Volume 31, Number 6—June 2025
Dispatch
Oral Flea Preventive to Control Rickettsia typhi–Infected Fleas on Reservoir Opossums, Galveston, Texas, USA, 2023–2024
Abstract
Murine typhus, a fleaborne bacterial disease caused by Rickettsia typhi, has reemerged and spread in the United States. We tested spinosad, an oral flea preventive, in opossum flea reservoirs. Spinosad killed 98% of fleas infesting opossums. Oral preventives could control fleas in host species and curb murine typhus spread to humans.
Rickettsia typhi is a fleaborne bacterium that causes murine typhus, an acute undifferentiated febrile illness, in humans (1). The organism is classically maintained by rats and transmitted by their fleas (Xenopsylla cheopis). In the United States, the incidence of murine typhus drastically fell after campaigns to control rat fleas with DDT (2). In the past decade, murine typhus has reemerged in the United States and alarmingly increased in incidence and geographic distribution (3). In endemic areas of North America, murine typhus has been associated with a transmission cycle involving opossums (Didelphis virginiana) and cat fleas (Ctenocephalides felis) (1).
One way to reduce murine typhus is field-based control of fleas that transmit R. typhi to humans. Spinosad (Comfortis; Elanco, https://farmanimal.elanco.com) is an orally ingested medication (comprising spinosyn A and spinosyn D) approved for use in dogs and cats. A single monthly dose is highly effective in killing fleas by activating nicotinic acetylcholine receptors, leading to flea paralysis and death (4). We tested effectiveness of spinosad for killing fleas on opossums in a murine typhus–endemic area. The study was approved by the University of Texas Medical Branch Institutional Animal Care and Use Committee (protocol no. 2104030) and Texas Parks and Wildlife (scientific permit no. SPR-1020154).
To capture opossums, we deployed Havahart 1-door cage traps (81 cm × 31 cm × 25 cm) (Woodstream Corporation, https://www.woodstream.com) in Galveston, Texas, USA, during evening hours. We conducted 2 arms, comprising an experimental group and a control group. In the experimental group, we baited traps with canned cat food mixed with a crushed 270-mg spinosad tablet. In the control group, we trapped opossums using cat food without spinosad in the bait.
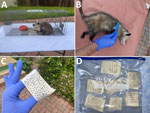
Spinosad starts to kill fleas within 30 minutes, and studies show it can kill 100% of fleas within 4 hours of ingestion in dogs and within 24 hours in cats (4). To collect dead fleas fallen from opossums, we placed a white terrycloth towel (160 cm × 84 cm) under the trap (Figure; Video). To ensure trapped opossums ingested bait at least 2 hours before flea collection, we checked traps between 4 am and 6 am the morning after setting.
We used intramuscular ketamine (30 mg/kg) to anesthetize trapped opossums. After adequate sedation, we collected fleas by combing through the fur with a flea comb (Hartz, https://www.hartz.com) for 15 minutes, then placed fleas on masking tape and secured in sealable plastic storage bags (Figure, panels B–D). After we collected fleas from the anesthetized opossum, we collected fleas from the towel. During collections, we observed flea activity and considered moving fleas to be alive and fleas without movement to be dead. All opossums recovered uneventfully from anesthesia and were released at a distant site to avoid subsequent trapping of the same animal. We caught 3 off-target species (1 raccoon and 2 cats) and released those animals on-site without intervening procedures.
We captured 9 opossums over 19 trap nights: 5 in the experimental group and 4 in control group (Table 1). Six (66.7%) were female and 3 (33.3%) were male. The mean weight was 2.1 kg. All opossums completely ingested food within the trap. We observed fleas on all 9 opossums. Among the opossums that ingested spinosad, fleas were largely immobile and easily combed from fur; fleas were also numerous on the towel and were easily collected and bagged (Figure, panels C, D). In contrast, fleas in the control group moved rapidly within the opossums’ fur; were difficult to comb off, often jumping off the comb; and would frequently escape from the tape after being bagged.
