Volume 10, Number 6—June 2004
Research
Antimicrobial Resistance among Campylobacter Strains, United States, 1997–2001
Cite This Article
Citation for Media
Abstract
We summarize antimicrobial resistance surveillance data in human and chicken isolates of Campylobacter. Isolates were from a sentinel county study from 1989 through 1990 and from nine state health departments participating in National Antimicrobial Resistance Monitoring System for enteric bacteria (NARMS) from 1997 through 2001. None of the 297 C. jejuni or C. coli isolates tested from 1989 through 1990 was ciprofloxacin-resistant. From 1997 through 2001, a total of 1,553 human Campylobacter isolates were characterized: 1,471 (95%) were C. jejuni, 63 (4%) were C. coli, and 19 (1%) were other Campylobacter species. The prevalence of ciprofloxacin-resistant Campylobacter was 13% (28 of 217) in 1997 and 19% (75 of 384) in 2001; erythromycin resistance was 2% (4 of 217) in 1997 and 2% (8 of 384) in 2001. Ciprofloxacin-resistant Campylobacter was isolated from 10% of 180 chicken products purchased from grocery stores in three states in 1999. Ciprofloxacin resistance has emerged among Campylobacter since 1990 and has increased in prevalence since 1997.
Campylobacter is the most common cause of bacterial gastroenteritis in the United States, causing an estimated 2.4 million human infections annually (1). Diagnosed infections have declined in recent years. In 2001, FoodNet surveillance identified 13.4 diagnosed Campylobacter infections per 100,000 persons (2). Approximately 95% of diagnosed Campylobacter infections are due to C. jejuni (3). Although most Campylobacter infections cause an acute, self-limited illness characterized by diarrhea, fever, and abdominal cramps, severe infections do occur (4). Antimicrobial treatment can shorten the duration of illness and may be life-saving in invasive infections (5–7). Fluoroquinolones (e.g., ciprofloxacin) are often prescribed empirically for the treatment of gastroenteritis and for Campylobacter infections in adults (6,8). Quinolones (e.g., nalidixic acid), although now seldom used for treatment in the United States, are frequently used to screen for fluoroquinolone resistance because of the close correlation between quinolone and fluoroquinolone resistance among Campylobacter. Macrolides, such as erythromycin, are also prescribed to treat Campylobacter infections (4,9).
Fluoroquinolone-resistant Campylobacter infections in humans were first detected in Europe in the late 1980s (10–12). Subsequently, an increasing proportion of Campylobacter isolates around the world have been found to be fluoroquinolone-resistant (13). Studies in the United States, Europe, and New Zealand have identified poultry as a principal source of Campylobacter infection (14–16). Quinolones have been available in human medicine since the mid-1960s, and the first fluoroquinolone (ciprofloxacin) was approved for use in humans in 1986. Two fluoroquinolones, sarafloxacin and enrofloxacin, were approved for use in poultry by the U.S. Food and Drug Administration (FDA) in 1995 and 1996, respectively (17). These fluoroquinolones were the first ones approved in food animals; subsequently, other fluoroquinolones have been approved for veterinary use but not for use in poultry (18).
To investigate the epidemiology of fluoroquinolone-resistant Campylobacter in the United States, we reviewed national surveillance data to determine the prevalence of antimicrobial resistance, particularly ciprofloxacin resistance, among Campylobacter isolates; conducted a case-control study to determine the proportion of ciprofloxacin-resistant infections that were domestically acquired; and performed a retail survey to determine the prevalence of ciprofloxacin-resistant Campylobacter contaminating chicken products sold in selected supermarkets.
National Surveillance for Resistance in Campylobacter
1989–1990 Sentinel County Study
From 1989 to 1990, a national county-based survey of antimicrobial susceptibility among Campylobacter isolates was conducted. Sentinel clinical laboratories in 19 counties participated. The methods of this survey are described elsewhere (19,20). Briefly, the first five sporadic Campylobacter isolates identified each month were forwarded to the Centers for Disease Control and Prevention (CDC). Patients with Campylobacter infection were interviewed with a standard questionnaire, which included information about clinical illness and exposures (i.e., food, animal, and foreign travel) during the 2 weeks before illness onset. Isolates were determined to be Campylobacter by dark-field microscopic examination and hippurate hydrolysis (20–22). Hippurate-positive isolates were considered C. jejuni. All isolates with questionnaires received during the first 4 months of the study underwent susceptibility testing. Because of a shortage of reagents, a random sample of 50% of isolates with completed questionnaires received during the last 8 months of the study was further characterized. Isolates were tested for susceptibility to azithromycin, chloramphenicol, ciprofloxacin, clindamycin, erythromycin, gentamicin, nalidixic acid, and tetracycline by using broth microdilution methods (19). In 2003, a retrospective analysis of the hippurate-negative isolates was completed; these isolates were speciated by using methods described below.
