Volume 10, Number 11—November 2004
THEME ISSUE
ICEID & ICWID 2004
International Conference on Women and Infectious Diseases (ICWID)
Nurses’ Working Conditions: Implications for Infectious Disease
Cite This Article
Citation for Media
Abstract
Staffing patterns and nurses’ working conditions are risk factors for healthcare-associated infections as well as occupational injuries and infections. Staffing shortages, especially of nurses, have been identified as one of the major factors expected to constrain hospitals’ ability to deal with future outbreaks of emerging infections. These problems are compounded by a global nursing shortage. Understanding and improving nurses’ working conditions can potentially decrease the incidence of many infectious diseases. Relevant research is reviewed, and policy options are discussed.
The Institute of Medicine’s report, To Err is Human, which spotlighted the problem of patient safety, reported that tens of thousands of Americans die each year as a result of human error in the delivery of health care (1). Authors of a more recent Institute of Medicine report, Keeping Patients Safe, Transforming the Work Environment of Nurses, concluded that nursing is inseparably linked to patient safety and emphasized that poor working conditions for nurses and inadequate nurse staffing levels increase the risk for errors (2). Nurse working conditions are related to patients’ risk of healthcare-associated infections and occupational injuries and infections among staff (3). We discuss the nurse workforce, review research examining nursing as it relates to infectious disease, identify gaps in the literature, and discuss potential policy options. Although our focus is on the nursing workforce in the United States, international trends and comparisons are also discussed.
Nearly 3 million registered nurses (RNs) work in the United States. Ninety-five percent of these nurses are women, as are most of the 700,000 licensed practical nurses and >2 million unlicensed nurse assistants. Internationally, occupational distributions are similar.
More than 1 million RNs work in hospitals, which makes nursing the largest hospital workforce. In 60% of U.S. hospitals, vacancy rates for RNs have increased since 1999; 14% of hospitals now report a severe nurse shortage (i.e., >20% of positions vacant). The American Hospital Association has reported that hospitals have up to 168,000 vacant positions; 126,000 (75%) of the available positions in these hospitals are for RNs (4). The current nursing shortage is related to an aging workforce, problems with retaining licensed personnel, and difficulty recruiting young people into the nursing workforce. The demand for RNs is projected to grow by 22% by 2008, and unless market corrections are made, the nursing shortage may reach 800,000 vacant positions by 2020 (5). Recent reports document that the nursing shortage is a severe and growing global problem (4).
Historically, the turnover rate among nurses is more than double that for other professionals of comparable education and sex (6). Recent estimates in U.S. hospitals of RN turnover and intention to quit have ranged from 17% to 36% (6,7), figures that compare to an overall turnover rate of 2.2% for those employed in health services and social services and 1.2% for those employed in educational services. In an investigation of the effects of various nurse working conditions in intensive care units, researchers found >17% of RNs indicated their intentions to quit within 1 year (P.W. Stone, unpub. data). This finding was disconcerting because this national U.S. sample of 2,324 RNs was highly qualified; their average experience in health care was 15.6 years (SD = 9.20), and their average tenure in their current position was 8.0 years (SD = 7.50). Of those intending to leave, 72% expressed poor working conditions as the reason. In an American Hospital Association–sponsored study, researchers estimated the cost of replacing one RN to be $30,000–$64,000 (4).
To cover patient census fluctuations and unplanned absences and to fill vacant positions caused by this nursing shortage, many healthcare facilities have increased nurses’ patient loads or expanded the use of nonpermanent staff, such as float pool and agency nurses (4). Concerns have been voiced that reliance on agency nursing services elevates hospital costs, increases the fragmentation of health care, and discourages longer term proactive solutions to staffing shortages that would improve the morale of the permanent staff as well as the quality of patient care services (8). Extended work shifts and overtime for nurses have also escalated; however, nurses report making more errors when working shifts >12 hours, working overtime, or working >40 hours per week (9).
To increase the overall supply of nurses, many countries are increasingly relying on international recruitment and migration (10). The percentage of foreign-trained nurses in the United States is 4%, compared to 8% in the United Kingdom and 23% in New Zealand (11). However, the actual number of foreign-trained nurses in the United States is 90,000, which compares to 42,000 in the United Kingdom (12). In 2002, for the first time more foreign-trained nurses (n = 16,155) were newly registered in Britain than were those who had been educated within the country (n = 14,538). Many concerns exist about clinical competencies, cultural sensitivity, and ethics of the practice of importing nurses (13). While international recruitment can be a solution in one country, it can create additional shortages in others.