We examined collected fleas with a dissecting microscope and identified flea species by taxonomic key (5). We pooled fleas (dead and alive) in groups of 5–20 fleas based on the animal from which they were collected. We homogenized a subset of pools from each opossum and extracted DNA, as previously described (6). We used a multiplex real-time PCR to amplify and identify R. typhi and R. felis from flea homogenates (7).
We compared the proportion of dead fleas from the experimental and control groups. Because those proportions were bounded by 0 and 1, we transformed proportions by taking the arcsine of their square root (8). We needed sample sizes of at least 3 opossums in the experimental and 2 in the control groups to achieve 82% power to reject the null hypothesis with a significance level (α) of 0.05 using a 2-sided 2-sample equal-variance t-test. We determined rates of R. typhi and R. felis flea infection by using previously described methods (9) (Appendix).
We collected a total of 2,047 fleas and identified all as Ct. felis. The proportion of dead fleas from opossums in the experimental group was 0.98 (range 0.92–1) compared with 0 (p<0.001) in the control group (Table 1).
We tested 71 pools (comprising 744 fleas) by PCR; 11 pools demonstrated R. typhi DNA, and 23 pools demonstrated R. felis DNA (Table 2). Those findings correspond to an infection rate of 1.3% (95% CI 0.7–2.2) for R. typhi and 3.2% (95% CI 2.2–7.9) for R. felis. Sequenced PCR products of portions of rickettsial htrA (GenBank accession no. PQ625781) and sca5 (GenBank accession no. PQ625780) of an R. typhi–infected flea pool detected by real-time PCR confirmed 100% homology with R. typhi Wilmington type strain.
In this study, we showed that commercially available spinosad (approximately $20 per tablet) effectively kills fleas infesting opossums. The observed animals readily fed on bait laced with the medication, and almost 100% of collected fleas were found dead at least 2 hours after opossums ingested the preventive. Although spinosad caused mild side effects (e.g., vomiting) in dogs and cats in controlled studies (4), little data on adverse effects in other species are available. Although we noticed no ill effects in opossums in this study, the sample size was small.
Consistent with other areas of the United States where murine typhus is endemic, we detected R. typhi in cat fleas collected from opossums (6,10). In contrast, other reports show few fleas collected from domestic cats are infected with R. typhi (11,12).
Targeted efforts to control rat fleas via application of DDT on rat runs and harborages during the 1940s and 1950s exemplify how vector control can break the cycle of vectorborne disease transmission. In 1944, murine typhus peaked at 5,401 reported cases, but that number fell to <100 reported cases annually by the mid-1950s after introduction of DDT (2,3). However, the effects of DDT seemed to have little spillover into opossums (13), and the lingering low-level endemicity of murine typhus in the United States was eventually attributed to an alternate R. typhi transmission cycle involving opossums and cat fleas (1,3). Those findings support the need to focus flea control efforts on opossums in murine typhus endemic areas of the United States. More research is required to investigate the proposed methods’ feasibility, effectiveness in nonexperimental conditions, logistics and toxicity among nontarget species, and effects on disease transmission in murine typhus endemic areas. For instance, in high-burden disease locations, field-deployable methods could include manual dispersion of spinosad-impregnated food pellets or timed-release dispenser stations placed at strategic distances.
In conclusion, the growing distribution and incidence of murine typhus in the United States are a call to develop and implement integrated pest control strategies to aid public health prevention (14,15). We found that oral flea preventive effectively controlled R. typhi flea vectors in reservoir opossums. The proposed method could be used to control vector fleas among reservoir hosts and reduce risk for murine typhus in humans.
Dr. Blanton is an infectious disease physician at the University of Texas Medical Branch in Galveston, Texas. His research interests are focused on the study of rickettsial diseases.
Dr. Villasante-Tezanos is a biostatistician at the University of Texas Medical Branch. His research interests include clinical trials and nonparametric statistics.
