Volume 4, Number 2—June 1998
Perspective
Multidrug-Resistant Mycobacterium tuberculosis: Molecular Perspectives
Figure 1
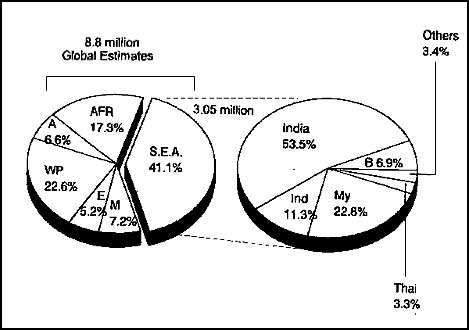
Figure 1. Global incidence of tuberculosis. Of the estimated 8.8 million cases worldwide, more than 40% of the cases are in Southeast Asia; India has approximately 53.3% of those cases. A, Americas; Afr, Africa; WP, Western Pacific; E, Europe; M, Eastern Mediterranean; and SEA, Southeast Asia; Ind, Indonesia; B, Bangladesh; Thai, Thailand; My, Myanmar. *Others include Bhutan, 0.05%; Nepal, 1.2%; Maldives, 0.001%; Sri Lanka, 1%; DPR Korea, 1.2%. (Data from reference 2).
References
- Bloom BR, Murray CJL. Tuberculosis: Commentary on a reemergent killer. Science. 1992;257:1055–64. DOIPubMedGoogle Scholar
- World Health Organization. Bridging the gaps: the world health report. Geneva: The Organization; 1995.
- World Health Organization report on TB epidemic. Global TB programme. Geneva: The Organization; 1997.
- Barnes P, Blotch AB, Davidson BT, Snyder DE Jr. Tuberculosis in patients with immuno-deficiency virus infection. N Engl J Med. 1991;324:1644–50.PubMedGoogle Scholar
- Kochi A, Vareldzis B, Styblo K. Multi-Drug resistant tuberculosis and control. Res Microbiol. 1993;144:104–10. DOIPubMedGoogle Scholar
- Bell RT. Tuberculosis of the 1990s: the quiet public health threat. Pa Med. 1992;95:24–5.PubMedGoogle Scholar
- Freiden TE, Sterling T, Pablos-Mendez A, Kilburn JO, Cauthen JO, Dooley SW. The emergence of drug-resistant tuberculosis in New York city. N Engl J Med. 1993;328:521–6. DOIPubMedGoogle Scholar
- Nosocomial transmission of multi-drug resistant tuberculosis among human immuno-deficiency virus infected patients—Florida and New York, 1988-1991. MMWR Morb Mortal Wkly Rep. 1991;40:585–91.PubMedGoogle Scholar
- Dooley SW, Jarvis WR, Martone WJ, Snyder DE Jr. Multi-Drug resistant tuberculosis [editorial]. Ann Intern Med. 1992;117:257–8.PubMedGoogle Scholar
- Edlin BR, Tokers JI, Greeko MH, Crawford JT, Williams J, Sordillo EM, An outbreak of multi-drug resistant tuberculosis among hospitalized patients with the Acquired Immuno-Deficiency syndrome. N Engl J Med. 1992;326:1514–21.PubMedGoogle Scholar
- Pearson ML, Jareb JA, Freiden TR, Crawford JT, Davis BJ, Dooley SN, Nosocomial transmission of multi-drug resistant tuberculosis—a risk to patients and health care workers. Ann Intern Med. 1992;117:191–6.PubMedGoogle Scholar
- Iseman MD, Sbarbaro JA. The increasing prevalence of resistance to antituberculosis chemotherapeutic agents: implications for global tuberculosis control. Curr Clin Top Infect Dis. 1992;12:188–204.PubMedGoogle Scholar
- Cohn DL, Flavia B, Raviglione MC. Drug-resistant tuberculosis: review of the worldwide situation and the WHO/IUATLD global surveillance project. Clin Infect Dis. 1997;24:S121–30.PubMedGoogle Scholar
- Initial therapy for tuberculosis in the era of multi-drug resistance: recommendations of the advisory council for the elimination of tuberculosis. MMWR Morb Mortal Wkly Rep. 1993;42(RR-7).
