Volume 31, Number 7—July 2025
Research Letter
Syphilitic Aortitis with Concomitant Neurosyphilis in Asymptomatic Patient
Cite This Article
Citation for Media
Abstract
We report a rare case of syphilitic aortitis with possible neurosyphilis in an asymptomatic 89-year-old man in Washington, DC, USA. This case highlights the need to consider emerging infectious causes of aortitis, even in patients without classic risk factors, by using multimodality imaging with confirmatory serologic and cerebrospinal fluid testing.
Syphilitic aortitis is exceptionally rare. However, syphilis, caused by the bacterium Treponema pallidum, has reemerged as a global public health concern, and the Centers for Disease Control and Prevention has reported >200,000 cases in the United States in 2022 (1). After 10–30 years, ≈10% of untreated persons will develop syphilitic aortitis. Early recognition and treatment are imperative to avoid high rates of death (2), although the broad differential of aortitis can complicate diagnosis. In this article, we describe a rare case of syphilitic aortitis in an asymptomatic, elderly patient in which using imaging, serology, and epidemiologic context helped guide diagnosis.
An 89-year-old man with a history of chronic lymphedema, deep vein thrombosis, and peripheral artery disease sought care at Georgetown University Hospital in Washington, DC, USA, having experienced 1 week of right leg erythema and swelling. At admission, his laboratory results revealed leukocytosis and elevated inflammatory markers. Computed tomography (CT) of the patient’s right leg revealed soft tissue changes consistent with cellulitis unresponsive to antimicrobial drugs. Because of the concern for sepsis, we broadened the patient’s antimicrobial regimen, and an infectious disease consultation prompted further evaluation for alternative sources.
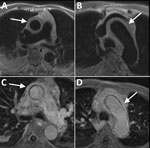
Contrast-enhanced CT of the chest showed circumferential soft tissue enhancement of the ascending aorta, aortic arch, and branching vessels, suggestive of aortitis versus intramural hematoma (Appendix Figure). Follow-up magnetic resonance angiography confirmed a diagnosis of aortitis (Figure). We consulted rheumatology because of the patient’s elevated inflammatory markers but had low suspicion for autoimmune disease after more specific antibody testing results were negative.
Because of our concern for an infectious etiology, we pursued serologic testing. Initial chemoluminescence immunoassay testing was reactive for syphilis, and subsequent rapid plasma reagin testing was positive with a 1:4 titer result. Despite no neurologic symptoms, we conducted cerebrospinal fluid (CSF) analysis that was negative by Venereal Disease Research Laboratory (VDRL) testing but positive for fluorescent treponemal antibody absorption. Full CSF results revealed a slightly elevated red blood cell count, slightly low monocytes, and unremarkable leukocyte and protein counts. Findings were inconsistent across all samples.
Ultimately, we attributed the patient’s underlying aortic pathology to syphilitic aortitis with concomitant neurosyphilis. The patient was treated with a 7-day course of intravenous penicillin G (3 million units every 4 h), and was prescribed the same treatment for an additional 7 days at discharge. The patient was discharged with reduced leg swelling, unremarkable vital signs, and resolved leukocytosis, but he was lost to follow-up.
This article describes the diagnosis of syphilitic aortitis with suspected neurosyphilis in an asymptomatic, elderly man with no classic symptoms or risk factors after using multimodality imaging and confirmatory testing. At 89 years of age, this patient is unusual and has a rare manifestation of syphilis, which is again rising in prevalence.
Our patient reported no cardiovascular symptoms, no prior syphilis diagnosis or treatment, no recollection of genital lesions, and no history of high-risk sexual behavior. Of note, he resided in Washington, DC, where syphilis rates are among the highest in the United States and have increased each year (3). Those data underscore the importance of considering T. pallidum infection in patients from high-risk areas, even in the absence of symptoms or traditional risk factors. Prompt treatment is critical, because some cases of syphilitic aneurysmal formation confer a 2-year mortality rate >80% (4). However, recognizing syphilitic aortitis can be challenging because of longstanding limitations in diagnostic strategies.
