Volume 13, Number 1—January 2007
Research
Prevalence of G2P[4] and G12P[6] Rotavirus, Bangladesh
Cite This Article
Citation for Media
Abstract
Approximately 20,000 stool specimens from patients with diarrhea visiting an urban and a rural hospital in Bangladesh during January 2001–May 2006 were tested for group A rotavirus antigen, and 4,712 (24.0%) were positive. G and P genotyping was performed on a subset of 10% of the positive samples (n = 471). During the 2001–2005 rotavirus seasons, G1P[8] (36.4%) and G9P[8] (27.7%) were the dominant strains, but G2[4] and G12P[6] were present in 15.4% and 3.1% of the rotavirus-positive patients, respectively. During the 2005–06 rotavirus season, G2P[4] (43.2%) appeared as the most prevalent strain, and G12P[6] became a more prevalent strain (11.1%) during this season. Because recently licensed rotavirus vaccines are specific for only P[8], these vaccines may not perform well in settings where non-P[8] types are prevalent.
Group A rotaviruses are the major etiologic agents of severe infantile diarrhea. Worldwide, >125 million infants and young children develop rotavirus-associated diarrhea each year, resulting in 440,000 infant and child deaths, mostly in developing countries (1). In Bangladesh, rotaviruses cause 6,000–14,000 deaths each year in children <5 years of age (2).
The tremendous incidence of rotavirus disease underscores the urgent need for interventions such as vaccines, particularly to prevent childhood deaths in developing nations. Fortunately, 2 rotavirus vaccines, RotaTeq (Merck and Co., Whitehouse Station, NJ, USA) and RotaRix (GlaxoSmithKline, Research Triangle Park, NC, USA) passed a large safety trial, showed high efficacy against the major rotavirus G types, and have been approved by the Food and Drug Administration (3,4). The efficacy trials of these vaccines have been conducted in the United States, Latin America, and Europe but not in developing countries in Africa and Asia.
Rotavirus infection shows a characteristic seasonal pattern that is not clearly understood. In developed countries with temperate climates, peak incidence is in winter; however, in developing countries with tropical or subtropical climates, the virus circulates year-round (5–8). The temperature in Bangladesh is usually high from April through October and relatively low from December through February. In addition, previous studies have indicated that rotavirus in Bangladesh is affected by floods, which increase opportunities for transmission of the virus (8,9). Bangladesh lies on the confluence of hundreds of rivers and is inundated with water every year due to enhanced rainfall during the monsoon season, starting in June (10).
Rotaviruses belong to the genus Reoviridae and consist of 11 segments of double-stranded RNA. Two outer capsid proteins, VP7 (defining G genotypes) and VP4 (defining P genotypes), independently elicit neutralizing responses. Based on these proteins, a dual classification system of group A rotaviruses has been introduced (5). Rotaviruses can be serotyped by using neutralization assays with panels of antisera and genotyped by type-specific primer-dependent reverse transcription–PCR (RT-PCR) and nucleotide sequence analysis (11–13). So far, >15 G and 26 P genotypes have been described in humans and a variety of animals (6,14,15). The major human G types are G1, G2, G3, G4, and G9, which, combined with the P types P[8], P[4], and P[6], account for >80% of rotavirus-associated gastroenteritis episodes worldwide (16,17).
Rotaviruses show great genomic diversity, and several studies in different regions of Bangladesh have identified types not targeted by candidate rotavirus vaccines (18–21). Unicomb et al. (8) showed that frequent genomic reassortment among different rotavirus types was accelerated by mixed infection and generated huge genomic diversity. Although the importance of type-specific immunologic protection against rotavirus disease is still under discussion, many investigators suggest that genomic characterization of rotaviruses is needed to assess whether vaccine efficacy might be altered by the changing pattern in the distribution of different G and P genotypes (17,22,23).