- Mitchison DA. Mechanism of drug action in short-course chemotherapy. Bull Int Union Tuberc. 1985;65:30–7.
- Iseman MD, Madsen LA. Drug-resistant tuberculosis. Clin Chest Med. 1989;10:341–53.PubMedGoogle Scholar
- Heifets LB, Lindohlm-Levy PJ. Pyrazinamide sterilizing activity in vitro against semidormant Mycobacterium tuberculosis populations. Am Rev Respir Dis. 1992;145:1223–5.PubMedGoogle Scholar
- Vareldzis BP, Grosset J, de Kantor I, Crofton J, Laszlo A, Felten M, Drug-resistant tuberculosis: laboratory issues. World Health Organization recommendations. Tuber Lung Dis. 1994;75:1–7. DOIPubMedGoogle Scholar
- Spratt BG. Resistance to antibiotics mediated by target alterations. Science. 1994;264:388–93. DOIPubMedGoogle Scholar
- Davis J. Inactivation of antibiotics and the dissemination of resistance genes. Science. 1994;264:375–82. DOIPubMedGoogle Scholar
- Shimao T. Drug-resistance in tuberculosis control. Tubercle. 1987;68(suppl):5–15.PubMedGoogle Scholar
- Crofton J. The assessment and treatment of drug-resistance problems in tuberculosis. J Ir Med Assoc. 1970;63:75–8.PubMedGoogle Scholar
- Grange JM. Drug-resistance and tuberculosis elimination. Bull Int Union Tuberc Lung Dis. 1990;65:57.PubMedGoogle Scholar
- Youatt J. A review of the action of isoniazid. Am Rev Respir Dis. 1969;99:729–49.PubMedGoogle Scholar
- Shoeb HA, Bowman BU Jr, Ottolenghi AC, Merola AJ. Peroxidase-mediated oxidation of isoniazid. Antimicrob Agents Chemother. 1985;27:399–403.PubMedGoogle Scholar
- Maggliozzo RS, Marcinkeviciene JA. Evidence for isoniazid oxidation by oxypressors mycobaterial catalase-oxidase. J Am Chem Soc. 1996;118:11303–4. DOIGoogle Scholar
- Middlebrook G. Isoniazid-resistance and catalase activity of tubercle bacilli. Am Rev Tuberc. 1954;69:471–2.PubMedGoogle Scholar
- Zhang Y, Heym B, Allen B, Young D, Cole S. The catalase-peroxidase gene and isoniazid resistance of Mycobacterium tuberculosis. Nature. 1992;358:591–3. DOIPubMedGoogle Scholar
- Zhang Y, Garbe T, Young D. Transformation with katG restores isoniazid-sensitivity in Mycobacterium tuberculosis isolates resistant to a range of drug concentrations. Mol Microbiol. 1993;8:521–4. DOIPubMedGoogle Scholar
- Demple B, Halbrook J. Inducible repair of oxidative DNA damage in Escherichia coli. Nature. 1983;304:466. DOIPubMedGoogle Scholar
- Sherman DR, Sabo PJ, Hickey MJ, Arain TM, Mahairas GG, Yuan Y, Disparate responses to oxidative stress in saprophytic and pathogenic mycobacteria. Proc Natl Acad Sci U S A. 1995;92:6625–9. DOIPubMedGoogle Scholar
- Sherman DR, Mdluli K, Hickey MJ, Arain TM, Morris SL, Barry CE III, Compensatory ahpC gene expression in isoniazid-resistant Mycobacterium tuberculosis. Science. 1996;272:1641–3. DOIPubMedGoogle Scholar
- Chae HZ, Robinson K, Leslie B, Church GB, Storz G, Rhee SG. Cloning and sequencing of thiol-specific antioxidant from mammalian brain, alkyl hydro-peroxide reductase and thiolspecific anti-oxidant define a large family of antioxidant enzymes. Proc Natl Acad Sci U S A. 1994;91:7017–21. DOIPubMedGoogle Scholar
- Chae HZ, Chung SJ, Rhee SG. Thioredoxin-dependent-peroxide reductase from yeast. J Biol Chem. 1994;269:276–0.
