Volume 17, Number 8—August 2011
Dispatch
Poliomyelitis Outbreak,Pointe-Noire, Republic of the Congo, September 2010–February 2011
Cite This Article
Citation for Media
Abstract
On November 4, 2010, the Republic of the Congo declared a poliomyelitis outbreak. A cross-sectional survey in Pointe-Noire showed poor sanitary conditions and low vaccination coverage (55.5%), particularly among young adults. Supplementary vaccination should focus on older age groups in countries with evidence of immunity gaps.
On November 4, 2010, the Ministry of Health of the Republic of the Congo officially declared a poliomyelitis outbreak centered in Pointe-Noire following the laboratory identification of poliovirus type 1 in a patient with acute flaccid paralysis (AFP) (1,2). A provisional total of 554 AFP case-patients that included a high proportion (68%) of male patients was identified nationally, with paralysis onset from September 20, 2010, through February 27, 2011 (3). During this same period, 451 cases (81.4%), which included 184 deaths, were reported in Pointe-Noire. Most cases were found in the young adult population (57.4% in patients 15–24 years of age), which had a higher case-fatality ratio (CFR) of 40.8% compared with the general population of the country (3).
In most developing countries, prevention and control of poliomyelitis relies on oral polio vaccine (OPV). Routine vaccination focuses on infants <11 months of age with trivalent OPV, and supplementary immunization activities (SIAs) provide additional opportunities for vaccination for children <5 years of age (4,5). In response to the epidemic, the Ministry of Health, in collaboration with the World Health Organization, launched 4 rounds of national SIAs that used monovalent type 1 and bivalent types 1 and 3 OPV during November 12–16, 2010, December 3–7, 2010, January 11–15, 2011, and February 22–26, 2011 (3). To assess risk factors for infection and estimate vaccination coverage, Epicentre and Médecins Sans Frontières implemented a cross-sectional survey in 1 affected neighborhood of Pointe-Noire.
This survey was a single-community rapid assessment of epidemiologic conditions potentially contributing to the outbreak, including vaccination coverage. The survey was done in Mbota, a neighborhood composed of 4 sectors, comprising 9.5% of the city population. This neighborhood was selected from Loandjili district (Figure 1) on the basis of local expert consultation to ensure socioeconomic diversity and representativeness. To estimate vaccination coverage of 80% among children with 5% precision at a 95% confidence level, we aimed to sample at least 246 households. We assumed each household had on average 1 child <5 years of age. We also assumed 5 persons per household on average, which corresponds to ≈1,230 persons overall. Households were selected in each sector of the neighborhood. From a starting point on the border of the sector, interviews focused on every fifth household, following a predefined direction toward the center of the sector, subsequently covering the entire neighborhood. Data were collected through face-to-face interviews December 9–10, 2010, by using a structured questionnaire. The questions included household demographics, water supply, and sanitary conditions. In addition, information for each person in the household was collected about vaccination history (routine and SIAs), any previous illness, and access to health care during the past 3 months. Vaccination coverage was estimated on the basis of reported personal history or documentary evidence of vaccination: a fingernail marked with ink indicating vaccination during SIAs or a vaccination card indicating routine vaccination.
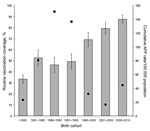
Data were eventually collected from 1,849 persons in 317 households of Mbota with all ages and both genders represented. Following the 2 first rounds of SIAs, most surveyed persons (1,812 [98%], 95% confidence interval [CI] 97.3%–98.6%) reported having been vaccinated with monovalent OPV and 1,769 (95.7%, 95% CI 94.7%–96.6%) received 2 doses in November and December 2010. Among vaccinated persons, 627 (33.9%, 95% CI 31.7%–36.1%) had fingernails marked with ink; the rest were absent during the interview or ink had already worn off. There were no significant differences in SIA vaccine coverage by gender or age. Routine vaccination coverage was estimated as 55.5% (95% CI 53.3%–57.8%) among the surveyed persons (Table 1). Among reported vaccinated persons, 21.3% (95% CI 18.8%–23.8%) showed their vaccination card, and among those, 78.7% (95% CI 73.1%–84.4%) were vaccinated >3 times. Routine vaccination coverage did not vary significantly by gender but decreased with age (p <0.0001). For persons younger than 5 years, it was 87.5% (95% CI 83.6%–91.4%) and <52% for anyone >15 years of age. In the most affected age groups, 15–19 and 20–24 years, vaccination coverage was estimated to be respectively 49.3% (95% CI 42.4%–56.1%) and 46.2% (95% CI 39.3%–53.1%) (Figure 2). By comparison, administrative vaccination coverage varied since 1986 between a reported 21% in 1997 and 112% in 2009 (Table 2).