In our study, stool samples from gastroenteritis patients admitted to 2 hospitals, 1 urban and 1 rural, within the hospital surveillance system of International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B), from January 2001 through May 2006 were tested for the rotavirus VP6 antigen. The study objective was to clarify the genomic diversity of rotavirus in urban and rural areas in Bangladesh, with a goal of providing information for rotavirus vaccine development programs.
Study Population
The ICDDR,B Centre for Health and Population Research runs an urban hospital situated in Dhaka, the capital city of Bangladesh, which has a population of ≈10 million, and a rural hospital at Matlab, 45 km southeast of Dhaka, which has ≈300,000 inhabitants. Each year, >100,000 patients are treated for diarrhea at the Dhaka hospital and ≈15,000 at the Matlab hospital. At the Dhaka hospital, diarrhea surveillance is conducted in a systematic manner; stool samples are collected to determine the presence of enteric pathogens in every 50th (2%) patient attending the hospital for treatment of diarrhea. In Matlab, hospital stool samples are collected from all patients from the community, which is under active rotavirus surveillance.
Rotavirus Antigen Detection
As part of the surveillance system, rotavirus antigens (group A rotavirus-specific VP6 proteins) were detected in the stool specimens using a solid-phase sandwich-type enzyme immunoassay modeled after the Dakopatts commercial kit (Dakopatts, Copenhagen, Denmark), incorporating rabbit hyperimmune antisera produced at ICDDR,B and an anti-human rotavirus–horseradish peroxidase conjugate. The same criteria as those used by the Dakopatts kit were used for determination of positivity (8).
RNA Extraction
Rotavirus RNA was extracted from the stool samples. The QIAamp Viral RNA mini kit (Qiagen/Westburg, Leusden, the Netherlands) was used according to the manufacturer’s instructions
RT-PCR
[[AA:T1:PREVIEWHTML]]A multiplex RT-PCR was performed by using the Qiagen OneStep RT-PCR Kit (Qiagen/Westburg) for rotavirus G and P genotypes using type-specific oligonucleotide primers as previously described (Table 1) (11,13,24). The reaction was carried out with an initial reverse-transcription step at 45°C for 30 min, followed by 35 cycles of amplification (30 sec at 94°C, 30 sec at 48°C, 1 min at 72°C), and a final extension of 7 min at 72°C in a thermal cycler (Eppendorf, Hamburg, Germany). PCR products were subjected to electrophoresis on a 2% agarose gel, stained with ethidium bromide, and observed under ultraviolet light. Specific segment sizes for different G and P genotypes were observed on the stained gel.
Nucleotide Sequencing
The PCR products were purified with the QIAquick PCR purification kit (Qiagen/Westburg) and sequenced by using the dideoxy-nucleotide chain termination method with the ABI PRISM BigDye Terminator Cycle Sequencing Reaction kit (Applied Biosystems, Foster City, CA, USA) on an automated sequencer. The consensus forward primer Beg9 and reverse primer End9 were used to amplify and sequence the VP7 gene. For the VP4 gene, the forward primer Con3 and reverse primer Con2 were used as described previously (15).
Data Analysis and DNA Sequence Submission
Data were analyzed by SPSS for Windows, release 11.5.1 (SPSS Inc., Chicago, IL, USA). The nucleotide sequence data of the rotavirus strains were submitted to the GenBank under the accession nos. DQ482712, DQ482718, DQ482725, DQ146652, DQ146653, DQ146654, DQ146658, DQ146663, DQ146664, DQ146665, DQ146669, EF033338, EF033339, and EF033340.
Detection of Rotavirus Antigen
[[AA:T2:PREVIEWHTML]]From January 2001 through May 2006, 19,039 stool specimens were tested for group A rotavirus VP6 antigen; 4,644 (24.4%) samples had positive results. Table 2 shows the distribution of rotavirus-positive patients in the hospital surveillance systems in Dhaka and Matlab. The average detection rate of rotavirus was 25.2% in Dhaka and 23.3% in Matlab.