- Sreevatsan S, Pan X, Zhang Y, Deretic V, Muser JM. Analysis of the oxyR-ahpC region in isoniazid-resistant and -susceptible Mycobacterium tuberculosis complex organims recovered from diseased humans and animals in diverse localities. Antimicrob Agents Chemother. 1997;41:600–6.PubMedGoogle Scholar
- Heym B, Stavropoulos E, Honore N, Domenech P, Saint-Joanis B, Wilson TM, Effects of overexpression of the alkyl hydroperoxide reductase AhpC on the virulence and isoniazid resistance of Mycobacterium tuberculosis. Infect Immun. 1997;65:1395–401.PubMedGoogle Scholar
- Altamarino M, Marostenmaki J, Wong A, Fitzgerald M, Black WA, Smith JA. Mutations in the catalase-peroxidase gene from isoniazid-resistant Mycobacterium tuberculosis isolates. J Infect Dis. 1994;160:1162–5.
- Stoeckle MY, Guan L, Riegler N, Weitzman I, Kreiswirth B, Kornblum J, Catalase-peroxidase gene sequences in isoniazid-sensitive and -resistant strains of Mycobacterium tuberculosis from New York City. J Infect Dis. 1993;168:1063–5.PubMedGoogle Scholar
- Cockerill FR III, Uhi JR, Temesgen Z, Zhang Y, Stockman L, Roberts GD, Rapid identification of a point mutation of the Mycobacterium tuberculosis catalase-peroxidase (katG) gene associated with isoniazid resistance. J Infect Dis. 1995;171:240–5.PubMedGoogle Scholar
- Pretorius GS, Van Helden PD, Sergel F, Eisenach KD, Victor TC, Mutations in katG gene sequences in isoniazid-resistant clinical isolates of Mycobacterium tuberculosis are rare. Antimicrob Agents Chemother. 1995;39:2276–81.PubMedGoogle Scholar
- Heym B, Alzavi PM, Honore N, Cole ST. Missense mutations in the catalase-peroxidase gene, katG, are associated with isoniazid resistance in Mycobacterium tuberculosis. Mol Microbiol. 1995;15:235–45. DOIPubMedGoogle Scholar
- Rouse DA, Devito JA, Li Z, Byer M, Morris SL. Site-directed mutagenesis of the katG gene of Mycobacterium tuberculosis: effects on catalase-peroxidase activities and isoniazid resistance. Mol Microbiol. 1996;22:583–92. DOIPubMedGoogle Scholar
- Jaber M, Rattan A, Kumar R. Presence of katG gene in isoniazid-resistant strains of Mycobacterium tuberculosis. J Clin Pathol. 1996;49:945–7. DOIPubMedGoogle Scholar
- Kalia A, Ahmad N, Rattan A. Diagnosis of multi-drug resistant tuberculosis: comparison of traditional, radiometric and molecular methods [abstract]. In: Abstracts of the 20th International Congress of Chemotherapy; 29 Jun-3 Jul 1997; Sydney, Australia. Sydney: International Society of Chemotherapy; 1997. p. 211.
