Volume 30, Number 9—September 2024
Research
Medical Costs of Nontuberculous Mycobacterial Pulmonary Disease, South Korea, 2015–2019
Cite This Article
Citation for Media
Abstract
Nontuberculous mycobacterial pulmonary disease (NTM-PD) prevalence is a rising public health concern. We assessed the long-term healthcare systems perspective of costs incurred by 147 NTM-PD patients at a tertiary hospital in South Korea. Median cumulative total medical cost in managing NTM-PD patients was US $5,044 (interquartile range US $3,586–$9,680) over 49.7 months (interquartile range 33.0–68.2 months) of follow-up. The major cost drivers were diagnostic testing and medication, accounting for 59.6% of total costs. Higher costs were associated with hospitalization for Mycobacterium abscessus infection and pulmonary comorbidities. Of the total medical care costs, 50.2% were patient co-payments resulting from limited national health insurance coverage. As South Korea faces significant problems of poverty during old age and increasing NTM-PD prevalence, the financial and socio-economic burden of NTM-PD may become a major public health concern that should be considered with regard to adequate strategies for NTM-PD patients.
Nontuberculous mycobacteria pulmonary disease (NTM-PD) is a chronic respiratory condition of growing concern. Its management is often complicated by multiple biological, clinical, healthcare-associated, and patient factors. Increased NTM infection can be attributed to the widespread presence of NTM in the environment, multiple transmission routes, and insufficient preventive measures (1). Diagnosing NTM-PD alone does not require immediate treatment (2), often resulting in a period of medical observation before treatment initiation. Eradication of NTM is further challenged by lengthy treatment, lack of effective treatment regimens, antimicrobial resistance, adverse reactions to treatment, and low adherence to therapeutic guidelines (2–5). Unfavorable treatment outcomes and frequent recurrence necessitate continued observation even after treatment completion (6,7). By increasing the NTM-PD disease burden (1,3,8,9), such issues pose considerable financial strain for healthcare systems and patients.
Among earlier studies evaluating the NTM-PD burden, only a few reviewed the costs associated with NTM-PD (10,11). A 2017 study in Germany reported a nearly 4-fold increase in the mean direct medical expenditure for patients with NTM-PD compared with those who had never had NTM-PD (12). A 2020 study in Canada estimated that NTM-PD management required an annual mean cost of US $11,541 (13). Regardless of between-country differences in costs associated with NTM-PD, evidence suggests that NTM-PD poses a substantial cost burden from the healthcare provider perspective (14).
To better elucidate the cost burdens associated with NTM-PD, we analyzed the medical costs incurred by patients with NTM-PD in South Korea. Furthermore, we aimed to determine the distribution of costs over the follow-up period and the effects of causative NTM species or pulmonary comorbidities on the costs. Our study was approved by the Institutional Review Board of Severance Hospital (4-2021-1663), with an informed consent waiver considering its retrospective design.
We retrospectively reviewed electronic health records (EHRs) and institution billing records (IBRs) of patients who had NTM-PD during 2015–2019 in Severance Hospital, a tertiary referral hospital in South Korea. We restricted the review of medical cost data to patients who had initiated and completed >12 months of NTM-PD treatment before February 2022 (Figure 1). We did not analyze costs incurred by healthcare services provided by or prescribed from institutions other than Severance Hospital.
We extracted patient-level data from the EHR on clinical history, laboratory and imaging tests, prescribed treatment regimens, treatment outcomes, and fee-for-service costs for all relevant medical procedures and care services used by the included patients leading up to February 28, 2022. For costs that could not be ascertained from the IBRs (e.g., medications or health services prescribed from Severance Hospital but received from elsewhere), we referenced the Korean Health Insurance Review and Assessment Service catalog for unit cost/prices (as of January 2019) to calculate estimated total medical costs (15). We based the definition of direct medical out-of-pocket costs on patient co-payment amount assessed for each health service used, estimated by the cost ceilings for each item defined by the National Health Insurance Service (NHIS, https://www.nhis.or.kr) (Appendix Table 1).