National Antimicrobial Resistance Monitoring System (NARMS), 1997–2001
NARMS for enteric bacteria is a collaboration between CDC, the Food and Drug Administration, and state and local health departments. The system monitors patterns of antimicrobial drug resistance. NARMS methods are described in detail elsewhere (23).
In brief, isolates were tested for viability, confirmed as Campylobacter, and identified to the species level by using the hippurate hydrolysis test according to published methods (21,22). Hippurate-negative Campylobacter in which the hippuricase gene could be detected by polymerase chain reaction (PCR) were identified as C. jejuni (24). Isolates that tested negative for the hippuricase gene but positive for a C. coli-specific ceuE sequence were identified as C. coli (25). Isolates that could not be identified as either C. jejuni or C. coli by these PCR assays were referred to the National Campylobacter Reference Laboratory at CDC for identification with genotypic (e.g., 16S rRNA sequencing) and phenotypic methods (21).
Isolates were tested with the E-test system (AB BIODISK, Solna, Sweden) to determine MICs for six antimicrobial agents: chloramphenicol, ciprofloxacin, clindamycin, erythromycin, nalidixic acid, and tetracycline. Beginning in 1998, azithromycin and gentamicin were also included. When available, National Committee for Clinical Laboratory Standards interpretive criteria for Enterobacteriaceae MICs were used; ciprofloxacin resistance was defined as MIC >4 μg/mL, and erythromycin resistance was defined as MIC >8 μg/mL (26). Multidrug resistance was defined as resistance to two or more of the original six antimicrobial agents.
We used a multivariable logistic regression model to assess changes in the proportion of isolates with antimicrobial drug resistance from 1997 through 2001 because the population under surveillance more than doubled from 1997 to 2001, and substantial site-to-site variation in prevalence of antimicrobial drug resistance was identified (i.e., uncertainty was found in the denominators for calculating rates). The model was for antimicrobial drug resistance as a function of year and included main effects adjustments for age categories and site-to-site variation in prevalence. Within the available data, site by year interaction was not a significant factor but because the catchment areas expanded, the hypothesis of site by year interaction could not be fully tested.
1997 Retrospective Case-Comparison Study
Using NARMS isolates, we conducted a retrospective case-comparison study in four NARMS sites (California, Connecticut, Georgia, and Oregon). Persons with ciprofloxacin-resistant (CipR) Campylobacter infection identified in 1997 were compared with persons in whom the diagnosis of ciprofloxacin-sensitive (CipS) Campylobacter infection was made that same year. We compared up to two CipS cases for each CipR case and matched cases by geographic site and date of stool specimen collection. All case-patients were interviewed by telephone, usually within 8 weeks of their illness onset, about demographics, clinical information, and exposures (e.g., antimicrobial drug use in the 4 weeks before illness onset, foreign travel, and consumption of poultry and raw milk in the 7 days before illness onset) with a standardized questionnaire.
1999 Retail Survey
Three NARMS-participating state health departments (Georgia, Maryland, and Minnesota) participated in a survey of retail chicken products. From January to June 1999, each site purchased a convenience sample of 10 whole broiler chickens per month from supermarkets located within the state. State public health laboratories at each site tested the samples for Campylobacter. Carcass rinse samples were centrifuged, and pellets were incubated in enrichment broth and plated onto Campylobacter blood agar plates according to methods published elsewhere (27); neither media contained quinolone or macrolide antimicrobial agents. Campylobacter isolates were forwarded to CDC for species identification and antimicrobial susceptibility testing according to NARMS methods.