Quality Control
Stool specimens obtained from 311 patients with diarrhea were tested for the presence of rotavirus particles using the IDEIA rotavirus kit (DAKO Ltd., Cambridgeshire, UK). By using the IDEIA kit, 234 samples were found to be positive and 77 negative. By comparison, our in-house ELISA kit could detect rotavirus antigen in 232 of the IDEIA-positive samples. Among the IDEIA-negative samples, 72 were negative for rotavirus antigen by our in-house kit. Thus, a comparison of the results indicated that our in-house ELISA kit had an overall sensitivity of 99.1% and specificity of 96.1% compared with the IDEIA rotavirus kit.
Age of the Rotavirus-positive Patients
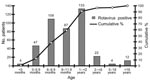
The age range of the rotavirus diarrhea patients (2001–2005) was 1 month–63.2 years, median age 10 months, and mean age 22.8 months. Most of the rotavirus-positive patients (91%) were <2 years of age (Figure 1). Infection rates were lowest in patients <3 months and >5 years of age.
Seasonal Pattern of Rotavirus Infection
Figure 2 shows the monthly distribution of rotavirus diarrhea in Dhaka and Matlab. Rotaviruses were detected throughout the year in both settings, even though 2 clear seasonal rotavirus peaks were observed each year: a sharp winter peak in January and February, and a monsoon peak in July and August. Taking the average for each setting into account, our model suggests that the rotavirus season in Bangladesh usually starts in June and ends in May (year-round).
Air temperature records for Dhaka and water level data for the Buriganga River (Sadarghat point, Dhaka) for the 5 years of the study (2001–2005) were obtained from the Institute of Water Modelling, Dhaka, Bangladesh (www.iwmbd.org). These data and the number of rotavirus patients admitted to the Dhaka hospital by month are shown in Figure 3. The temperature was lowest from December through February each year, which coincided with the increased number of rotavirus diarrhea cases. On the other hand, the monsoon peaks of rotavirus diarrhea were correlated with the water level. The water level reached the highest mark during July–August each year, which corresponded to the increase of the proportion of rotavirus diarrhea. The meteorologic data from Matlab also correlated to the increased incidence of rotavirus infection, as was seen for Dhaka (data not shown).
Distribution of G and P Types
[[AA:T3:PREVIEWHTML]]G and P genotyping were carried out on 471 rotavirus antigen–positive stool samples (10% of all rotavirus-positive patients) by using a type-specific primer–based multiplex RT-PCR that could detect 6 G genotypes (G1, G2, G3, G4, G8, G9) and 5 P genotypes (P[8], P[4], P[6], P[9], P[11]). The untypeable and suspicious samples with lower amounts of PCR products were successfully typed and confirmed by using nucleotide sequencing. Table 3 shows the distribution of G and P types of rotavirus strains detected in Dhaka and Matlab. No significant difference was observed between the distribution of rotavirus strains in Dhaka and Matlab (p>0.05). Overall, the most prevalent genotype was G1P[8] (33.8%), which was followed by G9P[8] (25.3%), G2P[4] (20.2%), and G4P[8] (8.3%). Mixed infections were detected in 3.2% of the samples. Strains with unusual G-P combinations, such as G1P[6], G2P[6], and G2P[8], were also detected.
Unusual porcine-like G11 rotavirus strains were detected in 3 patients (0.6%). These strains were untypeable by multiplex PCR because no G11-specific primer was included in the routine primer set. Therefore, sequencing of the VP7 and VP4 genes was required. The partial VP7 gene sequences of the 3 G11 rotavirus strains (Dhaka22-01, Matlab36-02, and Dhaka13-06) were most similar (>98% similarities at the nucleotide and >97% at the amino acid level) to the porcine-like G11 strain Dhaka6 (15). On the other hand, the VP4 genes were most similar to human P[8] or P[6] strains (Malawi strain OP351, Thai strain 15vp4w, and US strain Se585).