A recent evidence-based practice report sponsored by the Agency for Healthcare Quality and Research concluded that a relationship exists between lower levels of nurse staffing and higher incidence of adverse patient outcomes (14). Nurses’ working conditions have been associated with medication errors and falls, increased deaths, and spread of infection (15–30) (Table). RN staffing levels have been associated with the spread of disease during outbreaks (17,22,23,25,28). However, increasing nurse-to-patient ratios alone is not adequate; more complex staffing issues appear to be at work. Many studies have found that the times of higher ratios of “pool staff” (i.e., nursing staff who were members of the hospital pool service or agency nurses) to “regular staff” (i.e., nurses permanently assigned to the unit) were independently associated with healthcare-associated infections (16,17,21,27). The skill mix of the staff, that is, the ratio of RNs to total nursing personnel (RNs plus nurses’ aides), is also related to healthcare-associated infections; increased RN skill mix decreases the incidence of healthcare-associated infections (20,29,30). In a recent comprehensive review of the literature, the authors concluded that evidence of the relationship between nurses’ working environment and patient safety outcomes, including healthcare-associated infections is growing. They also concluded that stability, skill mix, and experience of the nurse workforce in specific settings are emerging as important factors in that relationship (31).
All healthcare workers face a wide range of hazards on the job, including blood and body fluid exposure as well as musculoskeletal injuries related to ergonomic hazards from lifting and repetitive tasks; nursing personnel often experience these hazards most frequently (32). In 2001, U.S. hospitals reported 293,600 nonfatal occupational injuries and illnesses among their personnel. Among the eight private U.S. industries with >100,000 injuries and illnesses annually, the number of cases of nonfatal injury or illness in hospitals is the second highest; and the incidence rate of injuries and illnesses per 100 fulltime workers employed in nursing and personal care facilities is 13.5; by contrast, the national average is 1.8. In 2001, nursing aides and orderlies reported the highest number of occupational injuries that resulted in days away from work of any service industry (70,300); RNs had the second highest number (24,400) (33).
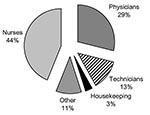
Work-acquired infectious diseases are among the risks all healthcare workers face; and bloodborne pathogens figure prominently among these. Occupational exposure to blood and body fluids is well documented among healthcare workers. Annual exposure prevalence rates range from <10% to 44%, depending on the occupational subgroup (34). Every year, approximately 600,000–800,000 occupational needlestick injuries occur in the United States (34). In a study of 60 U.S. hospitals in a 4-year period, nurses were the most likely to experience a blood or body fluid exposure (Figure) (34). Most exposures involve percutaneous injuries (e.g., needlesticks), although mucocutaneous (e.g., spray or splashes to the eyes or mouth) and direct contact of infected blood with nonintact skin are also routes of exposure. These potential infections, like healthcare-associated infections, also appear to be tied to nurses’ working conditions. In a cross-sectional study of >1,500 nurses employed on 40 units in 20 hospitals, poor organizational climate and high workloads were associated with 50% to 200% increases in the likelihood of needlestick injuries and near-misses among hospital nurses (3).
Emerging infectious diseases and outbreaks of recognized contagious illnesses have highlighted other concerns about the safety of healthcare workers. For example, much of the worldwide severe acute respiratory syndrome (SARS) outbreak was hospital-based, and healthcare workers made up a large proportion of cases, accounting for 37% to 63% of suspected SARS patients in highly affected countries (35). In many countries, nurses were the largest single group affected by SARS (36). During the Toronto outbreak, patient care activities commonly conducted by critical care nurses, such as manipulating oxygen masks and suctioning infected patients, were significantly associated with SARS infection (37). In the event of an influenza pandemic, healthcare workers would be susceptible. During an outbreak of parainfluenza in a intermediate care nursery, 16 (25%) of 65 staff members reported symptoms of respiratory illness (38). These threats to safety of the nurse and other essential healthcare workers are of concern for many reasons.
First, a trained, qualified healthcare workforce is necessary to respond and care for the public in the event of an outbreak. Staffing issues and hospital organization problems are believed to have complicated the containment of the SARS crisis in Toronto. Staffing shortages, especially of nurses, have been identified as one of the major factors expected to constrain hospitals’ ability to deal with possible future threats (4). Without adequate numbers of trained hospital employees to implement effective infection control procedures, such as hand hygiene and proper isolation procedures, emergency departments and hospital wards can easily become the venues where the spread of epidemics occurs.