National Surveillance
1989–1990 Sentinel County Study
Two hundred ninety-eight patients were interviewed, and their Campylobacter isolates were tested. Of these isolates, 289 (97%) were C. jejuni, 8 (3%) were C. coli, and 1 (0.3%) was a C. lari. None were resistant to ciprofloxacin, and 3 (1%) of 294 were resistant to nalidixic acid (MIC > 32 μg/mL); 1 isolate was C. lari, which is inherently resistant to nalidixic acid (28), and 2 were C. jejuni. The C. lari isolate was resistant to ofloxacin (MIC = 8 μg/mL), intermediately resistant to norfloxacin (MIC = 8 μg/mL) but susceptible to ciprofloxacin (MIC = 2 μg/mL).1 The two nalidixic acid-resistant C. jejuni isolates were susceptible to ciprofloxacin (MIC = 0.5 μg/mL) and norfloxacin and ofloxacin (MIC < 2 μg/mL). The proportion of the isolates resistant to tetracycline was 42% (124/295). The resistant proportion for the other antimicrobial agents tested were as follows: erythromycin 3% (8/295), clindamycin 2% (6/295), azithromycin 2% (5/294), chloramphenicol 0% (0/295), and gentamicin 0% (0/295). Travel history was available for 296 patients with Campylobacter infection; 23 (8%) patients traveled outside of the United States in the week before illness onset. Of the persons with available information, 32 (11%) of 295 had taken an antimicrobial agent in the 30 days before illness onset, 46 (15%) of 298 were hospitalized, and 241 (81%) of 297 were treated with an antimicrobial agent for their illness. Among the 234 persons for whom treatment data were available, the most common agents used for treatment were erythromycin (62%), ciprofloxacin (19%), and trimethoprim-sulfamethoxazole (5%). Of the three patients with nalidixic acid-resistant infections, none traveled outside the United States, and none were treated with a quinolone or fluoroquinolone in the month before illness.
NARMS, 1997–2001
From 1997 to 2001, a total of 1,932 presumptive Campylobacter isolates were received at CDC through NARMS; 193 (10%) were excluded because they were not viable, 104 (5%) were not in accordance with the one-a-week sampling method, 39 (2%) were determined not to be Campylobacter, 22 (1%) were duplicates, and 21 (1%) were contaminated cultures. Of the 1,553 (80%) isolates further characterized and included in this analysis, 1,471 (95%) were C. jejuni, 63 (4%) were C. coli, 7 (0.4%) were C. upsaliensis, 5 (0.3%) were C. fetus, 2 (0.1%) were C. lari, and 5 (0.3%) were undetermined (i.e., determination by 16S study did not identify a species). Forty-five percent of case-patients were female; the median age was 33 years (range <1–96). Among 1,439 isolates with known source of specimen collection, 1,426 (99%) were from stool samples, and 13 (1%) were from blood samples. Among blood isolates, eight were C. jejuni, two were C. fetus, two were C. upsaliensis, and one was C. lari.
The results of susceptibility testing among Campylobacter isolates by species are shown in Table 1. Resistance to ciprofloxacin among all Campylobacter isolates was 13% in 1997 and 19% in 2001. Resistance to erythromycin among all Campylobacter isolates was 2% in 1997 and 2% in 2001. The results of antimicrobial susceptibility testing by year for isolates of the most common species, C. jejuni, are shown in Table 2
The prevalence of ciprofloxacin-resistant Campylobacter ranged from 0% (0/14) in Tennessee in 1999 to 27% (27/52) in Georgia in 2001. By using a multivariate logistic regression model and controlling for age and site-to-site variation in prevalence, the proportion of all Campylobacter isolates resistant to ciprofloxacin and nalidixic acid in 2001 was significantly higher than the proportion of isolates resistant to ciprofloxacin in 1997 (data only shown for ciprofloxacin in Table 3). The remaining antimicrobial drugs had no statistically significant change in resistance over time (data not shown).
Fifty-one percent of Campylobacter isolates were resistant to >1 drug, 18% were resistant to >2 drugs, and 10% were resistant to >3 drugs. The most common multidrug resistance (i.e., >2 drugs) pattern included ciprofloxacin, nalidixic acid, and tetracycline.
