Volume 30, Number 3—March 2024
Research Letter
Staphylococcus succinus Infective Endocarditis, France
Abstract
Infective endocarditis is a rare condition in humans and is associated with high illness and death rates. We describe a case of infective endocarditis caused by Staphylococcus succinus bacteria in France. We used several techniques for susceptibility testing for this case to determine the oxacillin profile.
Staphylococcus succinus was first described in 1998 and was isolated from 25- to 35-million-year-old Dominican amber (1). Members of this species are widespread in nature. Studies have reported the frequent isolation of S. succinus bacteria from various sources, such as cheeses, dry or fermented meat products, the Dead Sea, and occasionally human specimens (2–4). We report a case of S. succinus infective endocarditis in a patient in France who had many cardiovascular risk factors: age, sex, hypertension, dyslipidemia, diabetes, and weight. In accordance with legislations in France and Europe, the use of anonymous data does not need approval of an ethics committee.
On hospital day 1, an 83-year-old man sought care for dyspnea and chest pain for 72 hours; he had evidence of global cardiac decompensation for a severe ischemic heart disease with preserved left ventricular ejection fraction. Cardiac blood marker analysis revealed an increased troponin level to 250 ng/L and thereafter 350 ng/L (reference range <14 ng/L). Electrocardiogram results showed ST-segment depression in the lateral leads. In this context of non–ST-segment elevation myocardial infarction, the patient was hospitalized in the cardiology unit. On day 6, transthoracic echocardiography revealed an aortic valve bioprosthesis, reshaped, with a thickening of the cusps and a vibratory element attached on the ventricular side (7 × 4 mm), suggesting vegetation suspicious for infective endocarditis (Appendix Figure). The patient became febrile. We collected a total of 7 sets of aerobic and anaerobic blood bottle cultures during days 9–12; all showed a Gram-positive coccus in clusters. Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry identification (VitekMS; bioMérieux, https://www.biomerieux.com) indicated S. succinus with a 99.9% index.
The patient initially received 6 g intravenous cefazolin; on day 13 we changed the antimicrobial treatment to intravenous daptomycin (10 mg/kg) and gentamicin (3 mg/kg) every 48 h. Finally, after a dedicated endocarditis multidisciplinary consultation, we changed the patient’s regimen on day 22 to daptomycin (10 mg/kg) and rifampin (900 mg) for 6 weeks. The patient returned home; follow-up care was scheduled with a hospital at home. The patient outcome was favorable without relapse or side effects from daptomycin/rifampin. His last cardiology appointment was 11 months after his initial treatment; no sequelae of endocarditis were present.
S. succinus susceptibility testing was a challenge. We performed methicillin resistance testing with cefoxitin screen and oxacillin testing using the AST-P668 bioMérieux card with a VitekXL automated system. However, we observed a discrepancy between the results from the 2 tests. To confirm oxacillin resistance, we tested by agar diffusion method using impregnated disks and interpreted them in accordance with EUCAST (European Committee on Antimicrobial Susceptibility Testing) criteria (https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_13.0_Breakpoint_Tables.pdf). We used oxacillin (1 μg) and cefoxitin (30 μg) disks (Bio-Rad, https://www.bio-rad.com). The oxacillin (1 μg) disk diffusion method detected oxacillin resistance. In contrast, the isolate was susceptible when we used the cefoxitin (30 μg) disk test. In addition, we performed an oxacillin MIC strip test; MIC of 0.5 (mg/L), indicated that the strain was susceptible according to the EUCAST 2022 criteria.
A retrospective study (5) of penicillin-binding protein (PBP) assays indicating antimicrobial drug resistance has shown that preinduction with cefoxitin/oxacillin and reading of the test after 10 min (instead of 5 min) substantially improve the sensitivity, specificity, and robustness of the immunochromatographic assay PBP2a (Abbott, https://www.globalpointofcare.abbott) for coagulase-negative staphylococci. We performed PBP2a detection from bacterial culture after a preinduction with cefoxitin, but results were negative. Thereafter, we performed mecA gene detection by PCR to identify oxacillin-resistant Staphylococcus (6); however, we did not detect the mecA gene by PCR.
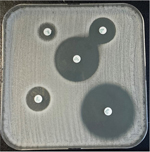
Finally, we sent the isolate to the French Reference Center for Staphylococci (Lyon, France) on day 19 for detection of other mec genes; this test result was negative. Staff at the reference center performed whole-genome sequencing of the strain as previously described (7); results revealed no site-specific insertion sequences comprising direct-repeat sequences typical of a staphylococcal cassette chromosome–like cassette (8). To evaluate the possibility of resistance by PBP modification, we performed a disk diffusion method for antimicrobial susceptibility of imipenem (PBP1), cefotaxime (PBP2), oxacillin (PBP3), and cefoxitin (PBP4) (9,10). The cefotaxime diameter was reduced, indicating resistance in a strain, most likely by a modification of PBP2 (Figure; Appendix Table).