- Heym B, Honore N, Truffot-Pernot C, Banerjee A, Schurra C, Jacobs WR Jr, Implications of multidrug resistance for the future of short-course chemotherapy of tuberculosis: a molecular study. Lancet. 1994;344:293–8. DOIPubMedGoogle Scholar
- Kapur V, Li LL, Hamrick MR, Plikaytis BB, Shinnick TM, Telenti A, Rapid Mycobacterium species assignment and unambiguous identification of mutations associated with antibiotic resistance in Mycobacterium tuberculosis by automated DNA sequencing. Arch Pathol Lab Med. 1995;119:131–8.PubMedGoogle Scholar
- Morris SL. Bai Gh, Suffys P, Portillo-Gomez L, Fairchok M, Rouse D. Molecular mechanisms of multidrug resistance in clinical isolates of Mycobacterium tuberculosis. J Infect Dis. 1995;171:954–60.PubMedGoogle Scholar
- Johnsson K, Froland WA, Schultz PG. Overexpression, purification and characterization of the catalase-peroxidase, katG from Mycobacterium tuberculosis. J Biol Chem. 1997;272:2834–40. DOIPubMedGoogle Scholar
- Rouse DA, Li Z, Baig M, Morris SL. Characterization of the katG and inhA genes of isoniazid resistant clinical isolates of Mycobacterium tuberculosis. Antimicrob Agents Chemother. 1995;30:2472–7.
- Rosner JL. Susceptibility of oxyR regulon mutants of Escherichia coli and Salmonella typhimurium to isoniazid. Antimicrob Agents Chemother. 1993;37:2251–3.PubMedGoogle Scholar
- Deretic V, Philipp W, Dhandyuthapani S, Mudd MH, Curcic R, Garbe T, Mycobacterium tuberculosis is a natural mutant with an inactivated oxidative stress regulatory gene: implications for sensitivity to isoniazid. Mol Microbiol. 1995;17:889–900. DOIPubMedGoogle Scholar
- Wilson TM, Collins DM. ahpC, a gene involved in isoniazid resistance of Mycobacterium tuberculosis complex. Mol Microbiol. 1996;19:1025–34. DOIPubMedGoogle Scholar
- Banerjee A, Dubnau E, Quemard A, Balasubramanian V, Um KS, Wilson T, inhA, a gene encoding a target for isoniazid and ethionamide in Mycobacterium tuberculosis. Science. 1994;263:227–30. DOIPubMedGoogle Scholar
- Bergler H, Wallner P, Ebeling A, Leitinger B, Fuchshlschler S, Aschauer H, Protein EnvM is the NADH-dependent-enoyl-ACP-reductase (Fab1) of Escherichia coli. J Biol Chem. 1994;269:5493–6.PubMedGoogle Scholar
- Cole ST. Mycobacterium tuberculosis: drug-resistance mechanisms. Trends Microbiol. 1994;2:411–5. DOIPubMedGoogle Scholar
- Dessen A, Quemard A, Blanchard JS, Jacobs WR Jr, Sacchettini JC. Crystal structure and function of the isoniazid target of Mycobacterium tuberculosis. Science. 1995;267:1638–41. DOIPubMedGoogle Scholar
- Quemard A, Sacchettini JC, Dessen A, Jacobs WR Jr, Blanchard JS, Enzymatic characterization of the target for isoniazid in Mycobacterium tuberculosis. Biochemistry. 1995;34:8235–41. DOIPubMedGoogle Scholar
- Johnsson K, King DS, Schultz PG. Studies on the mechanism of action of isoniazid and ethionamide in chemotherapy of tuberculosis. J Am Chem Soc. 1995;117:5009–10. DOIGoogle Scholar
- Takayama K, Schoenes HK, Armstrong EL, Boyle KW. Site of inhibitory action of isoniazid in the synthesis of mycolic acids in Mycobacterium tuberculosis. J Lipid Res. 1975;16:308–17.PubMedGoogle Scholar
- Davidson LA, Takayma K. Isoniazid inhibition of the synthesis of mono-saturated long chain fatty acids in Mycobacterium tuberculosis H37Ra. Antimicrob Agents Chemother. 1979;16:104–5.PubMedGoogle Scholar