1997 Retrospective Case-Comparison Study
Sixteen (57%) of 28 ciprofloxacin-resistant Campylobacter (CipR) case-patients and 31 ciprofloxacin-sensitive (CipS) case-patients were interviewed. The median age was 46 years (range 9–76 years) for CipR patients and 24 years (range 1–87 years) for CipS patients (Wilcoxon rank-sum, p = 0.08). CipR patients did not differ significantly from CipS patients in terms of sex (40% vs. 42% female, p = 0.1), race (87% vs. 77% white, p = 0.08), and place of residence (87% vs. 61% urban/suburban areas, p = 0.06). Five (31%) CipR patients were hospitalized for gastroenteritis compared with 1 (3%) CipS patient (matched odds ratio [mOR] = 13.6, 95% confidence interval [CI] 1.4 to 130.1). Eight (57%) CipR case-patients reported having bloody diarrhea compared with eight (30%) CipS patients (mOR = 3.2, 95% CI 0.8 to 12.1). Seven (44%) of 16 CipR patients compared with 1 (3%) of 31 CipS patients traveled to a foreign country in the 7 days before illness onset (mOR = 23.3, 95% CI 2.5 to 215.6); 5 (71%) of 7 CipR patients traveled to Europe while 1 CipS patient traveled to the Caribbean. Among all case-patients, 35 of 47 reported treatment with an antimicrobial agent for their illness. Of those who recalled the name of the antimicrobial drug, 75% reported taking a fluoroquinolone, 16% reported taking a macrolide, and 8% took trimethoprim-sulfamethoxazole (TMP/SMX). One CipR patient and one CipS patient took fluoroquinolones between onset of illness and collection of stool specimens. Among the eight CipR patients who did not travel and did not take fluoroquinolones between illness onset and stool specimen collection, seven (87%) consumed poultry in the 7 days before infection; this finding was not statistically different from that in CipS patients. No other exposures were significantly associated with ciprofloxacin-resistant infection, including having pets, drinking raw milk, or being exposed to a farm (data not shown).
1999 Retail Survey
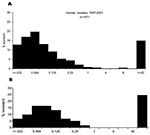
Among the 180 retail chicken products purchased, representing 18 domestic brand names from 22 grocery stores, Campylobacter was isolated from 80 (44%) samples. Sixty-two (77%) were C. jejuni, 16 (20%) were C. coli, and 2 (2%) were undetermined (i.e., determination by 16S study did not identify a species). The prevalence of Campylobacter isolated was 33% (20 of 60) in Georgia, 37% (22 of 60) in Maryland, and 63% (38 of 60) in Minnesota. This difference among sites was in part due to the difference in isolation rates of C. coli; 14 (87%) of the 16 C. coli isolates came from retail chickens purchased in Minnesota. A ciprofloxacin-resistant strain of Campylobacter was identified in 10% of the 180 retail chicken products tested, and an erythromycin-resistant strain was identified in 2% of chicken products (Table 4). The distribution of ciprofloxacin MICs in Campylobacter species of retail chicken and human isolates was similar. For both human and poultry Campylobacter isolates, MICs were predominantly <0.5 or >32 μg/mL with few intermediate phenotypes (Figure 1).
Fluoroquinolone-resistant Campylobacter have emerged over the last decade in the United States. In 1990, no ciprofloxacin-resistant human isolates were identified in a national sentinel county-based survey. From 1997 to 2001, the prevalence of ciprofloxacin-resistant Campylobacter increased significantly from 13% to 19%. These data are consistent with four prior surveillance studies from humans conducted in the United States: 1) a hospital-based study in Pennsylvania conducted from 1982 to 1991 found no fluoroquinolone resistance among C. jejuni isolates (29), 2) a second study at the same Pennsylvania hospital found a sharp increase in ciprofloxacin resistance among C. jejuni from 8% in 1996 to 40% in 2001 (30), 3) a study conducted in Wisconsin between 1992 and 1995 found 12% of the C. jejuni to be ciprofloxacin-resistant (31), and 4) a study in Minnesota showed an increase in quinolone-resistant C. jejuni isolates from 1.3% in 1992 to 10.2% in 1998 (Figure 2) (18). The emergence of fluoroquinolone resistance among Campylobacter isolates in the 1990s has occurred while resistance to other antimicrobial agents has remained stable. Specifically, resistance to the macrolides, azithromycin and erythromycin, which are commonly used antimicrobial agents in humans (32), has remained low (1%–3%).