To categorize hospital visits related to NTM-PD management, we divided the follow-up period into 4 periods: prediagnostic, pretreatment, treatment, and post-treatment (Figure 2). We defined the treatment period as the first uninterrupted NTM-PD treatment documented in the EHR.
All costs were assessed from the healthcare system perspective, which includes costs associated with patient co-payments (Table 1). Cumulative per-patient cost was defined as the total costs incurred at all NTM-PD–related visits over the entire follow-up period. Cost assessments were further categorically based on each period of follow-up, type of visit, and medical services. Subgroup analyses were based on NTM species, presence of pulmonary comorbidities, and type of services received (hospital admission, surgical treatment, and management of treatment complications).
All costs were assessed as 2019 United States dollars (US $), based on the mean exchange rate for South Korean won and US $ (1,165.69 won/US $1) and adjusted for the medical consumer price index and a 3% discount rate for costs incurred before 2019 (16,17). For all statistical analyses, we used SPSS Statistics 23 (IBM, https://www.ibm.com) and a 2-tailed significance level of 0.05.
Patient Selection and Baseline Characteristics
Of the 1,036 patients with NTM-PD and IBRs for 2015–2019, we included 147 in the final analysis (Figure 1). Median participant age was 61.0 years (interquartile range [IQR] 54.0–66.0 years), 100 (68.0%) participants were female and 47 (32%) were male, and 5 (3.4%) participants had previously received treatment for NTM-PD (Table 2).
From the index date, the median follow-up duration of our cohort was 49.7 months (IQR 33.0–68.2 months) and median treatment duration was 14.8 months (IQR 13.3–18.4 months). Over the entire follow-up period, 71 (48.3%) patients were admitted for NTM-PD >1 time.
Overall Per-Patient Medical Costs
The median per-patient cumulative total cost for NTM-PD treatment was US $5,044 (IQR $3,586–$9,680), or US $1,319 annually (Table 3; Appendix Table 2). Patients incurred a median out-of-pocket cost of US $2,535, which accounted for 50.2% of the total cost. For outpatient visits, patients with NTM-PD incurred a median total cost of US $3,863 (IQR $2,969–$5,333), or US $965 annually per patient. The 71 patients admitted for NTM-PD were hospitalized for a median of 9 days (IQR 3–30 days), incurring a median total admission cost of US $5,620 (IQR $1,296–$9,186), or US $1,146 annually (Appendix Table 3).
Patients with any history of hospitalization for NTM-PD–related treatment (median US $9,429) incurred a median total cost 2.5 times greater than those without (median US $3,773) (Appendix Table 4). However, costs for outpatient visits did not differ between both groups, suggesting that hospitalization costs were the main driver of increased medical cost for this patient group.
The median cumulative cost during the overall follow-up period was US $5,470 (IQR $3,613–$9,914) (Table 4; Figure 3; Appendix Table 5). The median per-patient cost was highest during the treatment period (US $2,108), followed by the pretreatment (US $616) and post-treatment (US $451) periods. Costs per patient were lowest for the prediagnostic period (US $425). Medical costs sharply increased approximately 6 months before treatment initiation, peaking during the first 3 months. Costs gradually decreased approximately 1 year after treatment initiation (Appendix Figure 1).
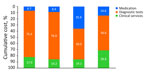
By types of medical services, costs for diagnostic tests shared the highest cumulative (59.6%, US $3,006), outpatient (59.1%, US $2,282), and admission (54.3%, US $1,590) costs over the entire follow-up period (Table 3). Diagnostic tests consistently accounted for the highest costs in any follow-up period (Table 4, Figure 3). Medication costs accounted for the second largest proportion of the cumulative costs for the entire follow-up period (23.7%, US $1,197) and for those incurred only during treatment (38.6%, US $814) but not in all other periods.