For source identification and subsequent control, whole-body imaging is typically indicated. Although CT imaging is sufficient for most aortopathies (2), it cannot reliably differentiate between hematoma and aortitis because of tissue density matching. Accordingly, a magnetic resonance aortogram provided further delineation of the abnormality, which was more indicative of aortitis than a hematoma because a hematoma is usually irregularly shaped and primarily diagnosed by using density-based imaging such as CT. Although not used in this case, fluorodeoxyglucose positron emission tomography/CT can be useful to evaluate differential causes of unexplained fever associated with vasculitis and ascertain treatment efficacy in cases of tertiary syphilis (5–7).
After ruling out more common autoimmune diseases, we chose treponemal-specific chemoluminescence immunoassay testing for suspicion of syphilitic aortitis. We selected this reverse sequence strategy because of institutional preference and high pretest probability (8), and a positive rapid plasma reagin titer of 1:4 confirmed active syphilis. Furthermore, diffuse syphilitic disease of the aorta necessitated CSF testing (9), showing negative VDRL and positive fluorescent treponemal antibody absorption. VDRL testing has poor sensitivity, and fluorescent treponemal antibody absorption has poor specificity. Fluorescent treponemal antibody absorption might be influenced by trace red blood cell contamination from the CSF (10). Nonetheless, intravenous penicillin G was initiated because of patient preference and the risk of not treating our elderly patient.
Syphilitic aortitis remains a rare but challenging diagnosis, especially in patients without typical symptoms or risk factors. This report highlights the importance of stepwise imaging and serologic testing in identifying syphilitic aortitis. CT scan is a reasonable first radiographic study, but magnetic resonance imaging can better define the underlying etiology. As syphilis cases continue to rise, clinicians should use local epidemiologic trends to ensure early disease detection.
Dr. Czulada graduated from Georgetown University School of Medicine in 2025 and is currently an internal medicine resident at Emory University Hospital in Atlanta, GA. His research interests include cardiac electrophysiology and the intersection of cardiology and infectious disease, with a special focus on Chagas cardiomyopathy.
Acknowledgment
We thank the patient for his consent to publish this case study.
References
- Centers for Disease Control and Prevention. Sexually transmitted infections surveillance, 2023 [cited 2024 Jul 5]. https://www.cdc.gov/sti-statistics/media/pdfs/2024/11/2022-STI-Surveillance-Report-PDF.pdf
- Bley TA, Francois CJ. Inflammatory and infectious vascular disorders. In: Abbara S, Kalva SP, editors. Problem solving in cardiovascular imaging. Philadelphia: Elsevier; 2013. p. 412–22.
- Health DC. 2023 Annual Epidemiology & Surveillance Report. 2023 [cited 2025 Apr 21]. https://dchealth.dc.gov/sites/default/files/dc/sites/doh/publication/attachments/2023-Annual-Surveillance-Report-v13.pdf
- Girardi LN. Syphilitic aortitis: The bigger picture. J Thorac Cardiovasc Surg. 2017;154:e27–8. DOIPubMedGoogle Scholar
- Kim J, Song HC. Role of PET/CT in the evaluation of aortic disease. Chonnam Med J. 2018;54:143–52. DOIPubMedGoogle Scholar
- Kalbi D, Li A, Hari A, Chun K. The utility of 18F-FDG PET/CT in active aortitis: a case study and literature review. J Nucl Med. 2023;64(S1):1230.
- Hayashida T, Sueyoshi E, Sakamoto I, Uetani M, Chiba K. PET features of aortic diseases. AJR Am J Roentgenol. 2010;195:229–33. DOIPubMedGoogle Scholar
- Ortiz DA, Shukla MR, Loeffelholz MJ. The traditional or reverse algorithm for diagnosis of syphilis: pros and cons. Clin Infect Dis. 2020;71(Suppl 1):S43–51. DOIPubMedGoogle Scholar
- Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1–137.PubMedGoogle Scholar
- Hamill MM, Ghanem KG, Tuddenham S. State-of-the-Art Review: Neurosyphilis. Clin Infect Dis. 2024;78:e57–68. DOIPubMedGoogle Scholar
Figure
Cite This ArticleOriginal Publication Date: June 23, 2025
Table of Contents – Volume 31, Number 7—July 2025
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Evan Czulada, Emory University Hospital, 1364 Clifton Rd NE, Atlanta, GA 30322, USA
Top