Uncommon human G12 rotavirus strains (5.6%), were also detected during our study period. Because the G12 strains were untypeable by using our routine primers, nucleotide sequencing of their VP7 genes was required. All the VP7 gene sequences of the Bangladeshi G12 strains were most similar to the recently isolated G12 strains (Indian strain ISO-2) but distantly related to the prototype G12 strain L26 isolated in the Philippines. The gene segments encoding the VP4, VP6, and NSP4 proteins were sequenced for Bangladeshi G12 strains Dhaka25-02 (G12P[8]) and Dhaka12-03 (G12P[6]). The VP4 gene sequence of strain Dhaka25-02 was most similar to the human P[8] rotavirus strain DRC88 (98% similarity at the amino acid level) isolated in Democratic Republic of the Congo, and strain Dhaka12-03 was most similar to the human P[6] strain US1205 (99% similarity at the amino acid level) isolated in the United States. The VP6 and NSP4 sequences of both strains were also most similar to human rotavirus strains (Indian rotavirus strains RMC100, G25795, and V13520).
Polyacrylamide gel electrophoresis was performed for the 26 G12 strains isolated in our study, and 18 showed a clear RNA migration pattern. Long electropherotypes were detected in 15 (83.3%) samples, which included both G12P[8] and G12P[6] strains. Short electropherotypes were detected in only 3 (16.7%) samples, which also included both G12P[8] and G12P[6] strains.
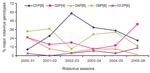
Fluctuation of the G and P Types Distribution over Time
Large fluctuations of the rotavirus genotype distribution were observed both in Dhaka and Matlab. However, no significant difference was observed between the urban and rural setting with regard to the yearly distribution of genotypes (p>0.05). The overall distribution of the major genotypes over time is shown in Figure 4. The G1P[8] strains were less common in 2001, became the most predominant strains in the following years, but decreased again in 2005–06. G9P[8] strains dominated in the first 2 rotavirus seasons, decreased sharply during 2002–03, dominated again for the next 2 years, and decreased again during 2005–06. G4P[8], which had been the most prevalent strain in the 1990s in Bangladesh, was found to be less common in our study and constituted only 1.2% during 2005–06. Most interestingly, the strain G2P[4] was the most predominant (43.2%) during the 2005–06 rotavirus season, although it was less common during the previous seasons (15.4% 2001–05). The uncommon strains G12P[6] and G12P[8], introduced in Bangladesh for the first time during the 2000–01 season, became more prevalent (13.6%) in this region by the 2005–06 season.
Rotavirus was found in approximately one fourth of all patients with diarrhea who were treated at ICDDR,B hospitals; most rotavirus cases (92.5%) occurred in children during their first 2 years of life. A recent report indicated that 33% of children <5 years age admitted to the ICDDR,B from 1993 through 2004 were rotavirus positive (2). Reports from other Asian countries also indicated that rotaviruses were present in 20%–58% of patients with diarrhea who were <5 years of age. Thus, the rotavirus detection rate from our study is comparable to rates from some other Asian countries, including India, South Korea, and Hong Kong (20%–30%), but much lower than those reported in Taiwan, Thailand, China, Japan, Mayanmar, and Vietnam (43%–58%) (25–34).
Although rotavirus-associated diarrhea was documented year-round in Dhaka and Matlab, a sharp winter peak and a monsoon peak were observed each year. The winter rotavirus peak is usually observed worldwide, but the monsoon peak is not common in settings with temperate climates. We analyzed environmental data including rainfall and water level of the nearest river and found that the monsoon rotavirus peaks in Bangladesh could be defined by high water levels due to heavy rainfall, which normally starts in the second week of June (35). Because of the heavy rainfall, the water level of the rivers begins to increase and reaches its highest level during July–August each year, resulting in inundation of the surrounding areas and increasing the chance of fecal contamination of water. Ahmed and colleagues reported that the number of rotavirus diarrhea cases increased remarkably, and mixed rotavirus types were frequently isolated during the floods in 1988 in Dhaka (10). In July and August 2004 in Matlab (Figure 2), a large increase in rotavirus-associated diarrhea was observed. Analysis of the water level of the nearest river (Chandpur point of the Meghna River, data not shown) showed that this increase correlated directly with an increased water level. The water level reached the 5.42 meter mark in July 2004, the highest in that region during our study period.