Subgroup Analyses and Patient-Level Cost Drivers
When comparing costs by the 2 major NTM species, the overall duration of follow-up was longer for the 112 patients treated for M. avium complex (MAC) infection (median 51.4 months) than for the 15 treated for M. abscessus infection (median 33.1 months); p = 0.006). All 15 patients with M. abscessus infection had been admitted for NTM-PD treatment, experiencing >2 hospitalizations that resulted in total stays of 33 days (IQR 28–62 days). Nearly 40.2% of patients with MAC infection were admitted for a median duration of 5 days (IQR 2–10 days) (Appendix Table 6). Likewise, median medical costs incurred by patients with M. abscessus infection (US $19,190) were higher than those incurred by patients with MAC infection (US $4,557; p<0.001) (Table 5; Appendix Tables 7, 8); the main driver of the cost difference between the groups was admission costs.
Regarding patient-level factors, the number of outpatient and admission visits, total length of stay, and death associated with M. abscessus infection (compared with MAC infection) were associated with increased total medical care costs for NTM-PD (Appendix Table 9). Multiple linear regression results revealed that the number of admissions and M. abscessus infections (compared with MAC infections) were positively associated with the total medical cost (i.e., more admissions and M. abscessus infections increased costs), whereas culture conversion was associated with decreased total cost (Table 6).
Out-of-Pocket Costs
Patients incurred a median out-of-pocket cost of US $2,535 (Table 3), accounting for 50.2% of the cumulative cost. The co-payment for outpatient visits and admissions was 55% (median US $2,124) and 26.6% (median US $1,494) of the cumulative costs for the respective visits. Similar to the patterns observed for cumulative costs, out-of-pocket costs over the follow-up period indicated that the highest co-payment was observed for the treatment period (US $1,029), followed by the pretreatment (US $359) and post-treatment (US $287) periods (Table 4; Figure 3).
Our report of comprehensive and detailed NTM-PD medical care costs in South Korea indicates that each patient with NTM-PD incurred a total cost of US $5,044 over a median follow-up period of 49.7 months, which translates to a median annual cost of US $1,319. Restricting analysis to the 87 patients with complete follow-up data brings the total median cost slightly higher, to US $5,470. Our analyses revealed that most NTM-PD–associated medical services were not fully covered through the Korean NHIS, resulting in a median out-of-pocket cost accounting for 50.2% (US $2,535) of the total care costs. Most (66.4%) of the total NTM-PD medical costs were incurred between 6 months before and 1 year after treatment initiation. The largest share of the total medical costs during the entire follow-up period was costs associated with diagnostic tests. Medical costs were higher for patients with M. abscessus infection and those with pulmonary comorbidities because of more frequent hospital visits and more extended hospitalizations.
In earlier studies evaluating medical costs of pulmonary infections in South Korea, medical costs for NTM-PD were considerably higher than those for asthma (US $267, reported in 2017) and drug-susceptible tuberculosis (US $754, reported in 2022) and were comparable to the costs for treating and managing tuberculosis-destroyed lungs (US $1,838, reported in 2019) (18–20). Furthermore, a recent 2023 study conducted by our team using the NHIS database reported that patients with NTM infection incurred at least 1.5 times higher annual medical costs than the healthy control population (a total annual medical cost of US $2,279.99 vs. US $1,496.26) (21). In addition, patients with NTM-PD incurred large co-payments or direct out-of-pocket costs for medical services not covered through the NHIS. Those costs comprised >50% of the total medical costs, suggesting that long-term disease burden directly translates to a considerable cost burden for patients with NTM-PD compared with other chronic respiratory conditions (22,23).
We report the long-term costs associated with NTM-PD and the cost drivers by different phases of disease management, types of medical services, and parts of the medical costs borne by patients. Costs start to increase approximately 6 months before treatment initiation, peak during the first quarter of treatment, and then decrease after approximately 1 year of treatment (Appendix Figure 1). That period, which roughly coincides with the pretreatment and treatment periods (Table 2), accounts for 66.4% of the total cost (Appendix Figure 2). A combination of factors may explain the cost concentration observed throughout that period, when intensive laboratory studies are needed to decide when to initiate treatment and monitor treatment outcomes as well as treatment and management of associated adverse events. Previous studies have demonstrated that the economic burden is greater during the early follow-up phases. In a recent study that compared healthcare expenditures among patients with NTM infection and matched controls, medical costs were the highest 6 months before NTM-PD diagnosis (21). Similar studies conducted in Germany and the United States reported that annual overall healthcare costs were highest during the first year after NTM-PD diagnosis (12,24). Another study conducted in Canada demonstrated that costs attributable to NTM-PD during the acute-care phase (i.e., the first 150 days after the first hospital visit associated with NTM-PD) were greater than those associated with subsequent care phases (13).
