . DOIPubMedGoogle Scholar - Chard AN, Machingaidze C, Loayza S, Gharpure R, Nogareda F, González R, et al. Estimating averted illnesses from influenza vaccination for children and pregnant women - El Salvador, Panama, and Peru, 2011-2018. Vaccine. 2024;42(Suppl 4):
125861 . DOIPubMedGoogle Scholar - McMorrow ML, Emukule GO, Obor D, Nyawanda B, Otieno NA, Makokha C, et al. Maternal influenza vaccine strategies in Kenya: Which approach would have the greatest impact on disease burden in pregnant women and young infants? PLoS One. 2017;12:
e0189623 . DOIPubMedGoogle Scholar - Tokars JI, Rolfes MA, Foppa IM, Reed C. An evaluation and update of methods for estimating the number of influenza cases averted by vaccination in the United States. Vaccine. 2018;36:7331–7. DOIPubMedGoogle Scholar
- Ferdinands JM, Alyanak E, Reed C, Fry AM. Waning of influenza vaccine protection: exploring the trade-offs of changes in vaccination timing among older adults. Clin Infect Dis. 2020;70:1550–9. DOIPubMedGoogle Scholar
- Belongia EA, Sundaram ME, McClure DL, Meece JK, Ferdinands J, VanWormer JJ. Waning vaccine protection against influenza A (H3N2) illness in children and older adults during a single season. Vaccine. 2015;33:246–51. DOIPubMedGoogle Scholar
- Cox N. Influenza seasonality: timing and formulation of vaccines. Bull World Health Organ. 2014;92:311. DOIPubMedGoogle Scholar
- Lambach P, Alvarez AM, Hirve S, Ortiz JR, Hombach J, Verweij M, et al. Considerations of strategies to provide influenza vaccine year round. Vaccine. 2015;33:6493–8. DOIPubMedGoogle Scholar
- Kenya National Bureau of Statistics. 2019 Kenya Population and Housing Census results. 2019 [cited 2023 Nov 8]. https://www.knbs.or.ke/2019-kenya-population-and-housing-census-results
- Dawa JA, Chaves SS, Nyawanda B, Njuguna HN, Makokha C, Otieno NA, et al. National burden of hospitalized and non-hospitalized influenza-associated severe acute respiratory illness in Kenya, 2012-2014. Influenza Other Respir Viruses. 2018;12:30–7. DOIPubMedGoogle Scholar
- Emukule GO, Osoro E, Nyawanda BO, Ngere I, Macharia D, Bigogo G, et al. Healthcare-seeking behavior for respiratory illnesses in Kenya: implications for burden of disease estimation. BMC Public Health. 2023;23:353. DOIPubMedGoogle Scholar
- Katz MA, Lebo E, Emukule GO, Otieno N, Caselton DL, Bigogo G, et al. Uptake and effectiveness of a trivalent inactivated influenza vaccine in children in urban and rural Kenya, 2010 to 2012. Pediatr Infect Dis J. 2016;35:322–9. DOIPubMedGoogle Scholar
- Boddington NL, Pearson I, Whitaker H, Mangtani P, Pebody RG. Effectiveness of influenza vaccination in preventing hospitalization due to influenza in children: a systematic review and meta-analysis. Clin Infect Dis. 2021;73:1722–32. DOIPubMedGoogle Scholar
- Igboh LS, Roguski K, Marcenac P, Emukule GO, Charles MD, Tempia S, et al. Timing of seasonal influenza epidemics for 25 countries in Africa during 2010-19: a retrospective analysis. Lancet Glob Health. 2023;11:e729–39. DOIPubMedGoogle Scholar
- World Health Organization. Vaccines against influenza: WHO position paper—May 2022. Wkly Epidemiol Rec. 2022;97:185–208.
- Flasche S, Ojal J, Le Polain de Waroux O, Otiende M, O’Brien KL, Kiti M, et al. Assessing the efficiency of catch-up campaigns for the introduction of pneumococcal conjugate vaccine: a modelling study based on data from PCV10 introduction in Kilifi, Kenya. BMC Med. 2017;15:113. DOIPubMedGoogle Scholar
- Liku N, Mburu C, Lafond KE, Ebama M, Athman M, Swaleh S, et al. A qualitative assessment of influenza vaccine uptake among children in Kenya. Vaccine X. 2024;19:
100507 . DOIPubMedGoogle Scholar - Alonso WJ, Yu C, Viboud C, Richard SA, Schuck-Paim C, Simonsen L, et al. A global map of hemispheric influenza vaccine recommendations based on local patterns of viral circulation. Sci Rep. 2015;5:17214. DOIPubMedGoogle Scholar
- Regan AK, Arriola CS, Couto P, Duca L, Loayza S, Nogareda F, et al. Severity of influenza illness by seasonal influenza vaccination status among hospitalised patients in four South American countries, 2013-19: a surveillance-based cohort study. Lancet Infect Dis. 2023;23:222–32. DOIPubMedGoogle Scholar
- Cohen C, Kleynhans J, Moyes J, McMorrow ML, Treurnicht FK, Hellferscee O, et al.; PHIRST group. Asymptomatic transmission and high community burden of seasonal influenza in an urban and a rural community in South Africa, 2017-18 (PHIRST): a population cohort study. Lancet Glob Health. 2021;9:e863–74. DOIPubMedGoogle Scholar
- Horby P, Mai Q, Fox A, Thai PQ, Thi Thu Yen N, Thanh T, et al. The epidemiology of interpandemic and pandemic influenza in Vietnam, 2007-2010: the Ha Nam household cohort study I. Am J Epidemiol. 2012;175:1062–74. DOIPubMedGoogle Scholar
- Tokars JI, Patel MM, Foppa IM, Reed C, Fry AM, Ferdinands JM. Waning of measured influenza vaccine effectiveness over time: the potential contribution of leaky vaccine effect. Clin Infect Dis. 2020;71:e633–41. DOIPubMedGoogle Scholar
- Macias AE, McElhaney JE, Chaves SS, Nealon J, Nunes MC, Samson SI, et al. The disease burden of influenza beyond respiratory illness. Vaccine. 2021;39(Suppl 1):A6–14. DOIPubMedGoogle Scholar
- Chung JR, Flannery B, Gaglani M, Smith ME, Reis EC, Hickey RW, et al. Patterns of influenza vaccination and vaccine effectiveness among young US children who receive outpatient care for acute respiratory tract illness. JAMA Pediatr. 2020;174:705–13. DOIPubMedGoogle Scholar
- Eichner M, Schwehm M, Eichner L, Gerlier L. Direct and indirect effects of influenza vaccination. BMC Infect Dis. 2017;17:308. DOIPubMedGoogle Scholar
- Newall AT, Nazareno AL, Muscatello DJ, Boettiger D, Viboud C, Simonsen L, et al. The association between influenza vaccination uptake and influenza and pneumonia-associated deaths in the United States. Vaccine. 2024;42:2044–50. DOIPubMedGoogle Scholar
Figure
Tables
Cite This ArticleOriginal Publication Date: October 19, 2024
Table of Contents – Volume 30, Number 11—November 2024
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
G.O. Emukule, US Centers for Disease Control and Prevention, Village Market, PO Box 606-00621, Nairobi, Kenya
Top