Our main goal was to characterize the VP7 (G genotype) and VP4 (P genotype) gene segments of the rotavirus strains. We identified most of the globally common rotavirus types (G1, G2, G4, and G9) in our study. Surprisingly, no G3 strain has been detected in Bangladesh since 1993, even though G3 is one of the most prevalent rotavirus types worldwide (8,25,29). Results of rotavirus diversity from this study were compared with previous findings in Bangladesh (8), and we observed that the distribution of rotavirus genotypes was changing over time. From 1992 through 1997, the most common rotavirus genotype was G4 (47% of the typeable rotavirus strains), but this genotype’s prevalence gradually decreased, and it became a less common rotavirus strain over time (1.2% in 2005–06). The distribution of G2 strains, on the other hand, remained nearly unchanged through rotavirus season 2004–05 (19.5% in 1992–1997 and 16.2% in 2001–2005). However, G2 suddenly became the most prevalent genotype in 2005–06 (43.2%).
Three G11 strains, commonly found in pigs, were isolated from humans in the present study. In Bangladesh, pigs are uncommon farm animals, and no genotyping studies on pigs or other animals have been conducted. Therefore, the identification of the strains with an animal-like G11 VP7 specificity and a human P[8] or P[6] specificity raises the question whether these strains are reassortants of human and animal rotavirus strains. This finding underscores the need to include animal rotavirus strains rotavirus surveillance programs. At the same time, water samples, particularly those collected during floods, can be evaluated for the presence of unusual rotavirus strains that might have been introduced from domestic animals.
For the first time in Bangladesh, a very uncommon human rotavirus strain, G12, was detected. The strain was first detected in 1987–1988 in the Philippines, and since then, it has been emerging all over the world (36–40). G12 is reported as an important rotavirus strain in India (17.1% in 2003–2005) and in Argentina (6% in 1999–2003) (17,36). A considerable proportion of G12 was also documented during our study period and reached 13.6% in the latest rotavirus season (2005–06). Thus, the emergence of G12 strains has led to the need for prospective surveillance using new diagnostic RT-PCR primers for G12 strains.
Genetic analysis of the VP4, VP6, and NSP4 gene segments showed that the Bangladeshi G12 strains contained typical human rotavirus gene segments distantly related to the prototype G12 strains L26 and T152. It is possible that the VP7 gene segments from the prototype G12 strains were reassorted with the typical human rotavirus strains. More genetic analyses of complete genome sequences would be helpful to investigate the possible reassortment events and evolution of the recently emerging G12 strains.
P genotype analysis showed that the rotavirus strains with the P[8] specificity made up 76.4% of the circulating strains during 2001–2005; non-P[8] strains constituted 21.9%. The most interesting finding about P types in our study was that the non-P[8] strains represented more than half of the strains (56.8%) during the rotavirus season 2005–06. The currently licensed rotavirus vaccines have shown high efficacy rates in trials and have focused on the role of the major G genotypes, but the role of P genotypes has not been addressed clearly (3,4). These vaccines include the P[8] specificity, but it is unknown how the vaccines will perform in settings where the non-P[8] types are prevalent. An efficacy trial of the rotavirus vaccine RotaTeq will begin soon in Bangladesh, so the findings of our study regarding rotavirus strain diversity will be important for evaluating the results of this trial.