Second, the perception of unsafe working conditions both for the patient and the worker may actually hinder recruitment and retention of qualified staff. In a American Nurses Association survey of RNs (N = 7,353), 88% of respondents reported health and safety concerns related to work, 75% felt the quality of nursing care had declined in their work setting in the past 2 years, and 92% of those respondents related these concerns to inadequate staffing. Furthermore, >70% of respondents indicated concerns about the acute and chronic effects of work stress and overwork, concerns about a disabling back injury (60%), and fear of contracting HIV or hepatitis from a needlestick injury (45%). Nurses reported that these health and safety concerns influence their decision to continue working in the field of nursing and the kind of nursing work they choose to perform. Because of these concerns, nearly 55% of the nurses surveyed would not recommend the nursing profession as a career for their children or friends. Although the results of this survey may not be generalizable to all nursing personnel because of the nonprobability sampling method and inclusion of only RNs, the results suggest that concern over safety may be contributing to hospital personnel shortages and hindering recruitment efforts. Dissatisfaction, burnout, and concerns about quality of care are reportedly common among hospital nurses in five other industrialized countries (39).
Barring unprecedented growth in the nursing workforce or unforeseen new forces in health care that intervene to reduce burden of care in society, the numbers of nurses will not keep pace with the demand for services. In the coming decades, we face the prospect of fewer professionals and more unlicensed workers in the healthcare workforce. Decisions will have to be made about how hospitals will safely adapt to this situation. At this time, little evidence exists on what constitutes a safe and efficient labor force mix. Therefore, the general impact of nurse working conditions needs to be examined. First, longitudinal studies that track change in infection rates and other untoward incidents over time, under different working conditions, and with different staffing models are essential. Second, researchers need to study how the actual care received by patients varies under different staffing conditions at the bedside so that a better understanding of the impact of work environments at the point of care can be gained. Finally, since costs of care increase when patients have adverse outcomes (40) and nurses’ working conditions affect outcomes, better working conditions could arguably save the healthcare system money. However, the cost-benefit ratio is not known and economic analyses, which include costs related to training, recruitment, and retention, need to be conducted.
Policy solutions for nurse staffing fall into two general categories: 1) incentives and funding for various parties to increase the supply of nurses and 2) employer and hospital regulatory approaches. Although scholarships, loan forgiveness schemes, and funding of new nursing school student slots may be helpful, these policies are unlikely to overcome the long-standing, complex nature of the difficulties in recruiting sufficient newcomers to the nursing profession and then retaining a qualified workforce.
In the United States, regulatory approaches by the states have included prohibiting mandatory overtime for nurses (nine states with regulations), holding hospitals accountable for developing and implementing valid staffing plans (seven states), and setting minimum staffing ratios (one state). Regulating minimum nurse-patient ratios has received much attention, despite critiques from the hospital industry that insufficient data exist to credibly set minimum safe staffing levels. California was the first state to implement hospitalwide minimum nurse-patient ratios. The effects of this regulation need to be carefully examined. Although nursing services are positively correlated with patient outcomes, controversy exists over what constitutes an optimal staffing ratio, and little empirical evidence is available on which to base these decisions.
Staffing levels for bedside nurses are not the only critical resource involved in decreasing risks for healthcare-associated infections, occupational injuries, and infections. Also important is determining the critical mass of infection control and occupational health professionals needed for surveillance, identification of departures from sound practices, and ongoing education of healthcare workers. Policies aimed at ensuring the availability of training programs on all aspects of patient and worker safety are needed, as is the availability of appropriate supplies to prevent unnecessary infections among patients and nurses.
Nursing is a predominately female occupation in which the working conditions are often poor. Such conditions contribute to recruitment and retention problems. Together with demographic changes, the result is a shortage of qualified nurses. Mounting evidence demonstrates that the lack of an adequate supply of qualified nurses is a global public safety issue that may require a multipronged policy approach. Monitoring and improving the working conditions of nurses are likely to improve the quality of health care by decreasing the incidence of many infectious diseases, assisting in retaining qualified nurses, and encouraging men and women to enter the profession. Further research is needed to understand how best to protect the patient as well as the healthcare worker. Changes in the workforce will have implications for infectious disease, infection control, and occupational health professionals with a need for much more thorough training of nonprofessionals in critical practices.