- Mdluli K, Sherman DR, Hickey MJ, Kreiswirth BN, Morris S, Stover CK, Biochemical and genetic data suggest that inhA is not the primary target for activated isoniazid in Mycobacterium tuberculosis. J Infect Dis. 1996;174:1085–90.PubMedGoogle Scholar
- Woodley CL, Kilburn JO, David HL, Silcox VA. Susceptibility of mycobacteria to rifampin. Antimicrob Agents Chemother. 1972;2:245–9.PubMedGoogle Scholar
- Ovchinnikov YA, Monastyrskaya GS, Gubanov VV, Lipkin VM, Sverdlov ED, Kiver IF, Primary structure of Escherichia coli RNA polymerase nucleotide substitution in the ß-subunit gene of rifampicin resistant rpoB255 mutant. Mol Gen Genet. 1981;84:536–8. DOIGoogle Scholar
- Levin ME, Hatfull GF. Mycobacterium smegmatis RNA polymerase: DNA supercoiling, action of rifampicin and mechanism of rifampicin resistance. Mol Microbiol. 1993;8:277–85. DOIPubMedGoogle Scholar
- Ovchinnikov YA, Monastryskaya GS, Gubanov VV, Lipkin VM, Sverdlov ED, Kiver IF, The primary structure of Escherichia coli RNA polymerase. Nucleotide sequence of rpoB gene and amino-acid sequence of the ß-subunit. Eur J Biochem. 1981;116:621–9. DOIPubMedGoogle Scholar
- Jin D, Gross C. Mapping and sequencing of mutations in the Escherichia coli rpoB gene that leads to rifampicin resistance. J Mol Biol. 1988;202:45–58. DOIPubMedGoogle Scholar
- Telenti A, Imboden P, Marchesi F, Lowrie D, Cole S, Colston MJ, . Detection of rifampicin-resistance mutations in Mycobacterium tuberculosis. Lancet. 1993;341:647–50. DOIPubMedGoogle Scholar
- Telenti A, Imboden P, Marchesi F, Schidheini T, Bodmer T. Direct, automated detection of rifampicin-resistant Mycobacterium tuberculosis by polymerase chain reaction and single-strand conformation polymorphism analysis. Antimicrob Agents Chemother. 1993;37:2054–8.PubMedGoogle Scholar
- Williams DL, Waguespack C, Eisenach K, Crawford JT, Portaels M, Salfinger M, Characterization of rifampicin-resistance in pathogenic mycobacteria. Antimicrob Agents Chemother. 1994;38:2380–6.PubMedGoogle Scholar
- Kapur V, Li LL, Iordanescu S, Hamrick MR, Wanger A, Kreisworth RN, Characterization by automated DNA sequencing of mutations in the gene (rpoB) encoding the RNA polymerase ß-subunit in rifampicin-resistant Mycobacterium tuberculosis strains from New York City and Texas. J Clin Microbiol. 1994;32:1095–8.PubMedGoogle Scholar
- Felmlee TA, Liu Q, Whelen AC, Williams D, Sommer SS, Persing DH. Genotypic detection of Mycobacterium tuberculosis rifampin resistance: comparison of single strand conformation polymorphism and dideoxy fingerprinting. J Clin Microbiol. 1995;33:1617–23.PubMedGoogle Scholar
- Whelen AC, Felmlee TA, Hunt JM, Williams DL, Roberts GD, Stockman L, Direct genotype detection of Mycobacterium tuberculosis rifampicin resistance in clinical specimens by using single-tube heminested PCR. J Clin Microbiol. 1995;33:556–61.PubMedGoogle Scholar
- De Benhouwer , Lhiang HZ, Jannes G, Mijis W, Machtelinckx L, Rossau H, . Rapid detection of rifampin resistance in sputum and biopsy samples from tuberculosis patients by PCR and line probe assay. Tuber Lung Dis. 1995;76:425–30. DOIPubMedGoogle Scholar
- Cooksey RC, Morlock GP, Glickman S, Crawford JT. Evaluation of a line probe assay kit for characterization of rpoB mutations in rifampin resistant Mycobacterium tuberculosis isolates from New York City. J Clin Microbiol. 1997;35:1281–3.PubMedGoogle Scholar
- Telenti A, Persing DH. Novel strategies for the detection of drug resistance in Mycobacterium tuberculosis. Res Microbiol. 1996;147:73–9. DOIPubMedGoogle Scholar