Acknowledgment
We thank Matthew Dacso and Susan McLellan for allowing trappings on their properties. We also thank David Walker for his mentorship and review of the manuscript.
References
- Civen R, Ngo V. Murine typhus: an unrecognized suburban vectorborne disease. Clin Infect Dis. 2008;46:913–8. DOIPubMedGoogle Scholar
- Pratt HD. The changing picture of murine typhus in the United States. Ann N Y Acad Sci. 1958;70:516–27. DOIPubMedGoogle Scholar
- Anstead GM. History, rats, fleas, and opossums. II. The decline and resurgence of flea-borne typhus in the United States, 1945–2019. Trop Med Infect Dis. 2020;6:2. DOIPubMedGoogle Scholar
- Elanco Animal Health. Comfortis (spinosad) package insert [cited 2025 March 7]. https://assets-eu-01.kc-usercontent.com/ad0f862a-9fb6-0162-80e8-2abe0fae68af/c1680843-25ec-4a2a-a152-2a1dacbcf4d2/Comfortis_Pack_Insert.pdf
- Communicable Diseases Center. Pictorial keys to arthropods, reptiles, birds, and mammals of public health significance, 1966 [cited 2025 Mar 7]. https://stacks.cdc.gov/view/cdc/13428
- Blanton LS, Idowu BM, Tatsch TN, Henderson JM, Bouyer DH, Walker DH. Opossums and cat fleas: new insights in the ecology of murine typhus in Galveston, Texas. Am J Trop Med Hyg. 2016;95:457–61. DOIPubMedGoogle Scholar
- Karpathy SE, Hayes EK, Williams AM, Hu R, Krueger L, Bennett S, et al. Detection of Rickettsia felis and Rickettsia typhi in an area of California endemic for murine typhus. Clin Microbiol Infect. 2009;15(Suppl 2):218–9. DOIPubMedGoogle Scholar
- Sokal RR, Rohlf FJ. Biometry: the principles and practice of statistics in biological research. Third edition. New York: W.H. Freeman and Co; 1995.
- Biggerstaff BJ. Confidence intervals for the difference of two proportions estimated from pooled samples. J Agric Biol Environ Stat. 2008;13:478–96. DOIGoogle Scholar
- Maina AN, Fogarty C, Krueger L, Macaluso KR, Odhiambo A, Nguyen K, et al. Rickettsial infections among Ctenocephalides felis and host animals during a flea-borne rickettsioses outbreak in Orange County, California. PLoS One. 2016;11:
e0160604 . DOIPubMedGoogle Scholar - Mullins KE, Maina AN, Krueger L, Jiang J, Cummings R, Drusys A, et al. Rickettsial infections among cats and cat fleas in Riverside County, California. Am J Trop Med Hyg. 2018;99:291–6. DOIPubMedGoogle Scholar
- Nelson K, Maina AN, Brisco A, Foo C, Croker C, Ngo V, et al. A 2015 outbreak of flea-borne rickettsiosis in San Gabriel Valley, Los Angeles County, California. PLoS Negl Trop Dis. 2018;12:
e0006385 . DOIPubMedGoogle Scholar - Mohr CO, Morlan HB. The nature of parasitism of the opossum by fleas in southwestern Georgia. J Parasitol. 1959;45:233–7. DOIPubMedGoogle Scholar
- Yomogida K, Kjemtrup A, Martínez-López B, Ibrahim M, Contreras Z, Ngo V, et al. Surveillance of flea-borne typhus in California, 2011–2019. Am J Trop Med Hyg. 2023;110:142–9. DOIPubMedGoogle Scholar
- Murray KO, Evert N, Mayes B, Fonken E, Erickson T, Garcia MN, et al. Typhus group rickettsiosis, Texas, USA, 2003–2013. Emerg Infect Dis. 2017;23:645–8. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: May 13, 2025
Table of Contents – Volume 31, Number 6—June 2025
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Lucas S. Blanton, University of Texas Medical Branch, 301 University Blvd, Galveston, TX 77555-0435, USA
Top