Volume 30, Number 4—April 2024
Research Letter
Potential Sexual Transmission of Antifungal-Resistant Trichophyton indotineae
Figure
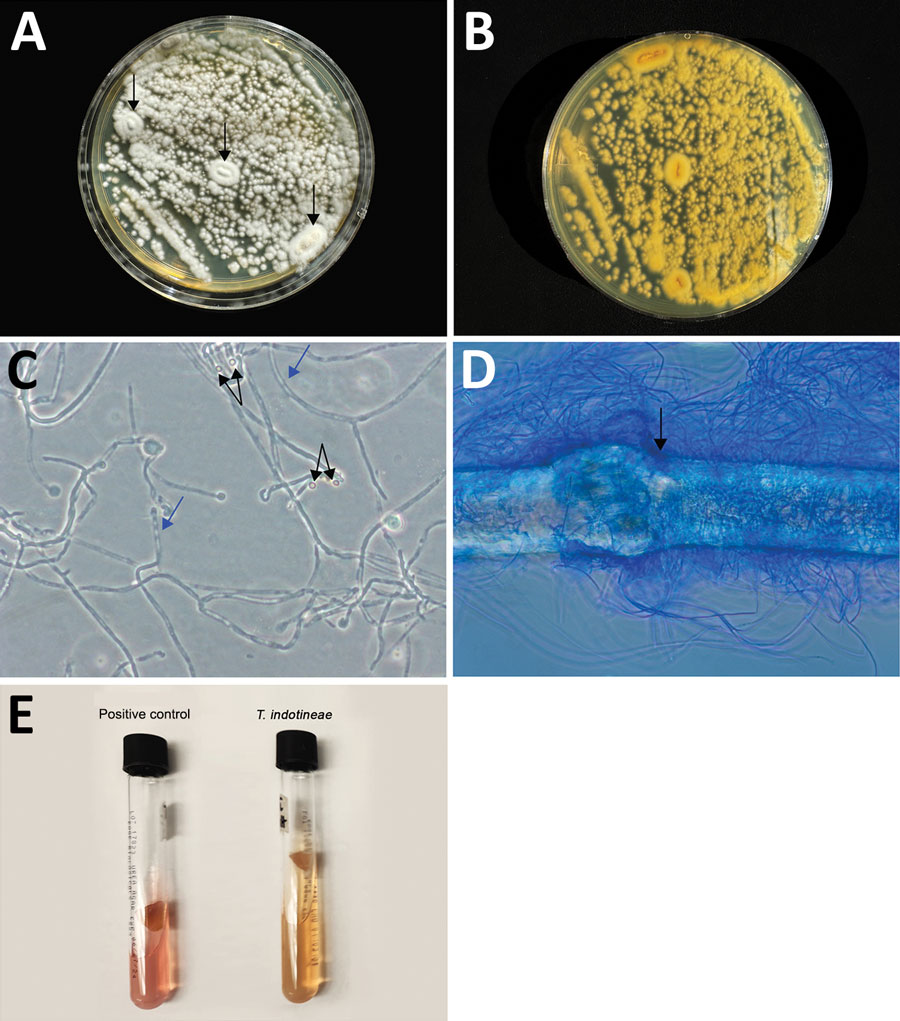
Figure. Results of gross and microscopic morphology and microbiological laboratory testing to identify Trichophyton indotineae in a woman in Pennsylvania, USA. A, B) Colonies were velvety white, flat, and had a raised center (arrow) (A) and a light yellow pigment on reverse (B). C) Numerous microconidia showed the pyriform and clavate forms (black arrow) and fungal hyphae with septation (blue arrows). Original magnification ×40. D) In vitro hair perforation test was positive (arrow). Original magnification ×100. E) T. indotineae had a negative urease test (yellowish color), while the positive control, Trichophyton tonsurans, was pinkish.
Page created: March 01, 2024
Page updated: March 21, 2024
Page reviewed: March 21, 2024
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.