Mr Rahman is a PhD student at the University of Leuven, Belgium, and a research officer in the Virology Laboratory, Laboratory Sciences Division, International Centre for Diarrhoeal Disease Research, Bangladesh, Dhaka, Bangladesh. His research interests focus on the molecular characterization and evolution of rotaviruses.
Acknowledgment
This study was funded by World Health Organization (WHO) (Ref. V27-181-176) and Government of Bangladesh/Debt Relief Grant Aid (DRGA) (grant No. GR-00410). International Centre for Diarrhoeal Disease Research, Bangladesh, acknowledges with gratitude the commitment of WHO and DRGA to the Centre’s research efforts. Mr Rahman was supported by Interfaculty Council for Development Co-operation Scholarship of the University of Leuven, Belgium.
References
- Parashar UD, Gibson CJ, Bresse JS, Glass RI. Rotavirus and severe childhood diarrhea.Emerg Infect Dis. 2006;12:304–6.PubMedGoogle Scholar
- International Centre for Diarrhoeal Disease Research. Bangladesh. Centre for Health and Population Research. Estimated deaths due to rotavirus in Bangladesh.Health and Science Bulletin.2006;4:6–10.
- Ruiz-Palacios GM, Perez-Schael I, Velazquez FR, Abate H, Breuer T, Clemens SC, Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis.N Engl J Med. 2006;354:11–22. DOIPubMedGoogle Scholar
- Vesikari T, Matson DO, Dennehy P, van Damme P, Santosham M, Rodrigue Z, Safety and efficacy of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine.N Engl J Med. 2006;354:23–33. DOIPubMedGoogle Scholar
- Estes MK. Rotaviruses and their replication. In: Howley PM, editor. Fields virology, 4th ed., vol 2. Philadelphia: Lippincott Williams & Wilkins; 2001. pp. 1747–86.
- Kapikian AZ, Hoshino Y, Chanock RM. Rotaviruses. In: Howley PM, editor. Fields virology, 4th ed., vol 2. Philadelphia: Lippincott Williams & Wilkins; 2001. pp. 1787–1833.
- Turcios RM, Curns AT, Holman RC, Pandya-Smith I, Lamonte A, Bresee JS, Temporal and geographic trends of rotavirus activity in the United States, 1997–2004.Pediatr Infect Dis J. 2006;25:451–4. DOIPubMedGoogle Scholar
- Unicomb LE, Podder G, Gentsch JR, Woods PA, Hasan KZ, Faruque ASG, Evidence of high-frequency genomic reassortment of group A rotavirus strains in Bangladesh: emergence of type G9 in 1995.J Clin Microbiol. 1999;37:1885–91.PubMedGoogle Scholar
- Ahmed MU, Urasawa S, Taniguchi K, Urasawa T, Kobayashi N, Wakasugi F, Analysis of human rotavirus strains prevailing in Bangladesh in relation to nationwide floods brought by the 1988 monsoon.J Clin Microbiol. 1991;29:2273–9.PubMedGoogle Scholar
- Ali A. Climate change impacts and adaptation assessment in Bangladesh.Clim Res. 1999;12:109–16. DOIGoogle Scholar
- Gentsch JR, Glass RI, Woods P, Gouvea V, Gorziglia M, Flores J, Identification of group A rotavirus gene 4 types by polymerase chain reaction.J Clin Microbiol. 1992;30:1365–73.PubMedGoogle Scholar
- Gorziglia M, Larralde G, Kapikian AZ, Chanock RM. Antigenic relationships among human rotaviruses as determined by outer capsid protein VP4.Proc Natl Acad Sci U S A. 1990;87:7155–9. DOIPubMedGoogle Scholar
