Volume 15, Number 12—December 2009
Dispatch
Mopeia Virus–related Arenavirus in Natal Multimammate Mice, Morogoro, Tanzania
Abstract
A serosurvey involving 2,520 small mammals from Tanzania identified a hot spot of arenavirus circulation in Morogoro. Molecular screening detected a new arenavirus in Natal multimammate mice (Mastomys natalensis), Morogoro virus, related to Mopeia virus. Only a small percentage of mice carry Morogoro virus, although a large proportion shows specific antibodies.
Arenaviruses are segmented negative-strand RNA viruses. Their natural hosts are various rodent species. The virus family comprises several human pathogens causing hemorrhagic fever, namely Machupo, Guanarito, Junin, Sabia, and Chapare viruses in South America, and Lassa and Lujo viruses in Africa (1–3). In addition, Africa harbors arenaviruses that are not linked with human disease: Mobala, Ippy, Mopeia, and Kodoko viruses (4–7). We conducted a systematic search in wildlife in Tanzania to identify new African arenaviruses.
During 1985 through 1989, a total of 2,520 small mammals were live-trapped in different regions of Tanzania. After species determination, they were measured and bled by orbital puncture. Serum samples were tested by indirect immunofluorescent antibody (IFA) assay (8). Lassa virus was used as antigen due to its cross-reactivity with immune sera from animals infected with other arenaviruses (4,6). Clusters of seropositivity were found in Arvicanthis spp. rodents from the Iringa region (20%) and in Natal multimammate mice (Mastomys natalensis) from Arusha (18%) and Morogoro (17%) (Table 1), which suggests that these animals are reservoirs of arenaviruses. Titers ranged from 16 to 512 and 16 to 4,096 in Arvicanthis spp. rodents and M. natalensis mice, respectively. Peak prevalence in M. natalensis mice was found on the campus of the Sokoine University in Morogoro (23.7% of 746 animals collected over several seasons).
In 2004, M. natalensis mice were trapped in a mosaic of maize fields and fallow grassland at the university campus in the city of Morogoro (6°50′34.9794′′S; 37°38′8.232′′E) to identify the virus. The animal voucher specimens were deposited at the Royal Museum of Central Africa, Tervuren, Belgium. RNA was prepared from 10 μL of rodent serum by using the QIAamp Viral RNA kit (QIAGEN, Valencia, CA, USA), and screening was performed by using a pan–Old World arenavirus reverse transcription–PCR (RT-PCR) specific for the large (L) gene (9). One of 96 serum samples was positive (no. 3017/2004) (Table 2), and sequencing of the PCR fragment showed a new arenavirus sequence. The virus was isolated in Vero cells and called Morogoro virus (strain 3017/2004).
For sequencing, the isolate was propagated in T75 flasks, virus particles in supernatant were pelleted by ultracentrifugation, and RNA was isolated by using the QIAamp Viral RNA kit (QIAGEN). The entire 3.5-kb small (S) RNA segment was amplified by RT-PCR as described previously (10). The 7-kb L RNA segment was amplified in 2 fragments by using a long-range RT-PCR protocol and primers targeting the conserved termini of L RNA and Morogoro virus–specific primers designed on the basis of the sequence of the fragment detected by RT-PCR screening. By using the PCR products as a template, short overlapping fragments were amplified and sequenced with a set of consensus primers for Old World arenaviruses, and S and L RNA sequences were assembled (GenBank accession nos. EU914103 and EU914104). (Sequences reported in this article have been submitted to GenBank and assigned the following accession numbers: full-length S and L RNA sequences of Morogoro virus, EU914103–04; partial L gene sequences of Morogoro virus, EU914107–22; cytochrome B gene of Morogoro virus-positive Mastomys natalensis, EU914105–06.)
Full-length amino acid sequences of glycoprotein precursor (GPC), nucleoprotein (NP), and L protein of Morogoro virus were aligned with published Old World arenavirus sequences and pairwise p distances were calculated. Morogoro virus showed genetic similarity to strains of Mopeia virus that were circulating in Mozambique (4) and Zimbabwe (5). A close relationship between both viruses was also demonstrated by phylogenetic analysis using GPC, NP, and L gene sequences (Figure 1, panel D, and data not shown). Both viruses are sister taxa, sharing a common ancestor with Mobala virus.