- Kim BJ, Kim SY, Park B-H, Liu M-A, Park I-K, Bai GH, Mutations in the rpoB gene in Mycobacterium tuberculosis that ineterfere with PCR-single strand conformation polymorphism analysis for rifampin susceptibility testing. J Clin Microbiol. 1997;35:492–4.PubMedGoogle Scholar
- Thomas JP, Baughan CO, Wilkinson RG, Shephard RG. A new synthetic compound with anti-tuberculous activity in mice: ethambutol (dextro-2,2'-[ethylenediimino]-di-1-butonol). Am Rev Respir Dis. 1961;83:891–3.PubMedGoogle Scholar
- Masur H. Recommendations on prophylaxis and therapy for disseminated Mycobacterium avium complex disease in patients infected with HIV virus. N Engl J Med. 1993;329:828–33. DOIPubMedGoogle Scholar
- Rastoggi N, Goh KS. Action of 1-isonicotinyl-2-palmitoyl hydrazine against the Mycobacterium avium complex and enhancement of its activity by m-flurophenyl alanine. Antimicrob Agents Chemother. 1990;34:2061–4.PubMedGoogle Scholar
- Rastoggi N, Goh KS, Labrausse V. Activity of clathiromycin compared with those of other drugs against Mycobacterium paratuberculosis and further enhancement of its extracellular and intracellular activities by etham-butol. Antimicrob Agents Chemother. 1992;36:2843–6.PubMedGoogle Scholar
- Takayama K, Armstrong EL, Kunugi KA, Kilburn JO. Inhibition by ethambutol of mycolic acid transfer into the cell wall of Mycobacterium smegmatis. Antimicrob Agents Chemother. 1979;16:240–2.PubMedGoogle Scholar
- Kilburn JO, Takayama K. Effects of ethambutol on accumulation and secretion of trehalose mycolates and free mycolic acid in Mycobacterium smegmatis. Antimicrob Agents Chemother. 1981;20:401–4.PubMedGoogle Scholar
- Takayama K, Kilburn JO. Inhibition of synthesis of arabinogalactan by ethambutol in Mycobacterium smegmatis. Antimicrob Agents Chemother. 1989;33:1493–9.PubMedGoogle Scholar
- Wolucka BA, McNeil MR, de Hoffman E, Chojnaki T, Brennan PJ. Recognition of the lipid intermediate for arabinogalactan/arabinomanan biosynthesis and its relation to the mode of action ethambutol on mycobacteria. J Biol Chem. 1994;269:23328–35.PubMedGoogle Scholar
- Belanger AE, Besra GS, Ford ME, Mikusova K, Belisle JT, Brennan PJ, The embAB genes of Mycobacterium avium encode an arabinosyl transferase involved in cell wall arabinan biosynthesis that is the target for the antimycobacterial drug ethambutol. Proc Natl Acad Sci U S A. 1996;93:11919–24. DOIPubMedGoogle Scholar
- Telenti A, Philipp WJ, Sreevatsan S, Bernasconi C, Stockbauer KE, Weites B, The emb operon, a gene cluster of Mycobacetrium tuberculosis involved in resistance to ethambutol. Nat Med. 1997;3:567–70. DOIPubMedGoogle Scholar
- Sreevatsan S, Stockbauer KE, Pan X, Kreisworth BM, Moghazeh SL, Jacobs WR Jr, Ethambutol resistance in Mycobacterium tuberculosis: critical role of embB mutations. Antimicrob Agents Chemother. 1997;41:1677–81.PubMedGoogle Scholar
- Konno K, Nagayama H, Oka S. Nicotinamidase in mycobacteria: a method for distinguishing bovine type tubercle bacilli from other mycobacteria. Nature. 1959;184:1743–4. DOIPubMedGoogle Scholar
- Konno K, Feldman FM, McDermot W. Pyrazinamide susceptibility and amidase activity of tubercle bacilli. Am Rev Respir Dis. 1967;95:461–7.PubMedGoogle Scholar
- Mackaness GB. The intracellular activation of pyrazinamide and nicotinamide. Am Rev Tuberc. 1953;74:718–28.