- Gouvea V, Glass RI, Woods P, Taniguchi K, Clark HF, Forrester B. Polymerase chain reaction amplification and typing of rotavirus nucleic acid from stool specimens.J Clin Microbiol. 1990;28:276–82.PubMedGoogle Scholar
- Martella V, Ciarlet M, Banyai K, Lorusso E, Cavalli A, Corrente M, Identification of a novel VP4 genotype carried by a serotype G5 porcine rotavirus strain.Virology. 2006;346:301–11. DOIPubMedGoogle Scholar
- Rahman M, Matthijnssens J, Nahar S, Podder G, Sack DA, Azim T, Characterization of a novel P[25],G11 human group a rotavirus.J Clin Microbiol. 2005;43:3208–12. DOIPubMedGoogle Scholar
- Gentsch JR, Laird AR, Bielfelt B, Griffin DD, Banyai K, Ramachandran M, Serotype diversity and reassortment between human and animal rotavirus strains: Implications for rotavirus vaccine programs.J Infect Dis. 2005;192:S146–59. DOIPubMedGoogle Scholar
- Santos N, Hoshino Y. Global distribution of rotavirus serotypes/genotypes and its implication for the development and implementation of an effective rotavirus vaccine.Rev Med Virol. 2005;15:29–56. DOIPubMedGoogle Scholar
- Fun BN, Unicomb LE, Rahim Z, Banu NN, Podder G, Clemens J, Rotavirus-associated diarrhea in rural Bangladesh: two-year study of incidence and serotype distribution.J Clin Microbiol. 1991;29:1359–63.PubMedGoogle Scholar
- Unicomb LE, Bingnan F, Rahim Z, Banu NN, Gomes JG, Podder G, A one-year survey of rotavirus strains from three locations in Bangladesh.Arch Virol. 1993;132:201–8. DOIPubMedGoogle Scholar
- Unicomb LE, Kilgore PE, Faruque ASG, Hamadani JD, Fuchs GJ, Albert MJ, Anticipating rotavirus vaccines: hospital-based surveillance for rotavirus diarrhea and estimates of disease burden in Bangladesh.Pediatr Infect Dis J. 1997;16:947–51. DOIPubMedGoogle Scholar
- Ward RL, McNeal MM, Clemens JD, Sack DA, Rao M, Huda N, Reactivities of serotyping monoclonal antibodies with culture-adapted human rotaviruses.J Clin Microbiol. 1991;29:449–56.PubMedGoogle Scholar
- Bernstein DI, Glass RI, Rodgers G, Davidson BL, Sack DA. Evaluation of rhesus rotavirus monovalent and tetravalent reassortant vaccines in US children.JAMA. 1995;273:1191–6. DOIPubMedGoogle Scholar
- Bresee JS, Hummelman E, Nelson EA, Glass RI. Rotavirus in Asia: the value of surveillance for informing decisions about the introduction of new vaccines.J Infect Dis. 2005;192:S1–5. DOIPubMedGoogle Scholar
- Rahman M, Sultana R, Podder G, Faruque ASG, Matthijnssens J, Zaman K, Typing of human rotaviruses: nucleotide mismatches between VP7 gene and primer are associated with genotyping failure.Virol J. 2005;2:24. DOIPubMedGoogle Scholar
- Bahl R, Ray P, Subodh S, Shambharkar P, Saxena M, Parashar U, Incidence of severe rotavirus diarrhea in New Delhi, India, and G and P types of the infecting rotavirus strains.J Infect Dis. 2005;192:S114–9. DOIPubMedGoogle Scholar
- Chen KT, Chen PY, Tang RB, Huang YF, Lee PI, Yang JY, Sentinel hospital surveillance for rotavirus diarrhea in Taiwan, 2001–2003.J Infect Dis. 2005;192:S44–8. DOIPubMedGoogle Scholar
- Fang ZY, Wang B, Kilgore PE, Bresee JS, Zhang LJ, Sun LW, Sentinel hospital surveillance for rotavirus diarrhea in the People’s Republic of China, August 2001–July 2003.J Infect Dis. 2005;192:S94–9. DOIPubMedGoogle Scholar