Our retrospective case-comparison study showed that patients with ciprofloxacin-resistant C. jejuni infections were more likely to be hospitalized compared to patients with ciprofloxacin-susceptible infections. These results, however, are based on a small number of patients, and age could have been a confounder. Other studies have found that patients infected with fluoroquinolone-resistant Campylobacter have a longer duration of diarrhea than patients with fluoroquinolone-susceptible isolates, although no difference in hospitalization rates have been reported (18,33). These findings may have clinical implications. Ciprofloxacin is commonly used to treatment severe Campylobacter infections and other intestinal infections in adults, so the rise of fluoroquinolone resistance may result in ineffective treatment when fluoroquinolones are used. Macrolides, which are efficacious in treating Campylobacter (5,34), should still be considered the first-line drugs for severe Campylobacter infections, as resistance to this class remains low.
Our study also identified foreign travel, particularly to Europe, to be associated with ciprofloxacin-resistant C. jejuni infection. High rates of fluoroquinolone-resistant Campylobacter have been reported from southern Europe and other regions of the world (13). Studies in northern Europe have associated fluoroquinolone use in food animals, particularly poultry, as a source for human infection with fluoroquinolone-resistant Campylobacter (13). Nevertheless, while foreign travel was a risk factor in our study, over half of the ciprofloxacin-resistant infections were domestically acquired. Ciprofloxacin resistance was not associated with use of fluoroquinolones before specimen collection, which suggests that fluoroquinolone-resistant organisms did not result from individual use of fluoroquinolones. A more recent, larger case-control study of patients infected with ciprofloxacin-resistant Campylobacter infections found similar results to our study; 58% of illnesses were domestically acquired, and none of the patients took fluoroquinolones after illness onset and before specimen collection (35).
Our 1999 survey of retail chicken sold in selected supermarkets provided ecologic evidence that chicken may be a source of domestically acquired ciprofloxacin-resistant Campylobacter infections; 10% of retail chickens were contaminated with ciprofloxacin-resistant Campylobacter. Other studies have shown that Campylobacter, including ciprofloxacin-resistant Campylobacter, are commonly isolated from retail poultry meats. A survey of retail meats purchased in the Washington, D.C., area isolated Campylobacter species from 71% of chicken and 14% of turkeys tested (36); 25% of the C. jejuni isolates and 40% of the C. coli isolates were resistant to ciprofloxacin (37). A second survey in Minnesota isolated Campylobacter from 88% of retail chicken meats purchased in 1997, including C. jejuni in 74% and C. coli in 21%. Ciprofloxacin-resistant Campylobacter was identified in 20% of retail chicken products (18). In this study, comparison of molecular subtypes from human and retail chicken quinolone-resistant C. jejuni isolates found that six of seven subtypes were indistinguishable from each other.
In the United States, the FDA has approved the use of fluoroquinolones at different times for humans and food animals. Fluoroquinolones have been commonly used in humans for treating intestinal and other infections since 1986 (32). The first fluoroquinolones to be FDA-approved for use in food animals in the United States were sarafloxacin in 1995 and enrofloxacin in 1996. These fluoroquinolones were approved for use in chickens and turkeys to treat bacterial respiratory infections principally caused by E. coli. These agents are typically administered to the entire poultry house (often >20,000 birds) through drinking water, which results in the treatment of sick and healthy birds with various concentrations of fluoroquinolones. The extent of fluoroquinolone use in chickens and turkeys in the United States is not known; manufacturers and farmers are not required to report these data. The Animal Health Institute has estimated that 1%–2% of the approximately 8 billion broiler chickens slaughtered each year in the United States are treated with fluoroquinolones (38). An experiment with Campylobacter–infected chickens treated with enrofloxacin and sarafloxacin showed that ciprofloxacin resistance rapidly developed among Campylobacter (39).
An association between the approval of fluoroquinolones for use in food-producing animals and the development of fluoroquinolone-resistant Campylobacter in animals and humans has been noted in several countries. The approval of fluoroquinolones for use in food animals has been followed temporally by a rise in ciprofloxacin-resistant Campylobacter and other enteric pathogens isolated from animals and humans in Denmark, the Netherlands, and Spain (13,40). After the use of oral fluoroquinolones in pigs was discontinued in Denmark in 1999, nalidixic acid resistance among C. coli isolates from pigs decreased from 17% in 1998 to 5% in 2001 (41). In the United States, FDA has recently conducted a quantitative risk assessment and concluded that fluoroquinolone use in chickens and turkeys results each year in >10,000 human infections with fluoroquinolone-resistant Campylobacter in persons who seek medical care and are treated with fluoroquinolones (42). FDA proposed the withdrawal of approval of fluoroquinolones for use in poultry in October 2000 (43). This is the first time a proposal has been made to withdraw an approval for an antimicrobial used in agriculture because of associated emergence of resistance in humans. The manufacturer of sarafloxacin has since withdrawn this product from the market, but the manufacturer of enrofloxacin continues to market enrofloxacin for use in poultry in the United States.