- Scorpio A, Zhang Y. Mutations in pncA, a gene encoding pyrazinamidase/nicotinamidase, cause resistance to the antituberculous drug pyrazinamide in tubercle bacillus. Nat Med. 1996;2:662–7. DOIPubMedGoogle Scholar
- Sreevatsan S, Pan X, Zhang Y, Kreisworth BN, Musser JM. Mutations associated with pyrazinamide resistance in pncA of Mycobacterium tuberculosis complex organisms. Antimicrob Agents Chemother. 1997;41:636–40.PubMedGoogle Scholar
- Scorpio A, Lindholm-Levy P, Heifets L, Gilman R, Siddiqi S, Cynamon M, Characterization of pncA mutations in pyrazinamide resistant Mycobacterium tuberculosis. Antimicrob Agents Chemother. 1997;41:540–2.PubMedGoogle Scholar
- Hewlett D, Horn DL, Alfalfa C. Drug resistant tuberculosis: inconsistent results of pyrazinamide susceptibility testing. JAMA. 1995;273:916–7. DOIPubMedGoogle Scholar
- Scorpio A, Collins D, Whipple D, Cave D, Bates J, Zhang Y. Rapid differentiation of bovine and human tubercule bacilli based on a characteristic mutation in the bovine pyrazinamidase gene. J Clin Microbiol. 1997;35:106–10.PubMedGoogle Scholar
- Gay JD, de Young DR, Roberts GD. In vitro activities of norfloxacin and ciprofloxacin against Mycobacterium tuberculosis, M. avium complex, M chelonei, M. forfuitre, and M. kansasii. Antimicrob Agents Chemother. 1984;26:94–6.PubMedGoogle Scholar
- Gellert M, Mizuuchi K, O'Dea MH, Nash HA. DNA gyrase: an enzyme that introduces superhelical turns into DNA. Proc Natl Acad Sci U S A. 1976;73:3872–5. DOIPubMedGoogle Scholar
- Kirchausen T, Wang JC, Harrison SC. Purification of the subunits of Escherichia coli DNA gyrase and reconstitution of enzyme activity. Proc Natl Acad Sci U S A. 1978;75:1773–7. DOIPubMedGoogle Scholar
- Gellert M, O'Dea MH, Itoh T, Tomizava J. Novobiocin and coumeromycin inhibit DNA supercoiling catalyzed by DNA gyrase. Proc Natl Acad Sci U S A. 1976;73:4474–8. DOIPubMedGoogle Scholar
- Sugino A, Peebles CL, Kreuzer KN, Cozzarelli NR. Mechanism of action of Nalidixic acid: purification of Escherichia coli nalA gene product and its relationship to DNA gyrase and a novel nicking closing enzyme. Proc Natl Acad Sci U S A. 1977;74:4667–71. DOIGoogle Scholar
- Kirkegaard K, Wand JC. Mapping the topography of DNA wrapped around gyrase by nucleolytic and chemical probing of complexes of unique DNA sequences. Cell. 1981;23:721–9. DOIPubMedGoogle Scholar
- Shen LL, Pernet AG. Mechanism of inhibition of DNA gyrase by analogues of nalidixic acid: the target of the drugs is the DNA gyrase. Proc Natl Acad Sci U S A. 1985;82:307–11. DOIPubMedGoogle Scholar
- Wilmont CJR, Critchlow SE, Eperon IC, Maxwell A. The complex of DNA gyrase and quinolone drugs with DNA forms a barrier to transcription by RNA polymerase. J Mol Biol. 1994;242:351–63. DOIPubMedGoogle Scholar
- Lewis RJ, Tsai FTF, Wigley DB. Molecular mechanism of drug inhibition by DNA gyrase. Bioessays. 1996;18:661–71. DOIPubMedGoogle Scholar
- Takiff HE, Salazar L, Guerrero C, Philipp W, Huang WM, Kreisworth B, Cloning and nucleotide sequencing of Mycobacterium tuberculosis gyrA and gyrB genes and detection of quinolone resistant mutations. Antimicrob Agents Chemother. 1994;38:773–80.PubMedGoogle Scholar