- Jiraphongsa C, Bresee JS, Pongsuwanna Y, Kluabwang P, Poonawagul U, Arporntip P, Epidemiology and burden of rotavirus diarrhea in Thailand: results of sentinel surveillance.J Infect Dis. 2005;192:S87–93. DOIPubMedGoogle Scholar
- Kang G, Kelkar SD, Chitambar SD, Ray P, Naik T. Epidemiological profile of rotaviral infection in India: challenges for the 21st century.J Infect Dis. 2005;192:S120–6. DOIPubMedGoogle Scholar
- Kim JS, Kang JO, Cho SC, Jang YT, Min SA, Park TH, Epidemiological profile of rotavirus infection in the Republic of Korea: results from prospective surveillance in the Jeongeub District, 1 July 2002 through 30 June 2004.J Infect Dis. 2005;192:S49–56. DOIPubMedGoogle Scholar
- Moe K, Hummelman EG, Oo WM, Lwin T, Htwe TT. Hospital-based surveillance for rotavirus diarrhea in children in Yangon, Myanmar.J Infect Dis. 2005;192:S111–3. DOIPubMedGoogle Scholar
- Nakagomi T, Nakagomi O, Takahashi Y, Enoki M, Suzuki T, Kilgore PI. Incidence and burden of rotavirus gastroenteritis in Japan, as estimated from a prospective sentinel hospital study.J Infect Dis. 2005;192:S106–10. DOIPubMedGoogle Scholar
- Nelson EA, Tam JS, Yu LM, Ng YC, Bresee JS, Poon KH, Hospital-based study of the economic burden associated with rotavirus diarrhea in Hong Kong.J Infect Dis. 2005;192:S64–70. DOIPubMedGoogle Scholar
- Van Man N, Luan Le T, Trach DD, Thanh NT, Van Tu P, Long NT, Epidemiological profile and burden of rotavirus diarrhea in Vietnam: 5 years of sentinel hospital surveillance, 1998–2003.J Infect Dis. 2005;192:S127–32. DOIPubMedGoogle Scholar
- Singh OP. Cause-effect relationships between sea surface temperature, precipitation and sea level along the Bangladeshi coast.Theor Appl Climatol. 2001;68:233–43. DOIGoogle Scholar
- Samajdar S, Varghese V, Barman P, Ghosh S, Mitra U, Dutta P, Changing pattern of human group A rotaviruses: emergence of G12 as an important pathogen among children in eastern India.J Clin Virol. 2006;36:183–8. DOIPubMedGoogle Scholar
- Das S, Varghese V, Chaudhury S, Barman P, Mahapatra S, Kojima K, Emergence of novel human group A rotavirus G12 strains in India.J Clin Microbiol. 2003;41:2760–2. DOIPubMedGoogle Scholar
- Griffin DD, Nakagomi T, Hoshino Y, Nakagomi O, Kirkwood CD, Parashar UD, Characterization of nontypeable rotavirus strains from the United States: identification of a new rotavirus reassortant (P2A[6],G12) and rare P3[9] strains related to bovine rotaviruses.Virology. 2002;294:256–69. DOIPubMedGoogle Scholar
- Pongsuwanna Y, Guntapong R, Chiwakul M, Tacharoenmuang R, Onvimala N, Wakuda M, Detection of a human rotavirus with G12 and P[9] specificity in Thailand.J Clin Microbiol. 2002;40:1390–4. DOIPubMedGoogle Scholar
- Shinozaki K, Okada M, Nagashima S, Kaiho I, Taniguchi K. Characterization of human rotavirus strains with G12 and P[9] detected in Japan.J Med Virol. 2004;73:612–6. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleTable of Contents – Volume 13, Number 1—January 2007
| EID Search Options |
|---|
|
|
|
|
|
|


Please use the form below to submit correspondence to the authors or contact them at the following address:
Mustafizur Rahman, Virology Laboratory, Laboratory Sciences Division, ICDDR,B, GPO Box-128, Dhaka-1000, Bangladesh;
Top