Earlier studies have identified hospitalization costs as the main cost driver of NTM-PD management (12,13,24). Among our study population, 71 (48.3%) patients were admitted for NTM-PD–related issues throughout the follow-up period. Admission costs accounted for ≈59.6% of the total costs incurred by those patients, consistent with earlier findings reporting hospitalization costs accounting for as much as 69% of the total medical costs for NTM-PD (14). In our study, the main cost drivers for hospital admissions (54.3%) and the entire NTM-PD management (59.6%) were diagnostic tests (Table 3). The second largest cost driver, medication costs (23.7% of the total cost), was concentrated in the treatment period (38.4% of the costs during treatment) (Table 3; Appendix Figure 2). Our estimates were higher than those in France (6%), Germany (9%–21.8%), and the United Kingdom (12%) but lower than those in Canada (6%–70%), which may reflect differences in clinical practice and patient characteristics across countries (11,12,14). Furthermore, a relatively lower proportion of medication costs for managing NTM-PD in South Korea may be attributed to the government-negotiated drug costs for those approved for reimbursement schemes by the NHIS, which are generally lower than the market prices in other high-income settings (25).
Clinically challenging patient subgroups, such as those with M. abscessus infections (2,26) or comorbidities, probably require more healthcare resources and incur more costs for disease management (10,11). Our study directly assessed the increased costs and cost drivers associated with managing more difficult subgroups of patients with NTM-PD in South Korea. Patients with the M. abscessus subtype incurred costs 4.2 times higher than those infected with MAC, which was almost exclusively because of the increased costs associated with longer and more frequent hospitalizations for patients with M. abscessus infection (Table 5; Appendix Table 6). Moreover, patients with pulmonary comorbidities bore >67.4% more costs to treat and manage NTM-PD than those without comorbidities (Appendix Tables 10–12). NTM-PD patients with pulmonary comorbidities incurred approximately twice as much medication cost and a 50% increase in diagnostic test costs. When comparing the cost driver by types of clinical visits, we found that most of the increased medical costs were attributable to hospitalization costs.
Our cost estimates of NTM-PD management in South Korea were considerably lower than those in Germany and Canada. In 2011, Leber et al. estimated an annual cost of approximately CA $6,000 required to treat NTM-PD in Canada (11). In 2017, researchers in Germany compared the healthcare costs of patients with NTM-PD with those of uninfected controls and reported an attributable direct annual cost associated with NTM-PD of €9,093.20 (12). Our estimate of US $1,319 as the annual cost of managing NTM-PD is substantially lower in absolute terms; the large difference in medical costs for NTM-PD may be attributable to lower fee-for-service costs for medical care in South Korea than in Germany or Canada. According to a 2021 health report of the Organisation for Economic Cooperation and Development (OECD, https://www.oecd.org), per-capita healthcare expenditure in Korea (US $3,406) is approximately half of that in Canada (US $5,370) and Germany (US $6,518); however, healthcare use (e.g., annual consultations per person) far exceeds (17.2 in 2019 for South Korea) that of Germany (9.8) and Canada (6.6) (23). Those discrepancies may result from considerable differences in medical fee schedules across those countries. If medical service fees in South Korea are equivalent to those of Canada and Germany, costs associated with NTM-PD management in South Korea would be equivalent to, if not higher than, those of Canada and Germany.