In conclusion, we identified environmental S. succinus behaving as an opportunistic pathogen as the cause of infective endocarditis in a patient with many cardiovascular risk factors. The source of S. succinus was not clearly established. Virulence factors contributing to S. succinus pathogenicity are not yet well defined. We further described the difficulty of determining the resistance profile of this rarely pathogenic species mimicking either the borderline oxacillin-resistant S. aureus phenotype with an elevated oxacillin MIC value, or to a lesser extent the modified S. aureus phenotype in the absence of mec gene–mediated resistance. Our findings highlight the importance of a multiple-technology approach for laboratories assessing methicillin resistance using a combination of phenotypic and genotypic methods.
Dr. Ruffier d’Epenoux is a medical microbiologist at Nantes University Hospital, Nantes, France. Her primary research interests are device-related infections, especially bone and joint infection (Cutibacterium acnes) and prosthetic infective endocarditis.
Acknowledgments
We thank Patricia Martin for her technical assistance in the whole-genome sequencing of the clinical strain. We thank Julie Marraillac, Caroline Consent, Jihane El Khobzi, and Gaëlle Croizier, for their technical assistance.
This study has been recorded in the Nantes Hospital by the local Data Protection Officer under reference TS005-BIO-AP-2019_20. In accordance with legislations in France and Europe, the use of anonymous data does not need approval of an ethics committee.
References
- Lambert LH, Cox T, Mitchell K, Rosselló-Mora RA, Del Cueto C, Dodge DE, et al. Staphylococcus succinus sp. nov., isolated from Dominican amber. Int J Syst Bacteriol. 1998;48:511–8. DOIPubMedGoogle Scholar
- Place RBE, Hiestand D, Burri S, Teuber M. Staphylococcus succinus subsp. casei subsp. nov., a dominant isolate from a surface ripened cheese. Syst Appl Microbiol. 2002;25:353–9. DOIPubMedGoogle Scholar
- Stabnikov V, Chu J, Ivanov V, Li Y. Halotolerant, alkaliphilic urease-producing bacteria from different climate zones and their application for biocementation of sand. World J Microbiol Biotechnol. 2013;29:1453–60. DOIPubMedGoogle Scholar
- Nováková D, Sedláček I, Pantůček R, Štětina V, Švec P, Petráš P. Staphylococcus equorum and Staphylococcus succinus isolated from human clinical specimens. J Med Microbiol. 2006;55:523–8. DOIPubMedGoogle Scholar
- Kolesnik-Goldmann N, Bodendoerfer E, Röthlin K, Herren S, Imkamp F, Marchesi M, et al. Rapid detection of PBP2a in Staphylococci from shortly incubated subcultures of positive blood cultures by an immunochromatographic assay. Microbiol Spectr. 2021;9:
e0046221 . DOIPubMedGoogle Scholar - Okuma K, Iwakawa K, Turnidge JD, Grubb WB, Bell JM, O’Brien FG, et al. Dissemination of new methicillin-resistant Staphylococcus aureus clones in the community. J Clin Microbiol. 2002;40:4289–94. DOIPubMedGoogle Scholar
- Durand G, Javerliat F, Bes M, Veyrieras JB, Guigon G, Mugnier N, et al. Routine whole-genome sequencing for outbreak investigations of Staphylococcus aureus in a national reference center. Front Microbiol. 2018;9:511. DOIPubMedGoogle Scholar
- Ito T, Ma XX, Takeuchi F, Okuma K, Yuzawa H, Hiramatsu K. Novel type V staphylococcal cassette chromosome mec driven by a novel cassette chromosome recombinase, ccrC. Antimicrob Agents Chemother. 2004;48:2637–51. DOIPubMedGoogle Scholar
- Herold BC, Immergluck LC, Maranan MC, Lauderdale DS, Gaskin RE, Boyle-Vavra S, et al. Community-acquired methicillin-resistant Staphylococcus aureus in children with no identified predisposing risk. JAMA. 1998;279:593–8. DOIPubMedGoogle Scholar
- Tomic V, Svetina Sorli P, Trinkaus D, Sorli J, Widmer AF, Trampuz A. Comprehensive strategy to prevent nosocomial spread of methicillin-resistant Staphylococcus aureus in a highly endemic setting. Arch Intern Med. 2004;164:2038–43. DOIPubMedGoogle Scholar
Figure
Cite This ArticleOriginal Publication Date: February 01, 2024
Table of Contents – Volume 30, Number 3—March 2024
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Stéphane Corvec, Institut de Biologie des Hôpitaux de Nantes, Service de Bactériologie et des contrôles Microbiologiques, CHU de Nantes, 9 quai Moncousu, 44093 Nantes CEDEX 01, France
Top