Although the distances between Morogoro and Mopeia virus in the amino acid sequence of GPC (12%), NP (12%–13%), and L gene (26%) were higher than intraspecies differences among known African arenaviruses (i.e., pairwise differences between strains of the same species; <11% in GPC and NP; <21% in L), they did not reach the level of interspecies distances (>20% in GPC and NP; >37% in L) (Figure 1, panels A–C). Therefore, we currently consider Morogoro virus a subspecies of Mopeia virus rather than a new arenavirus species. This classification is supported by the fact that both viruses share the same host. Sequencing of the mitochondrial cytochrome b gene of rodent liver samples positive for Morogoro virus confirmed that its natural host is M. natalensis mice (GenBank accession nos. EU914105 and EU914106).
An additional 303 ethanol-preserved liver samples and 63 serum samples were collected in 2004 and 2007, respectively. Liver tissue (≈3 mg) was homogenized by using a bead mill. Cell debris was pelleted by centrifugation, and RNA was isolated from the homogenate with the RNeasy Mini kit (QIAGEN). Testing by L gene RT-PCR (9) showed 16 positive liver and serum samples, which indicated a virus prevalence in the M. natalensis population of ≈4% (Table 2). PCR fragments were sequenced (GenBank accession nos. EU914107–EU914122), and Morogoro virus was isolated in cell culture from all 4 PCR-positive serum samples obtained in 2007. Morogoro virus–specific antibodies in serum samples from 2004 and 2007 were measured by IFA assay using Vero cells infected with Morogoro virus. The antibody prevalence was ≈50%, which compares quite well with the 23% prevalence determined in this area 20 years before. In some animals, virus and antibodies were detected (Table 2).
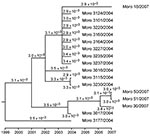
The availability of Morogoro virus L gene sequences from 2004 and 2007, originating from the same host population (trapping sites <1 km apart), provided us with the opportunity to estimate the molecular clock rate for this virus. Phylogenetic reconstruction was performed with the BEAST version 1.4.8 package (http://beast.bio.ed.ac.uk) (11) under the assumption of a relaxed lognormal molecular clock and general time reversible (GTR) or Hasegawa-Kishino-Yano (HKY) substitution model with gamma-distributed substitution rate variation among sites (Figure 2 and data not shown). Analysis was run for 2 million Markov chain Monte Carlo steps, which yielded a reliable set of data as verified with the TRACER program (http://tree.bio.ed.ac.uk/software/tracer). Based on GTR and HYK model, 3.2 × 10–3 and 3.4 × 10–3 substitutions per site and year (95% interval of highest posterior density 1.1–6.6 × 10–3), respectively, were calculated.
A serologic survey in small mammals from Tanzania identified a hot spot of arenavirus circulation in Morogoro in the late 1980s. This work is being published now because early attempts to substantiate the existence of the virus failed. The identification of the virus was facilitated by a recently developed pan–Old World arenavirus PCR (9) that also led to the discovery of new arenaviruses in rodents from West Africa (7). Only a small percentage of M. natalensis mice carry Morogoro virus, and a large proportion shows specific antibodies, which indicates that most animals clear the virus during life. Viruses and antibodies, which are presumbably directed to nucleocapsid proteins, also co-circulate, as seen in hantavirus infection in rodents (12). Detection of Morogoro virus in the liver is consistent with the organ tropism of Lassa virus in M. natalensis mice (13). In agreement with studies on Lassa virus strains, the largest genetic distance between Morogoro and Mopeia virus was seen in L gene, which contains several highly variable regions (14).
The clock rate estimate of 3 × 10–3 for Morogoro virus L gene is in agreement with that of other RNA viruses (15), although it must be interpreted with caution, given that the difference in date between the samples is not large. The tree topology did not correlate with geographic or ecologic sampling data.
The pathogenicity of Morogoro virus for humans is not known, though its phylogenetic clustering with African arenaviruses that are not linked with human disease (4–6) and the absence of hemorrhagic fever in the area suggest that it does not cause severe disease. Hospital-based investigations are required to estimate the public health relevance of this virus.
Dr Günther is head of the Virology Department at the Bernhard-Nocht-Institute for Tropical Medicine, Hamburg, Germany. His research interests are molecular biology and epidemiology of arenaviruses, in particular, Lassa virus.
Acknowledgments
We thank the Tanzanian authorities and the academic authorities of the Sokoine University of Agriculture, Morogoro, who provided us with the necessary permits and working facilities; and the field staff as well as Mike Michiels, Jan Stuyck, and Bukheti S. Kilonzo for their help in collecting animals.