Although our study did not assess patient perspective costs, we were able to assess patient co-payment costs associated with all medical services used through NTM-PD management. Patients incurring higher medical costs experienced higher co-payment and out-of-pocket costs for their illness management. Except for patients with M. abscessus infection, patients in our cohort paid approximately more than half of the cumulative total medical care costs incurred during their disease management at our institution alone, which represents a much larger share (in terms of co-payment) of medical costs relative to the general South Korea population average (30%) and >3 times the share of costs reported from Canada (15%) and Germany (13%) (23).
Given the limited scope of our data, we were not able to ascertain cost burdens associated with nonmedical direct and indirect costs. As such, the direct patient out-of-pocket medical care costs assessed represent only ≈2% of the South Korea Gross Domestic Product per capita. However, South Korea faces substantial problems with poverty during old age, which affects 43.8% of the elderly population according to the OECD. That proportion is the highest in the OECD rankings and 3 times greater than the OECD average of 13.5% (27). NTM-PD patients in our study and South Korea in general are elderly (8,21,28). Given those considerations, we suspect that NTM-PD may impose major socio-economic burdens on the patients, which may be much more significant for particular subgroups (e.g., those with multiple hospitalizations or M. abscessus infections and those who remain culture positive despite treatment). More research is needed to better understand the socio-economic consequences of NTM-PD (including the level of catastrophic costs experienced by the patient and their household because of NTM-PD) and guide the development of relevant policy measures.
Among the interpretation and generalizability limitations of our study, our study cohort was derived from a single institution. Thus, our cost estimates may not fully represent the general medical costs of NTM-PD management across South Korea. It is possible that NTM-PD patients included in our sample may have sought care for NTM-PD at other institutions before and during follow-up visits to Severance Hospital, which may result in higher healthcare systems perspective per-patient costs. However, annual per-patient NTM management costs reported from an earlier study in South Korea that used the national health insurance claims database (healthcare systems perspective) (US $1,197.75/y) were equivalent to (or slightly lower than) our cost estimates (US $1,319/y) (21). Although we are not able to directly compare the 2 studies by using patient-level data, similarities in the cost estimates suggest that many NTM patients may be managed at a single institution and that our estimates closely represent those of general NTM patients in South Korea. Although it is difficult to ascertain and attribute differences in NTM-PD medical costs attributed to patients in South Korea compared with those in other countries, similarities in the overall trends (key cost drivers by types of healthcare use and types of diseases) suggest that the magnitude of our estimates largely represents differences in clinical practices and medical service costs across other countries with similar estimates. Second, we were limited in assessing any additional NTM-PD–related costs that patients and the healthcare systems may have incurred, such as nonmedical costs and productivity loss. Therefore, our cost estimates may underestimate true costs for NTM-PD management. Data from patient cost survey studies (to ascertain short- and long-term patient costs) and large panel data comprising multi-institutional cohorts with medical insurance claims information may provide a complete disease and financial burden of NTM-PD. Last, although we compared the costs associated with NTM-PD with those associated with other respiratory conditions, lack of an adequate control group with no history of NTM-PD limited our assessment of the relative disease and financial burden of NTM-PD.
In conclusion, our comprehensive, long-term assessment of medical costs associated with NTM-PD management demonstrates that NTM-PD poses a substantial disease burden on and financial costs to healthcare services and patients. Our findings suggest that the cost burden is considerably higher for patients with M. abscessus infection or pulmonary comorbidities, which is attributable to the longer duration of disease management and more frequent and longer hospitalization required. In addition, unlike patients with other respiratory infection–related illnesses, patients with NTM-PD bear much larger direct out-of-pocket costs that account for approximately 50% of direct medical costs. Although additional evidence from more complete data sources may be needed to fully ascertain long-term disease burden and costs, our study findings provide initial evidence that can be used for developing policies to support patients with NTM-PD and alleviate financial burdens during their disease management.
Dr. Chang is a clinical fellow of pulmonary and critical care medicine at Severance Hospital of Yonsei University in Seoul. His primary research interests include respiratory infections.
Acknowledgments
The data that support the findings of this study are available from the corresponding author (Y.P.) upon reasonable request.
This research was supported by the “Korea Disease Control and Prevention Agency (KDCA)” research project (project #20211111777-00).
