Volume 17, Number 1—January 2011
Letter
Zoonotic Cryptosporidiosis from Petting Farms, England and Wales, 1992–2009
To the Editor: Visits to petting farms in England and Wales recently have increased in popularity. Petting farms are commercial operations at which visitors, mainly families and organized groups, are encouraged to have hands-on contact with animals. The ≈1,000 petting farms in the United Kingdom collectively receive >2 million visitors per year, with peak visitor times during school and public holidays. Commercial farms also may host farm visits on single days for group and school visits. The farm attraction business is a substantial part of the rural economy, generating >£12 million annually (1).
During 1992–2009, a total of 55 outbreaks of infectious intestinal disease associated with petting farms in England and Wales was reported to the Health Protection Agency. Verocytotoxin-producing Escherichia coli O157 (VTEC O157) caused 30 (55%) of these outbreaks (244 persons were affected [range 2–93, mean 8 persons] and 84 were hospitalized); Salmonella enterica serovar Typhimurium definitive phage type 104 caused 2 (3%) of the outbreaks. A total of 23 (42%) petting farm outbreaks were caused by Cryptosporidium spp. (1,078 persons were affected [range 2–541, mean 45 persons] and 29 were hospitalized). We report on these cryptosporidiosis outbreaks as a reminder of the risk to petting farm visitors.
Contributory factors reported in the cryptosporidiosis outbreaks included direct contact with preweaned lambs, calves, kids, or animal feces (e.g., diarrhea in lambs, a recognized risk factor for cryptosporidiosis; 11/23 [48%]) and inadequate hand washing facilities (7/23 [30%]). Of outbreaks in which hand washing facilities were inadequate, thumb sucking by children was also noted in 1; in another, alcohol-based hand gels and sanitizers, which are ineffective against Cryptosporidium spp., were used.
Cryptosporidium spp. are coccidian parasites that infect a wide range of farm livestock, including cattle, sheep, goats, pigs, horses, and deer, but are mainly a veterinary problem in neonatal ruminants. C. parvum, for example, is a common agent in the etiology of the neonatal diarrhea syndrome of calves, lambs, and goat kids. Widespread asymptomatic carriage of this parasite exists in livestock in the United Kingdom (2). In humans, cryptosporidiosis occurs most commonly in children <5 years of age, can be life threatening in immunocompromised persons, and is caused predominantly by C. hominis and C. parvum parasites. Fecal–oral transmission can occur directly from animal to person and from person to person or indirectly through contaminated food or water (2).
Typing of Cryptosporidium spp. has been undertaken by the UK Cryptosporidium Reference Unit since 1999. C. parvum was identified from human feces in 12 (75%) of the 16 petting farm outbreaks since 1999 (feces were not submitted for typing in 4). Additionally, Cryptosporidium spp. oocysts were detected and confirmed as C. parvum from suspected sources (lambs, calves) in 4 (33%) of these 12 outbreaks and linked by GP60 subtype to human cases in 3 outbreaks. Zoonotic risk factors in case–control studies of sporadic cryptosporidiosis cases in England and Wales also have identified an association between C. parvum infection and touching farm animals or visiting a farm (3).
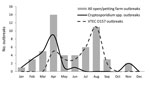
In petting farm outbreaks, Cryptosporidium spp. displayed a seasonal pattern, as did VTEC O157. Cryptosporidiosis outbreaks occurred more often in springtime (18 vs. 5; p = 0.0001) than did VTEC O157 outbreaks, which occurred more frequently during the summer (25 vs. 5; p<0.00001), especially in August (Figure). During spring 2010, two additional C. parvum outbreaks associated with contact with lambs at petting farms were reported in England. Control measures included restricting bottle feeding of lambs and enhancing the supervision of hand washing. The associations with outbreaks of cryptosporidiosis in spring and contact with young farm animals also has been reported in Scotland (4).
Despite the 2 separate seasonal peaks of infection, care should be exercised throughout the year. The importance of careful attention to hygiene and supervision of children visiting farms and the need for appropriate facilities, such as those for hand washing, are covered in the UK Health and Safety Executive standards; operators of petting farms are expected to meet these standards (5). These guidelines also apply to commercial farms hosting open days. A good practice reminder on managing the risks from VTEC O157 in a petting farm context was published by the Health Protection Agency, Health and Safety Executive, and the Local Government Regulation (6). Guidance on the control of VTEC O157 infections for farms open to public access applies equally to most gastrointestinal pathogens, including Cryptosporidium spp. The need for a sound approach to managing hygiene control measures at petting farms cannot be overemphasized.
Acknowledgment
We thank all reporting investigators in England and Wales, including HPA Health Protection Units (England), Public Health Wales, microbiologists, local authorities, and environmental health practitioners for their continual support in reporting to the electronic foodborne and nonfoodborne gastrointestinal outbreaks surveillance system.
References
- Restoring confidence in open farms to educate our children. Farmers Guardian 2010, January 29 [cited 2010 May 25]. http://www.farmersguardian.com/home/rural-life/country-view/restoring-confidence-in-open-farms-to-educate-our- children/29936.article
- Chalmers RM, Giles M. Zoonotic cryptosporidiosis in the UK—challenges for control. J Appl Microbiol. 2010;109:1487–97. DOIPubMedGoogle Scholar
- Hunter PR, Thompson RC. The zoonotic transmission of Giardia and Cryptosporidium. Int J Parasitol. 2005;35:1181–90. DOIPubMedGoogle Scholar
- McGuigan CC, Steven K, Pollock KGJ. Cryptosporidiosis associated with wildlife center, Scotland [letter]. Emerg Infect Dis. 2010;16:895–6.PubMedGoogle Scholar
- Health and Safety Executive. Avoiding ill health at open farms—advice to farmers (with teachers’ supplement) [cited 2010 May 25]. http://www.hse.gov.uk/pubns/ais23.pdf
- Health and Safety Executive, Local Authorities Coordinators of Regulatory Services, and Health Protection Agency. Understanding and managing the risks from E. coli O157 in an open farm context [cited 2010 May 25]. http://www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1267551712693
Figure
Cite This ArticleRelated Links
Table of Contents – Volume 17, Number 1—January 2011
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Fraser J. Gormley, Health Protection Agency–Gastrointestinal, Emerging and Zoonotic Infections, Health Protection Services: Colindale, 61 Colindale Ave, London NW9 5EQ, UK
Top