Volume 7, Number 2—April 2001
THEME ISSUE
4th Decennial International Conference on Nosocomial and Healthcare-Associated Infections
State of the Art
Cost-Effective Infection Control Success Story: A Case Presentation
Cite This Article
Citation for Media
Abstract
In a surgical intensive care unit, the 1996-1997 incidence of central catheter-associated bloodstream infections exceeded that of hospitals participating in the National Nosocomial Infections Surveillance System. Interventions were implemented, and a cost-benefit analysis was done that led to hiring a vascular catheter care nurse. Subsequent outcome data demonstrated a substantial reduction in central catheter-associated bloodstream infections.
Most hospital-acquired bloodstream infections are associated with use of an intravascular device, specifically central venous catheters. Catheter-associated bloodstream infections occur more often in intensive care unit (ICU) patients than in ward patients. The attributable mortality rate for bloodstream infections in surgical ICUs has been estimated to be 35% (1). ICU-acquired bloodstream infections account for an estimated $40,000 increase in costs per survivor and an estimated $6,000 increase in hospital costs (2).
In 1997, the Centers for Disease Control and Prevention's (CDC) National Nosocomial Infections Surveillance System reported 0.4 to 9.2 bloodstream infections per 1,000 central-line days in patients in surgical ICUs. A mean of 5.1 and a median of 3.6 infections per 1,000 patient days was reported. Coagulase-negative staphylococcus was found to be the predominant microorganism responsible. In 1997, despite conventional infection prevention and control strategies, we identified a mean of 8.8 and a median of 8.9 catheter-associated bloodstream infections per 1,000 patient days in patients in a surgical ICU at Texas Medical Center. The predominant microorganism responsible for these catheter-associated bloodstream infections was coagulase-negative staphylococcus, which has been associated with a lower risk of death than other hospital-acquired bloodstream pathogens.
The Methodist Hospital, a tertiary-care facility in the Texas Medical Center with 900 beds, is affiliated with Baylor College of Medicine. The increased incidence of catheter-associated bloodstream infections was identified in a 32-bed surgical ICU. Prospective surveillance for device-related infection is performed in the surgical ICU by an experienced nurse epidemiologist. All positive cultures are reported to infection control by the microbiology laboratory. CDC's definition for catheter-associated bloodstream infection is used (3).
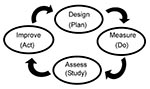
In response to the increased rate of infections, three working groups were formed to develop strategies for catheter selection, insertion, care, and maintenance; and clinical practice guidelines. Products and practices used in the ICU were reviewed, and a literature search was performed to identify best practices associated with insertion, care, and maintenance of central venous catheters, which formed the basis for the clinical practice guidelines. The Design, Measure, Assess, Improve model described by the Joint Commission on Accreditation of Healthcare Organizations was used to guide the plan of action (Figure).
The following recommendations were adopted by the Infection Prevention and Control Committee: use an antibiotic-coated catheter for patients expected to have the device in place for >7 days; disseminate the clinical practice guideline to surgeons, anesthesiologists, house staff, and nursing staff; dispense maximum barrier precaution supplies (i.e., gown, mask, gloves, and fenestrated drape with insertion tray); and hire a vascular catheter-care nurse for the surgical ICU. The nurse's responsibilities would include educating the house staff and nursing staff on the clinical practice guideline; observing practices associated with insertion, care, and maintenance of the central venous catheter system on all three shifts; collecting and analyzing outcome data related to bloodstream infections; and providing status reports to the nursing staff, medical staff, and the Infection Prevention and Control Committee.
A cost-benefit analysis was presented to the hospital administration to justify hiring the nurse, at a projected salary of $50,000. A cost of $6,000 per catheter-associated bloodstream infections was used. We proposed that adding the nurse to the staff would prevent at least one bloodstream infection per month, or 12 infections annually. This cost-benefit analysis approach was effective in securing approval for the position. A registered nurse with 15 years of surgical ICU experience at Methodist Hospital was hired in March 1999.
In January 2000, 9 months after joining the infection control team, the nurse reported that 18 fewer bloodstream infections occurred in 1999 than in 1998, for an estimated savings of $108,000, with no change noted in surgical ICU patient days. The 1999 mean bloodstream infection rate was 6.6 per 1,000 central-line days; the median was 6.7 per 1,000 central-line days (Table).
The pathogenesis of catheter-associated bloodstream infections is multifactorial. A multidisciplinary approach is necessary to develop and enforce corrective measures. Efforts to prevent bloodstream infections in the surgical ICU patient population are cost-effective from both the patient and hospital standpoint. We were able to effectively present a cost-benefit analysis to secure approval for a unique infection prevention and control position.
In a cost-benefit analysis, the outcome is presented in monetary terms (4). Another decision analysis tool, cost-effectiveness analysis, incorporates both the cost and the effect of the intervention. Cost-effectiveness analysis measures the net cost of providing a service as well as the outcome obtained. The outcomes are reported in a single unit of measurement, e.g., years of life saved, number of lives saved, or number of cases of a specific disease prevented (4,5). The advantage of cost-effectiveness analysis is that it considers the possibility of improved outcomes in exchange for the use of more resources. A cost-effectiveness analysis is planned to further justify the resource allocation of an ICU nurse to the position of vascular catheter-care nurse.
Dr. Slater is director of infection control, performance improvement, and decision support at Methodist Hospital, Houston, Texas. She is a past president of the Association for Professionals in Infection Control and Epidemiology and current President of the APIC Research Foundation.
References
- Pittet D, Wenzel RP. Nosocomial bloodstream infections--secular trends in rates, mortality, and contribution to total hospital deaths. Arch Intern Med. 1995;155:1177–84. DOIPubMedGoogle Scholar
- Pittet D, Tarara D, Wenzel RP. Nosocomial bloodstream infection in critically ill patients: excess length of stay, extra costs, and attributable mortality. JAMA. 1994;271:1598–601. DOIPubMedGoogle Scholar
- Garner JS. Guidelines for prevention of intravascular infections. The Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1996;17:53–80. DOIPubMedGoogle Scholar
- Eisenberg J. Clinical economics: a guide to the economic analysis of clinical practices. JAMA. 1989;262:2879–86. DOIPubMedGoogle Scholar
- Nettleman MD. Decision analysis: a tool for infection control. Infect Control Hosp Epidemiol. 1988;9:88–91. DOIPubMedGoogle Scholar
Figure
Table
Cite This ArticleTable of Contents – Volume 7, Number 2—April 2001
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Fran Slater, Infection Control Department, The Methodist Hospital, 6565 Fannin - Mailstation F-ll92, Houston, Texas 77030, USA; fax: 713-790-6413
Top