Volume 13, Number 3—March 2007
Dispatch
Environmental Burkholderia cepacia Complex Isolates from Human Infections
Cite This Article
Citation for Media
Abstract
Members of the Burkholderia cepacia complex (Bcc), found in many environments, are associated with clinical infections. Examining diverse species and strains from different environments with multilocus sequence typing, we identified >20% of 381 clinical isolates as indistinguishable from those in the environment. This finding links the natural environment with the emergence of many Bcc infections.
The Burkholderia cepacia complex (Bcc) is a group of closely related gram-negative bacteria comprising at least 9 species (1). They are routinely isolated from the natural environment, where they can have a range of beneficial properties (2). However, these bacteria can also frequently cause fatal infections in vulnerable humans, such as those who have cystic fibrosis (CF). Because Bcc bacteria are not normally carried as commensal organisms, the main sources of infection are considered to be patient-to-patient spread (3,4); hospital settings, including medical devices and contaminated disinfectants; and the environment (5,6). Therefore, although Bcc species may have an important environmental role in agriculture and biotechnology industries, their use also represents a potential clinical risk to susceptible members of the community (7,8). All species of Bcc can be isolated from the environment in differing degrees (2). Similarly, all current Bcc species have been cultured from CF patient sputum (2). Infection control measures have been implemented to reduce patient-to-patient transmission; although effective, these measures have not prevented the emergence of new infection. Thus, the environment could be acting as a constant nonpatient reservoir for infectious Bcc pathogens.
Previous studies have reported the possibility of humans acquiring Bcc directly from natural environments (9,10). The most recent of these studies reported evidence that a B. cenocepacia strain, isolated from soil, was indistinguishable by several typing methods (pulsed-field gel electrophoresis [PFGE] genomic fingerprinting and repetitive extragenic palindromic [rep]–PCR) from isolates of the problematic CF lineage PHDC (10).
To evaluate how widespread the emergence of environmental isolates as causes of clinical infections may be, we used a highly discriminatory and transportable typing method to study isolates from several large bacterial culture collections. Multilocus sequence typing (MLST) is a relatively new technique based upon unambiguous sequence analysis of several housekeeping genes. Unlike previous methods for Bcc strain typing (10), MLST is not based on banding patterns but instead relies on the robust comparison of DNA sequence information. This process facilitates both the identification and matching of identical clones as well as their evolutionary comparison to closely related strains.
Using a recently validated MLST scheme (11), we analyzed a collection of 381 clinical isolates of all 9 currently reported Bcc species, from 28 countries. A total of 187 distinct sequence types (STs) were identified from clinical isolates within this collection and compared with 233 environmental Bcc isolates (113 STs). We found that 81 clinical isolates (encompassing15 STs) were identical by MLST to a wide range of environmental isolates. This figure represents 21.5% of the clinical isolates examined (for clarity, a subset are shown in the Table; [12]).
The resolution of strain identification offered by MLST is such that different isolates sharing the same ST (genotypically indistinguishable at all 7 loci) are defined as clones of the same strain (e.g., for a group of isolates within this collection, we have further validated this identity by cloning and sequencing up to 10 random fragments of DNA). The 15 STs identified from environmental and clinical sources belonged to 6 different Bcc species (Table): B. cepacia (4 STs), B. multivorans (2 STs), B. cenocepacia (3 STs), B. stabilis (2 STs), B. vietnamiensis (2 STs), and B. ambifaria (2 STs). Three B. cenocepacia STs also belonged to 2 different recA lineages defined within this species: IIIA (1 ST) and IIIB (2 STs).
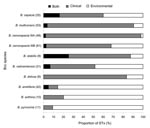
STs occurring in both clinical and environmental niches were found in 6 of the 9 formally described Bcc; the greatest degree of overlap occurred in B. cepacia and B. stabilis (Figure). The proportion of STs not shared between clinical and environmental isolates varied for each Bcc species we examined. This finding may reflect the few clinical or environmental isolates for that species or high genetic diversity; a larger sample size is needed to find identical matches. Species dominated by clinical STs (>83% of STs) were B. multivorans, B. cenocepacia recA lineage IIIA, and B. dolosa. Those species containing mainly environmental STs (>80%) were B. ambifaria, B. anthina, and B. pyrrocinia (Figure). Although this distribution agrees with findings of previous studies (2), it also reflects the distribution of isolates within the collections from which isolates were obtained.
Several ST matches between clinical and environmental isolates were of particular interest. MLST ST-10 was shared by B. cepacia J1050, a human isolate cultured in the United States (Cleveland, Ohio) and the type strain for B. cepacia ATCC 25416, isolated from an onion. This evidence of clonality augments the clonal relationship reported earlier (9) between ATCC 25416 and a UK isolate from a CF patient. The B. multivorans IST455 isolated from a CF patient’s sputum in Portugal, as reported in a previous study (13) had the same sequence type (ST-375) as R-20526, which was isolated from the River Schelde in Belgium.
B. cenocepacia recA lineage IIIA isolates with ST-32 (Table) were from 4 independent sources: POPR8 (isolated from a radish in Mexico), BCC1118 (isolated from a UK non-CF patient infection), R-16597 (isolated from a CF patient in Belgium), and 5–457 (isolated from a CF patient in the Czech Republic). ST-32 appears to be a globally distributed, predominantly clinical strain (A. Baldwin, unpub. data). The B. cenocepacia recA lineage IIIB isolates identified as ST-122 (Table) include the PHDC strains, predominant in US CF patients (AU1054) and previously found in US soil (HI-2424) (10), and CEP0497, which was obtained from a leg wound in a non-CF patient in Canada. Together with a recent report of PHDC strains identified in Europe (14), the Canadian isolate in our study adds further weight to the identification of this ST as a globally distributed strain.