Our studies had several limitations. The retrospective case-comparison study did not assess exposures among travelers and therefore cannot assess the possibility that the travelers may have acquired ciprofloxacin-resistant Campylobacter from eating poultry or other foods while traveling. Routine surveillance for antimicrobial susceptibility among Campylobacter did not start until 1997, and therefore we cannot identify national trends in antimicrobial resistance from 1991 to 1996. Other limitations are evident in NARMS Campylobacter surveillance, including the use of sentinel clinical laboratories in some states and some variation in the isolation procedures. However, these limitations are not likely to be associated with an increased (or decreased) likelihood of selecting antimicrobial-resistant isolates for submission to NARMS since the antimicrobial resistance pattern of the isolates were not known when the isolates were selected. Lastly, because NARMS Campylobacter surveillance was not nationwide and resistance may differ regionally, generalization to the U.S. population should be done with caution.
In summary, we describe the emergence over the last decade of fluoroquinolone-resistant Campylobacter infections in the United States. As of 1997, more than half of such ifnections were domestically acquired. In 1999, fluoroquinolone-resistant Campylobacter organisms were present on a substantial fraction of chickens sold at supermarkets in three widely separated locations in the United States. Continuing national surveillance of human infections and prospective national monitoring of the frequency of contamination of poultry at retail would provide useful ongoing information. Clinicians should include macrolides, such as azithromycin, as a first-line treatment of severe Campylobacter infections.
Dr. Gupta is a former EIS fellow of the Foodborne and Diarrheal Diseases Branch, National Center for Infectious Diseases, Centers for Disease Control and Prevention, and is now on the faculty at Johns Hopkins University, Division of Infectious Diseases. Her research interests include diarrheal diseases and more recently HIV and coexisting conditions in India and other resource-poor settings.
Acknowledgments
We thank Allen Ries, Felecia Hardnett, Robert Hoekstra, Jocelyn Rocourt, and Charlotte Sumner for their assistance with this manuscript.
Funds for this study come from the Emerging Infections Program, Centers for Disease Control and Prevention, the U.S. Food and Drug Administration, and from state funds to support public health surveillance activities.
References
- Mead PS, Slutsker L, Dietz V, McCaig LF, Bresee JS, Shapiro C, Food-related illness and death in the United States. Emerg Infect Dis. 1999;5:607–25. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Preliminary FoodNet data on the incidence of foodborne illnesses—selected sites, United States, 2002. MMWR Morb Mortal Wkly Rep. 2003;52:340–3.PubMedGoogle Scholar
- Altekruse SF, Stern NJ, Fields PI, Swerdlow DL. Campylobacter jejuni—an emerging foodborne pathogen. Emerg Infect Dis. 1999;5:28–35. DOIPubMedGoogle Scholar
- Allos BM. Campylobacter jejuni infections: update on emerging issues and trends. Clin Infect Dis. 2001;32:1201–6. DOIPubMedGoogle Scholar
- Salazar-Lindo E, Sack RB, Chea-Woo E, Kay BA, Piscoya ZA, Leon-Barua R, Early treatment with erythromycin of Campylobacter jejuni–associated dysentery in children. J Pediatr. 1986;109:355–60. DOIPubMedGoogle Scholar
- Goodman LJ, Trenholme GM, Kaplan RL, Segreti J, Hines D, Petrak R, Empiric antimicrobial therapy of domestically acquired acute diarrhea in urban adults. Arch Intern Med. 1990;150:541–6. DOIPubMedGoogle Scholar
- Mattila L, Peltola H, Siitonen A, Kyronseppa H, Simula I, Kataja M. Short-term treatment of traveler’s diarrhea with norfloxacin: a double- blind, placebo-controlled study during two seasons. Clin Infect Dis. 1993;17:779–82.PubMedGoogle Scholar