- Rees RJ, Maxwell A. DNA gyrase. Structure and function. Crit Rev Biochem Mol Biol. 1991;26:335–75. DOIPubMedGoogle Scholar
- Revel V, Cambau E, Jarlier E, Sougakoff W. Characterization of mutations in Mycobacterium smegmatis involved in resistance to fluoroquinolones. Antimicrob Agents Chemother. 1994;38:1991–6.PubMedGoogle Scholar
- Inderlied CB. Antimycobacterial agents: in vitro susceptibility testing, spectrums of activity, mechanisms of action and resistance, and assays for activity in biological fluids. In: Lorain V, editor. Antibiotics in laboratory medicine. Baltimore: Williams and Wilkins, Baltimore; 1991. p. 134-197.
- Benveinste R, Davies J. Mechanism of antibiotic resistance in bacteria. Annu Rev Biochem. 1973;42:471–506. DOIPubMedGoogle Scholar
- Davies J, Wright JD. Bacterial resistance to aminoglycoside antibiotics. Trends Microbiol. 1997;5:234–9. DOIPubMedGoogle Scholar
- Douglass J, Steyn LM. A ribosomal gene mutation in streptomycin-resistant Mycobacterium tuberculosis isolates. J Infect Dis. 1993;167:1505–6.PubMedGoogle Scholar
- Finken M, Kirschner P, Meier A, Wrede A, Bottger EC. Molecular basis of streptomycin-resistance in Mycobacterium tuberculosis: alteration of the ribosomal protein S12 gene and point mutations within a functional 16S rRNA pseudoknot. Mol Microbiol. 1993;9:1239–46. DOIPubMedGoogle Scholar
- Meier A, Kirschner P, Bange FC, Vogel U, Botger EC. Genetic alteration in streptomycin-resistance in Mycobacterium tuberculosis: mapping of mutations conferring resistance. Antimicrob Agents Chemother. 1994;38:228–33.PubMedGoogle Scholar
- Nair J, Rouse DA, Bai GH, Morris SL. The rpsL gene and streptomycin resistance in single and multi-drug resistant strains of Mycobacterium tuberculosis. Mol Microbiol. 1993;10:521–4. DOIPubMedGoogle Scholar
- Honore N, Cole ST. Streptomycin resistance in myco-bacteria. Antimicrob Agents Chemother. 1994;38:238–42.PubMedGoogle Scholar
- Woes CR, Gutell RR. Evidence for several higher order structural elements in ribosomal rRNA. Proc Natl Acad Sci U S A. 1989;86:3119–22. DOIPubMedGoogle Scholar
- Shaila MS, Gopinathan RP, Ramakrishnan T. Protein synthesis Mycobacterium tuberculosis H37Rv and the effect of streptomycin in streptomycin susceptible and resistant strains. Antimicrob Agents Chemother. 1973;4:205–13.PubMedGoogle Scholar
- Meier A, Sander P, Schaper KJ, Scholz M, Bottger EC. Correlation of molecular resistance mechanisms and phenotypic resistance levels in streptomycin-resistant Mycobacterium tuberculosis. Antimicrob Agents Chemother. 1996;40:2452–4.PubMedGoogle Scholar
- Orita M, Suzuki Y, Sekiya T, Hayashi K. Rapid and sensitive detection of point mutations and DNA polymorphisms using the polymerase chain reaction. Genomics. 1989;5:875–9. DOIGoogle Scholar
Page created: December 14, 2010
Page updated: December 14, 2010
Page reviewed: December 14, 2010
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.