Dr. Stone is an assistant professor at Columbia University School of Nursing. Her research interests include the assessment of cost and quality outcomes related to nursing care delivery.
References
- Institute of Medicine. To err is human: building a safer health system. Washington: National Academy Press; 2000.
- Institute of Medicine. Keeping patients safe: transforming the work environment of nurses (prepublication copy). Washington: National Academies Press; 2004. p. 435.
- Clarke SP, Sloane DM, Aiken LH. Effects of hospital staffing and organizational climate on needlestick injuries to nurses. Am J Public Health. 2002;92:1115–9. DOIPubMedGoogle Scholar
- First Consulting Group. Health care workforce shortage and its implications for American hospitals. Washington: The Group; 2001.
- Health Resources and Services Administration, Bureau of Health Professions. Projected supply, demand, and shortages of registered nurses: 2000–2020. Washington: The Administration; 2002.
- Steel R. Turnover theory at the empirical interface: problems of fit and function. Acad Manage Rev. 2002;27:346–60. DOIGoogle Scholar
- Jones CB. Staff nurse turnover costs: Part II, Measurements and results. J Nurs Adm. 1990;20:27–32.PubMedGoogle Scholar
- Manias E, Aitken R, Peerson A, Parker J, Wong K. Agency nursing work in acute care settings: perceptions of hospital nursing managers and agency nurse providers. J Clin Nurs. 2003;12:457–66. DOIPubMedGoogle Scholar
- Rogers A, Hwang W, Scott L, Aiken L, Dinges D. The working hours of hospital staff nurses and patient safety. Health Aff (Millwood). 2004;23:202–12. DOIPubMedGoogle Scholar
- Aiken LH, Buchan J, Sochalski J, Nichols B, Powell M. Trends in international nurse migration. Health Aff (Millwood). 2004;23:69–77. DOIPubMedGoogle Scholar
- Organisation for Economic Co-operation and Development. International migration of physicians and nurses: causes, consequences and health policy implications. Paris: The Organisation; 2002.
- Sprately E, Johnson A, Sochalski J, Fritz M, Spencer W. The registered nurse population march 2000. Washington: U.S. Department of Health and Human Services, Bureau of Health Professions, Division of Nursing; 2001.
- Stilwell B, Diallo K, Zurn P, Dal Poz M, Adams O, Buchan J. Developing evidence-based ethical policies on the migration of health workers: conceptual and practical challenges. Hum Resour Health. 2003;1:8. DOIPubMedGoogle Scholar
- Hickman D, Severance S, Feldstein A. The effect of health care working conditions on patient safety. Rep.74. Rockville (MD): Agency for Healthcare Research and Quality; 2003.
- Kovner C, Jones C, Zhan C, Gergen PJ, Basu J. Nurse staffing and postsurgical adverse events: an analysis of administrative data from a sample of U.S. hospitals, 1990–1996. Health Serv Res. 2002;37:611–29. DOIPubMedGoogle Scholar
- Alonso-Echanove J, Edwards JR, Richards MJ, Brennan P, Venezia RA, Keen J, Effect of nurse staffing and antimicrobial-impregnated central venous catheters on the risk for bloodstream infections in intensive care units. Infect Control Hosp Epidemiol. 2003;24:916–25. DOIPubMedGoogle Scholar
- Andersen BM, Lindemann R, Bergh R, Nesheim B, Syversen G, Solheim N, Spread of methicillin-resistant Staphylococcus aureus in a neonatal intensive unit associated with understaffing, overcrowding and mixing of patients. J Hosp Infect. 2002;50:18–24. DOIPubMedGoogle Scholar
- Stegenga J, Bell E, Matlow A. The role of nurse understaffing in nosocomial viral gastrointestinal infections on a general pediatrics ward. Infect Control Hosp Epidemiol. 2002;23:133–6. DOIPubMedGoogle Scholar
- Amaravadi RK, Jacobson BC, Solomon DH, Fischer MA. ICU nurse-to-patient ratio is associated with complications and resource use after esophagectomy. Intensive Care Med. 2000;26:1857–62. DOIPubMedGoogle Scholar
- Lichtig LK, Knauf RA, Risen-McCoy R, Wozniak L. Nurse staffing and patient outcomes in the inpatient hospital setting. Washington: American Nurses Association; 2000.