The early work was supervised and stimulated by the late Walter Verheyen, within the framework of the Tanzanian-Belgium Joint Rodent Research Project (supported by the Belgian General Administration for Developmental Cooperation); the recent work was undertaken under the SUA-VLIR Interuniversity Cooperation program of the Flemish Interuniversity Council and the VIZIER integrated project grant LSHG-CT-2004-511960 of the European Union 6th Framework. The Bernhard-Nocht-Institute is supported by the Bundesministerium für Gesundheit and the Freie und Hansestadt Hamburg.
References
- Delgado S, Erickson BR, Agudo R, Blair PJ, Vallejo E, Albarino CG, Chapare virus, a newly discovered arenavirus isolated from a fatal hemorrhagic fever case in Bolivia. PLoS Pathog. 2008;4:e1000047. DOIPubMedGoogle Scholar
- Briese T, Paweska JT, McMullan LK, Hutchison SK, Street C, Palacios G, Genetic detection and characterization of Lujo virus, a new hemorrhagic fever–associated arenavirus from southern Africa. PLoS Pathog. 2009;5:e1000455. DOIPubMedGoogle Scholar
- Wulff H, McIntosh BM, Hamner DB, Johnson KM. Isolation of an arenavirus closely related to Lassa virus from Mastomys natalensis in south-east Africa. Bull World Health Organ. 1977;55:441–4.PubMedGoogle Scholar
- Johnson KM, Taylor P, Elliott LH, Tomori O. Recovery of a Lassa-related arenavirus in Zimbabwe. Am J Trop Med Hyg. 1981;30:1291–3.PubMedGoogle Scholar
- Gonzalez JP, McCormick JB, Saluzzo JF, Herve JP, Georges AJ, Johnson KM. An arenavirus isolated from wild-caught rodents (Pramys species) in the Central African Republic. Intervirology. 1983;19:105–12. DOIPubMedGoogle Scholar
- Lecompte E, ter Meulen J, Emonet S, Daffis S, Charrel RN. Genetic identification of Kodoko virus, a novel arenavirus of the African pigmy mouse (Mus Nannomys minutoides) in West Africa. Virology. 2007;364:178–83. DOIPubMedGoogle Scholar
- van der Groen G, Kurata T, Mets C. Modifications to indirect immunofluorescence tests on Lassa, Marburg, and Ebola material. Lancet. 1983;1:654. DOIPubMedGoogle Scholar
- Vieth S, Drosten C, Lenz O, Vincent M, Omilabu S, Hass M, RT-PCR assay for detection of Lassa virus and related Old World arenaviruses targeting the L gene. Trans R Soc Trop Med Hyg. 2007;101:1253–64. DOIPubMedGoogle Scholar
- Günther S, Emmerich P, Laue T, Kühle O, Asper M, Jung A, Imported Lassa fever in Germany: molecular characterization of a new Lassa virus strain. Emerg Infect Dis. 2000;6:466–76. DOIPubMedGoogle Scholar
- Drummond AJ, Ho SY, Phillips MJ, Rambaut A. Relaxed phylogenetics and dating with confidence. PLoS Biol. 2006;4:e88. DOIPubMedGoogle Scholar
- Essbauer SS, Schmidt-Chanasit J, Madeja EL, Wegener W, Friedrich R, Petraityte R, Nephropathia epidemica in metropolitan area, Germany. Emerg Infect Dis. 2007;13:1271–3.PubMedGoogle Scholar
- Walker DH, Wulff H, Lange JV, Murphy FA. Comparative pathology of Lassa virus infection in monkeys, guinea-pigs, and Mastomys natalensis. Bull World Health Organ. 1975;52:523–34.PubMedGoogle Scholar
- Vieth S, Torda AE, Asper M, Schmitz H, Günther S. Sequence analysis of L RNA of Lassa virus. Virology. 2004;318:153–68. DOIPubMedGoogle Scholar
- Jenkins GM, Rambaut A, Pybus OG, Holmes EC. Rates of molecular evolution in RNA viruses: a quantitative phylogenetic analysis. J Mol Evol. 2002;54:156–65. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleTable of Contents – Volume 15, Number 12—December 2009
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Stephan Günther, Bernhard-Nocht-Institute for Tropical Medicine Department of Virology, Bernhard-Nocht-Str 74, 20359 Hamburg, Germany
Top