MLST analysis of B. stabilis corroborated the high degree of clonality observed by PFGE fingerprint analysis in the original description of this species (15). However, MLST was further able to distinguish 8 STs among the 26 isolates examined, which indicates that MLST may be a more effective method than PFGE for epidemiologic analysis of B. stabilis. This increased resolution adds to the observation that 2 B. stabilis STs are globally distributed and isolated from clinical samples and an array of different niches, including domestic products, medical solutions, industrial process contaminants, and hospital devices.
In summary, >20% of the clinical isolates we examined were indistinguishable by MLST from isolates from environmental sources. This finding suggests that conservation of intrinsic determinants necessary to thrive in environmental niches may confer an ability to colonize susceptible humans. Further work is urgently required to more extensively investigate the emergence of pathogenic members of the Bcc in the natural environment and the risk for infection this may represent.
Dr Baldwin is a postdoctorate research fellow at the University of Warwick on a 3-year project funded by the Wellcome Trust. His main research interests are horizontal gene transfer, pathogenicity islands, evolutionary biology, and epidemiology of bacterial populations.
Acknowledgments
We thank Angela Marchbank and Lynne Richardson for technical support. This publication made use of the Bcc multilocus sequence typing website (http://pubmlst.org/bcc/) developed by Keith Jolley and hosted at the University of Oxford.
This work was funded by the Wellcome Trust, grant number 072853. The Trust also funded development of the website.
References
- Coenye T, Vandamme P, Govan JR, LiPuma JJ. Taxonomy and identification of the Burkholderia cepacia complex.J Clin Microbiol. 2001;39:3427–36. DOIPubMedGoogle Scholar
- Mahenthiralingam E, Urban TA, Goldberg JB. The multifarious, multireplicon Burkholderia cepacia complex.Nat Rev Microbiol. 2005;3:144–56. DOIPubMedGoogle Scholar
- Govan JR, Brown PH, Maddison J, Doherty CJ, Nelson JW, Dodd M, Evidence for transmission of Pseudomonas cepacia by social contact in cystic fibrosis.Lancet. 1993;342:15–9. DOIPubMedGoogle Scholar
- LiPuma JJ, Dasen SE, Nielson DW, Stern RC, Stull TL. Person-to-person transmission of Pseudomonas cepacia between patients with cystic fibrosis.Lancet. 1990;336:1094–6. DOIPubMedGoogle Scholar
- Hutchinson GR, Parker S, Pryor JA, Duncan-Skingle F, Hoffman PN, Hodson ME, Home-use nebulizers: a potential primary source of Burkholderia cepacia and other colistin-resistant, gram-negative bacteria in patients with cystic fibrosis.J Clin Microbiol. 1996;34:584–7.PubMedGoogle Scholar
- Oie S, Kamiya A. Microbial contamination of antiseptics and disinfectants.Am J Infect Control. 1996;24:389–95. DOIPubMedGoogle Scholar
- Holmes A, Govan J, Goldstein R. Agricultural use of Burkholderia (Pseudomonas) cepacia: a threat to human health?Emerg Infect Dis. 1998;4:221–7.PubMedGoogle Scholar
- LiPuma JJ, Mahenthiralingam E. Commercial use of Burkholderia cepacia.Emerg Infect Dis. 1999;5:305–6.PubMedGoogle Scholar
- Govan JRW, Balendreau J, Vandamme P. Burkholderia cepacia - Friend and foe.ASM News. 2000;66:124–5.
- LiPuma JJ, Spilker T, Coenye T, Gonzalez CF. An epidemic Burkholderia cepacia complex strain identified in soil.Lancet. 2002;359:2002–3. DOIPubMedGoogle Scholar
- Baldwin A, Mahenthiralingam E, Thickett KM, Honeybourne D, Maiden MC, Govan JR, Multilocus sequence typing scheme that provides both species and strain differentiation for the Burkholderia cepacia complex.J Clin Microbiol. 2005;43:4665–73. DOIPubMedGoogle Scholar
- Coenye T, Vandamme P, LiPuma JJ, Govan JR, Mahenthiralingam E. Updated version of the Burkholderia cepacia complex experimental strain panel.J Clin Microbiol. 2003;41:2797–8. DOIPubMedGoogle Scholar
- Cunha MV, Leitao JH, Mahenthiralingam E, Vandamme P, Lito L, Barreto C, Molecular analysis of Burkholderia cepacia complex isolates from a Portuguese cystic fibrosis center: a 7-year study.J Clin Microbiol. 2003;41:4113–20. DOIPubMedGoogle Scholar
- Coenye T, Spilker T, Van Schoor A, LiPuma JJ, Vandamme P. Recovery of Burkholderia cenocepacia strain PHDC from cystic fibrosis patients in Europe.Thorax. 2004;59:952–4. DOIPubMedGoogle Scholar
- Vandamme P, Mahenthiralingam E, Holmes B, Coenye T, Hoste B, De Vos P, Identification and population structure of Burkholderia stabilis sp. nov. (formerly Burkholderia cepacia genomovar IV).J Clin Microbiol. 2000;38:1042–7.PubMedGoogle Scholar
Figure
Table
Cite This ArticleTable of Contents – Volume 13, Number 3—March 2007
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Chris G. Dowson, Department of Biological Sciences, University of Warwick, Coventry, CV4 7AL, United Kingdom;
Top