- Dryden MS, Gabb RJ, Wright SK. Empirical treatment of severe acute community-acquired gastroenteritis with ciprofloxacin. Clin Infect Dis. 1996;22:1019–25.PubMedGoogle Scholar
- Endtz HP, Mouton RP, van der Reyden T, Ruijs GJ, Biever M, van Klingeren B. Fluoroquinolone resistance in Campylobacter spp isolated from human stools and poultry products. [see comments]. Lancet. 1990;335:787. DOIPubMedGoogle Scholar
- Gaunt PN, Piddock LJ. Ciprofloxacin resistant Campylobacter spp. in humans: an epidemiological and laboratory study. J Antimicrob Chemother. 1996;37:747–57. DOIPubMedGoogle Scholar
- Prats G, Mirelis B, Llovet T, Munoz C, Miro E, Navarro F. Antibiotic resistance trends in enteropathogenic bacteria isolated in 1985–1987 and 1995–1998 in Barcelona. Antimicrob Agents Chemother. 2000;44:1140–5. DOIPubMedGoogle Scholar
- Engberg J, Aarestrup FM, Taylor DE, Gerner-Smidt P, Nachamkin I. Quinolone and macrolide resistance in Campylobacter jejuni and C. coli: resistance mechanisms and trends in human isolates. Emerg Infect Dis. 2001;7:24–34. DOIPubMedGoogle Scholar
- Harris NV, Thompson D, Martin DC, Nolan CM. A survey of Campylobacter and other bacterial contaminants of pre-market chicken and retail poultry and meats, King County, Washington. Am J Public Health. 1986;76:401–6. DOIPubMedGoogle Scholar
- Adak GK, Cowden JM, Nicholas S, Evans HS. The Public Health Laboratory Service national case-control study of primary indigenous sporadic cases of Campylobacter infection. Epidemiol Infect. 1995;115:15–22. DOIPubMedGoogle Scholar
- Eberhart-Phillips J, Walker N, Garrett N, Bell D, Sinclair D, Rainger W, Campylobacteriosis in New Zealand: results of a case-control study. J Epidemiol Community Health. 1997;51:686–91. DOIPubMedGoogle Scholar
- U.S. Food and Drug Administration. Enrofloxacin for poultry; opportunity for Hearing. [cited 2002 Nov 18]. Available from: http://www.fda.gov/OHRMS/DOCKETS/98fr/103100a.htm. DHHS; 2000
- Smith KE, Besser JM, Hedberg CW, Leano FT, Bender JB, Wicklund JH, Quinolone-resistant Campylobacter jejuni infections in Minnesota, 1992–1998. N Engl J Med. 1999;340:1525–32. DOIPubMedGoogle Scholar
- Tenover FC, Baker CN, Fennell CL, Ryan CA. Antimicrobial resistance in Campylobacter species. In: Nachamkin I, Blaser MJ, Tompkins LS, editors. Campylobacter jejuni current status and future trends. Washington: American Society of Microbiology; 1992. p. 66–73.
- Patton CM, Nicholson MA, Ostroff SM, Ries AA, Wachsmuth IK, Tauxe RV. Common somatic O and heat-labile serotypes among Campylobacter strains from sporadic infections in the United States. J Clin Microbiol. 1993;31:1525–30.PubMedGoogle Scholar
- Barrett TJ, Patton CM, Morris GK. Differentiation of Campylobacter species using phenotypic characterization. Lab Med. 1988;19:96–102.
- Murray PR. Manual of clinical microbiology. In: Microbiology. 7th ed. Washington: ASM Press; 1999. p. 1773.
- Centers for Disease Control and Prevention. National Antimicrobial Resistance Monitoring System Annual Report 2001. Atlanta: Department of Health and Human Services. [cited 2003 Nov]. Available from: http://www.cdc.gov/narms/annual/2001/annual_01.htm
- Linton D, Lawson AJ, Owen RJ, Stanley J. PCR detection, identification to species level, and fingerprinting of Campylobacter jejuni and Campylobacter coli direct from diarrheic samples. J Clin Microbiol. 1997;35:2568–72.PubMedGoogle Scholar
- Gonzalez I, Grant KA, Richardson PT, Park SF, Collins MD. Specific identification of the enteropathogens Campylobacter jejuni and Campylobacter coli by using a PCR test based on the ceuE gene encoding a putative virulence determinant. J Clin Microbiol. 1997;35:759–63.PubMedGoogle Scholar
- National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing: eighth informational supplement. Wayne (PA): The Committee; 1998.
- Hunt JM. Campylobacter. In: Food and Drug Administration bacteriological analytical manual. 7th ed. Arlington (VA): AOAC International; 1992. p. 77–91.