Authors have no conflicts of interest to declare.
Authors met the criteria for authorship recommended by the International Committee of Medical Journal Editors, were fully responsible for all content, and were involved in all stages of manuscript development. Study conception and design: Y.A.K., H.S., Y.P.; data collection: S.C., S.K.; Y.A.K., M.S.P., and Y.P; and data interpretation: S.C., Y.A.K., H.S., and Y.P.
References
- Jeon D. Infection source and epidemiology of nontuberculous mycobacterial lung disease. Tuberc Respir Dis (Seoul). 2019;82:94–101. DOIPubMedGoogle Scholar
- Daley CL, Iaccarino JM, Lange C, Cambau E, Wallace RJ Jr, Andrejak C, et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Clin Infect Dis. 2020;71:e1–36. DOIPubMedGoogle Scholar
- Stout JE, Koh WJ, Yew WW. Update on pulmonary disease due to non-tuberculous mycobacteria. Int J Infect Dis. 2016;45:123–34. DOIPubMedGoogle Scholar
- Griffith DE, Aksamit TR. Managing Mycobacterium avium complex lung disease with a little help from my friend. Chest. 2021;159:1372–81. DOIPubMedGoogle Scholar
- Adjemian J, Prevots DR, Gallagher J, Heap K, Gupta R, Griffith D. Lack of adherence to evidence-based treatment guidelines for nontuberculous mycobacterial lung disease. Ann Am Thorac Soc. 2014;11:9–16. DOIPubMedGoogle Scholar
- Pasipanodya JG, Ogbonna D, Deshpande D, Srivastava S, Gumbo T. Meta-analyses and the evidence base for microbial outcomes in the treatment of pulmonary Mycobacterium avium-intracellulare complex disease. J Antimicrob Chemother. 2017;72(suppl_2):i3–19. DOIPubMedGoogle Scholar
- Pasipanodya JG, Ogbonna D, Ferro BE, Magombedze G, Srivastava S, Deshpande D, et al. Systematic review and meta-analyses of the effect of chemotherapy on pulmonary Mycobacterium abscessus outcomes and disease recurrence. Antimicrob Agents Chemother. 2017;61:e01206–17. DOIPubMedGoogle Scholar
- Lee H, Myung W, Koh WJ, Moon SM, Jhun BW. Epidemiology of nontuberculous mycobacterial infection, South Korea, 2007–2016. Emerg Infect Dis. 2019;25:569–72. DOIPubMedGoogle Scholar
- Winthrop KL, Marras TK, Adjemian J, Zhang H, Wang P, Zhang Q. Incidence and prevalence of nontuberculous mycobacterial lung disease in a large U.S. managed care health plan, 2008–2015. Ann Am Thorac Soc. 2020;17:178–85. DOIPubMedGoogle Scholar
- Ballarino GJ, Olivier KN, Claypool RJ, Holland SM, Prevots DR. Pulmonary nontuberculous mycobacterial infections: antibiotic treatment and associated costs. Respir Med. 2009;103:1448–55. DOIPubMedGoogle Scholar
- Leber A, Marras TK. The cost of medical management of pulmonary nontuberculous mycobacterial disease in Ontario, Canada. Eur Respir J. 2011;37:1158–65. DOIPubMedGoogle Scholar
- Diel R, Jacob J, Lampenius N, Loebinger M, Nienhaus A, Rabe KF, et al. Burden of non-tuberculous mycobacterial pulmonary disease in Germany. Eur Respir J. 2017;49:
1602109 . DOIPubMedGoogle Scholar - Ramsay LC, Shing E, Wang J, Marras TK, Kwong JC, Brode SK, et al. Costs associated with nontuberculous mycobacteria infection, Ontario, Canada, 2001–2012. Emerg Infect Dis. 2020;26:2097–107. DOIPubMedGoogle Scholar
- Goring SM, Wilson JB, Risebrough NR, Gallagher J, Carroll S, Heap KJ, et al. The cost of Mycobacterium avium complex lung disease in Canada, France, Germany, and the United Kingdom: a nationally representative observational study. BMC Health Serv Res. 2018;18:700. DOIPubMedGoogle Scholar
- Health Insurance Review and Assessment Service. Reimbursed drugs and price ceilings [cited 2022 May 12]. https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA030014050000