- Robert J, Fridkin SK, Blumberg HM, Anderson B, White N, Ray SM, The influence of the composition of the nursing staff on primary bloodstream infection rates in a surgical intensive care unit. Infect Control Hosp Epidemiol. 2000;21:12–7. DOIPubMedGoogle Scholar
- Harbarth S, Sudre P, Dharan S, Cadenas M, Pittet D. Outbreak of Enterobacter cloacae related to understaffing, overcrowding, and poor hygiene practices. Infect Control Hosp Epidemiol. 1999;20:598–603. DOIPubMedGoogle Scholar
- Vicca AF. Nursing staff workload as a determinant of methicillin-resistant Staphylococcus aureus spread in an adult intensive therapy unit. J Hosp Infect. 1999;43:109–13. DOIPubMedGoogle Scholar
- Kovner C, Gergen PJ. Nurse staffing levels and adverse events following surgery in U.S. hospitals. Image J Nurs Sch. 1998;30:315–21. DOIPubMedGoogle Scholar
- Fridkin SK, Peear SM, Williamson TH, Galgiani JN, Jarvis WR. The role of understaffing in central venous catheter-associated bloodstream infections. Infect Control Hosp Epidemiol. 1996;17:150–8. DOIPubMedGoogle Scholar
- Haley RW, Cushion NB, Tenover FC, Bannerman TL, Dryer D, Ross S, Eradication of endemic methicillin-resistant Staphylococcus aureus infections from a neonatal intensive care unit. J Infect Dis. 1995;171:614–24. DOIPubMedGoogle Scholar
- Arnow P, Allyn PA, Nichols EM, Hill DL, Pezzlo M, Bartlett RH. Control of methicillin-resistant Staphylococcus aureus in a burn unit: role of nurse staffing. J Trauma. 1982;22:954–9. DOIPubMedGoogle Scholar
- Archibald LK, Manning ML, Bell LM, Banerjee S, Jarvis WR. Patient density, nurse-to-patient ratio and nosocomial infection risk in a pediatric cardiac intensive care unit. Pediatr Infect Dis J. 1997;16:1045–8. DOIPubMedGoogle Scholar
- Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346:1715–22. DOIPubMedGoogle Scholar
- Knauf RA, Lichtig LK, Risen-McCoy R, Singer AD, Wozniak L. Implementing nursing’s report card: a study of RN staffing, length of stay and patient outcomes. Washington: American Nurses Association;1997.
- Jackson M, Chairello L, Gaynes RP, Gerberding JL. Nurse staffing and health care-associated infections: proceedings from a working group meeting. Am J Infect Control. 2002;30:199–206. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Worker health chartbook, 2000. Cincinnati (OH): US Department of Health and Human Services, Public Health Service; 2000.
- U.S. Bureau of Labor Statistics. Lost-worktime injuries and illnesses: characteristics and resulting days away from work. Washington: The Bureau; 2003.
- Occupational outlook handbook, 2002–2003 edition. Washington: U.S. Department of Labor, Bureau of Labor Statistics; 1999.
- Varia M, Wilson S, Sarwal S, McGeer A, Gournis E, Galanis E, Investigation of a nosocomial outbreak of severe acute respiratory syndrome (SARS) in Toronto, Canada. CMAJ. 2003;169:285–92.PubMedGoogle Scholar
- Booth CM, Boone RH, Tomlison G, Detsky AS. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289:2801–9. DOIPubMedGoogle Scholar
- Loeb M, McGeer A, Henry B, Ofner M, Rose D, Hylwka T. SARS among critical care nurses, Toronto. Emerg Infect Dis. 2004;10:251–5.PubMedGoogle Scholar
- Moisiuk SE, Robson D, Klass LK, Kliewer G, Wasyliuk W, Davi M, Outbreak of parainfluenza virus type 3 in an intermediate care neonatal nursery. Pediatr Infect Dis J. 1998;17:49–53. DOIPubMedGoogle Scholar
- Aiken LH, Clarke SP, Sloane DM. Hospital staffing, organization, and quality of care: Cross-national findings. Nurs Outlook. 2002;50:187–94. DOIPubMedGoogle Scholar
- Zhan C, Miller MR. Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290:1868–74. DOIPubMedGoogle Scholar
Figure
Table
Cite This ArticleTable of Contents – Volume 10, Number 11—November 2004
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Patricia W. Stone, Columbia University, School of Nursing, 617 W. 168th Street, New York, NY 10032, USA; fax: 212-305-6937
Top