- Lastovica A, Skirrow M. Clinical significance of Campylobacter and related species other than Campylobacter jejuni and C. coli. In: Blaser M, editor. Campylobacter. Washington: American Society for Microbiology; 2000. p. 89–120.
- Nachamkin I, Ung H, Li M. Increasing fluoroquinolone resistance in Campylobacter jejuni, Pennsylvania, USA, 1982–2001. Emerg Infect Dis. 2002;8:1501–3. Nachamkin I. Antimicrobial susceptibility of Campylobacter jejuni and Campylobacter coli to ciprofloxacin, erythromycin and tetracycline from 1982 to 1992. Med Microbiol Lett. 1994;3:300–5.
- Kiehlbauch J, Simon M, Makowski J. Use of filtration to isolate Campylobacter and related organisms from stools. In: Newell DG, editor. Campylobacters, Helicobacters, and related organisms. New York: Plenum Press; 1996. p. 47–9.
- McCaig LF, Besser RE, Hughes JM. Antimicrobial drug prescription in ambulatory care settings, United States, 1992–2000. Emerg Infect Dis. 2003;9:432–7.PubMedGoogle Scholar
- Marano NVD, Fiorentino T, Segler S, Carter M, Kassenborg H, Smith K, Fluoroquinolone-resistant Campylobacter causes longer duration of diarrhea than fluoroquinolone-susceptible Campylobacter strains in FoodNet sites. 2nd International Conference on Emerging Infectious Diseases. Atlanta, GA, 2000.
- Kuschner RA, Trofa AF, Thomas RJ, Hoge CW, Pitarangsi C, Amato S, Use of azithromycin for the treatment of Campylobacter enteritis in travelers to Thailand, an area where ciprofloxacin resistance is prevalent. Clin Infect Dis. 1995;21:536–41.PubMedGoogle Scholar
- Kassenbourg H, Smith K, Vugia D, Rabatsky-Ehr T, Bates M, Dumas N, Fluoroquinolone-resistant infections: eating poultry outside the home and foreign travel are risk factors. Clin Infect Dis. 2004. In press. DOIGoogle Scholar
- Zhao C, Ge B, De Villena J, Sudler R, Yeh E, Zhao S, Prevalence of Campylobacter spp., Escherichia coli, and Salmonella serovars in retail chicken, turkey, pork, and beef from the greater Washington, D.C. area. Appl Environ Microbiol. 2001;67:5431–6. DOIPubMedGoogle Scholar
- Ge B, White DG, McDermott PF, Girard W, Zhao S, Hubert S, Antimicrobial-resistant Campylobacter species from retail raw meats. Appl Environ Microbiol. 2003;69:3005–7. DOIPubMedGoogle Scholar
- Animal Health Institute. Antimicrobial volume survey. [cited 2002 Dec 12]. Available from: www.ahi.org
- McDermott PF, Bodeis SM, English LL, White DG, Walker RD, Zhao S, Ciprofloxacin resistance in Campylobacter jejuni evolves rapidly in chickens treated with fluoroquinolones. J Infect Dis. 2002;185:837–40. DOIPubMedGoogle Scholar
- Endtz HP, Ruijs GJ, van Klingeren B, Jansen WH, van der Reyden T, Mouton RP. Quinolone resistance in Campylobacter isolated from man and poultry following the introduction of fluoroquinolones in veterinary medicine. J Antimicrob Chemother. 1991;27:199–208. DOIPubMedGoogle Scholar
- Bager F, Emborg H, Heuer O. DANMAP 2001—Use of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from food animals, foods and humans in Denmark. Vol. 2002. Copenhagen: Statens Serum Institut; 2001.
- U.S. Food and Drug Administration. The human health impact of fluoroquinolone-resistant Campylobacter attributed to the consumption of chicken. [cited 2002 15 Jun]. Available from: http://www.fda.gov/cvm/antimicrobial/revisedRA.pdf
- Baker CN. The E-test and Campylobacter jejuni. Diagn Microbiol Infect Dis. 1992;15:469–72. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleTable of Contents – Volume 10, Number 6—June 2004
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Amita Gupta, Johns Hopkins University, Division of Infectious Diseases, 1830 East Monument Street, Room 450E, Baltimore, MD 21287, USA; fax: 410-614-8488
Top