- US Internal Revenue Service. Yearly average currency exchange rates [cited 2024 Feb 1]. https://www.irs.gov/individuals/international-taxpayers/yearly-average-currency-exchange-rates
- Korean Statistical Information Service. Annual consumer price index by expenditure category [cited 2024 Feb 1]. https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1J22135&vw_cd=MT_ETITLE&list_id=P2_6&scrId=&language=en&seqNo=&lang_mode=en&obj_var_id=&itm_id=&conn_path=MT_ETITLE&path=%252Feng%252FstatisticsList%252FstatisticsListIndex.do
- Lee YJ, Kwon SH, Hong SH, Nam JH, Song HJ, Lee JS, et al. Health care utilization and direct costs in mild, moderate, and severe adult asthma: a descriptive study using the 2014 South Korean Health Insurance Database. Clin Ther. 2017;39:527–36. DOIPubMedGoogle Scholar
- Lee S, Kim MJ, Lee SH, Kim HY, Kim HS, Oh IH. Comparison of disability-adjusted life years (DALYs) and economic burden on people with drug-susceptible tuberculosis and multidrug-resistant tuberculosis in Korea. Front Public Health. 2022;10:
848370 . DOIPubMedGoogle Scholar - Lee HY, Han DJ, Kim KJ, Kim TH, Oh YM, Rhee CK. Clinical characteristics and economic burden of tuberculous-destroyed lung in Korea: a National Health Insurance Service-National Sample Cohort-based study. J Thorac Dis. 2019;11:2324–31. DOIPubMedGoogle Scholar
- Lee SW, Chang S, Park Y, Kim S, Sohn H, Kang YA. Healthcare use and medical cost before and after diagnosis of nontuberculous mycobacterial infection in Korea: the National Health Insurance Service-National Sample Cohort Study. Ther Adv Respir Dis. 2023;17:
17534666221148660 . DOIPubMedGoogle Scholar - Ruger JP, Kim HJ. Out-of-pocket healthcare spending by the poor and chronically ill in the Republic of Korea. Am J Public Health. 2007;97:804–11. DOIPubMedGoogle Scholar
- Organization for Economic Cooperation and Development. Health at a glance 2021 [cited 2024 Jul 22]. https://www.oecd-ilibrary.org
- Marras TK, Mirsaeidi M, Chou E, Eagle G, Zhang R, Leuchars M, et al. Health care utilization and expenditures following diagnosis of nontuberculous mycobacterial lung disease in the United States. J Manag Care Spec Pharm. 2018;24:964–74. DOIPubMedGoogle Scholar
- Chung WJ, Kim HJ. Interest groups’ influence over drug pricing policy reform in South Korea. Yonsei Med J. 2005;46:321–30. DOIPubMedGoogle Scholar
- Griffith DE, Daley CL. Treatment of Mycobacterium abscessus pulmonary disease. Chest. 2022;161:64–75. DOIPubMedGoogle Scholar
- Kang J, Park J, Cho J. Inclusive aging in Korea: eradicating senior poverty. Int J Environ Res Public Health. 2022;19:2121. DOIPubMedGoogle Scholar
- Park JH, Shin S, Kim TS, Park H. Clinically refined epidemiology of nontuberculous mycobacterial pulmonary disease in South Korea: overestimation when relying only on diagnostic codes. BMC Pulm Med. 2022;22:195. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: August 13, 2024
1These first authors contributed equally to this article.
2These authors were co–principal investigators.
Table of Contents – Volume 30, Number 9—September 2024
| EID Search Options |
|---|
|
|
|
|
|
|


Please use the form below to submit correspondence to the authors or contact them at the following address:
Youngmok Park, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Yonsei University College of Medicine, Severance Hospital, 50-1 Yonsei-ro, Seodaemun–gu, 03722 Seoul, South Korea
Top