The number of persons per bedroom, an indicator of crowding, ranged between 1 and 9, and there were >4 persons per bedroom for 12.1% (95% CI 8.4%–15.7%) of all households with no statistical differences among sectors. Tap water either from a neighbor’s house (41.9%, 95% CI 35.9%–47.8%) or within the house (30.7%, 95% CI 25.2%–36.3%) was the primary potable water source recorded. Wells were also common (23.3%, 95% CI 18.3%–28.4%). When the primary source of potable water was unavailable, wells were the most frequently mentioned alternative source (37.8%, 95% CI 32.0%–43.6%). Most households reported use of a latrine shared with neighbors (57.4%, 95% CI 51.8%–63.1%) or within their house (31.4%, 95% CI 26.1%–36.7%). Few surveyed persons (16.1%, 95% CI 14.4%–17.7%) reported illness during the recall period, but if sick, 73.3% (95% CI 67.4%–79.2%) they sought health care, which suggests little underreporting of AFP cases.
The cross-sectional survey confirmed administrative estimates of low routine vaccination decreasing with age. Specifically, in the surveyed young adult population (15–29 years of age) it varied between a reported 46.2% and 52.6%. According to administrative data, the reported vaccination coverage varies between 41.7% and 79% in young adults between 15 and 24 years of age. Civil conflicts spanning the 1990s have potentially undermined vaccination efforts, especially affecting those currently 10–20 years of age. A further method of protection for a person is past exposure to wildtype strains. To our knowledge, no polio transmission had been reported in Pointe-Noire since the last outbreak in the city in 1969 (6). Low vaccination coverage and no previous exposure to wild virus likely led to an accumulation of susceptible persons. Once introduced, the disease spread quickly through this highly susceptible, undervaccinated, and underexposed young adult population, with disease spread facilitated by frequent flooding and poor to medium household sanitation conditions, i.e., crowding sleeping areas, shared latrines between households, and common sources for water consumption.
Poliovirus infections lead to clinical disease more frequently in older age groups (7), which partially explains the observed shift of AFP cases toward young adult populations. Moreover, children were better protected with higher vaccination coverage. Death is more frequent when infection occurs in older age groups (8,9), which explains part of the high observed CFR. Clinical manifestations of poliovirus infections are more common in boys and men than in girls and women (10), as observed, and even though males and females share similar vaccination coverage, women in the young adult age groups may have additionally benefitted from exposure to excreted OPV while caring for the young (11).
As seen in the Republic of the Congo, or previously in Namibia (12), Cape-Verde (13), any country with no recent wild-type polio transmission and a similarly low level of vaccination coverage may face similar outbreaks characterized by a large proportion of cases in older age groups and a high CFR (14). Avoiding outbreaks will rely on ensuring vaccination of the at-risk population. Routine vaccination activities should be reinforced by SIAs punctually focusing on older age groups (especially among persons 15–35 years of age) when evidence of immunity gaps are documented by serologic surveys or low historical vaccination coverage data. Lessons from the epidemic should benefit health authorities in better prevention and response to further outbreaks on the road to eradication.
Dr Le Menach is an epidemiologist specialized in infectious diseases modeling, surveillance, prevention, and control. He works at London Regional Epidemiology Unit of the Health Protection Agency, as part of the European program for intervention epidemiology (EPIET).
Acknowledgment
We thank the Ministry of Health for support and collaboration, the hospital directors and laboratory director in Pointe-Noire, and colleagues from World Health Organization and the Centers for Disease Control and Prevention for the harmonization of the database and stimulating technical discussions.
References
- Grard G, Drexler JF, Lekana-Douki S, Caron M, Lukashev A, Nkoghe D, Type 1 wild poliovirus and putative enterovirus 109 in an outbreak of acute flaccid paralysis in Congo, October–November 2010. Euro Surveill. 2010;15:pii:19723.
- Roberts L. Infectious disease. Polio outbreak breaks the rules. Science. 2010;330:1730–1. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Poliomyelitis outbreak—Republic of the Congo, September 2010–February 2011. MMWR Morb Mortal Wkly Rep. 2011;60:312–3.PubMedGoogle Scholar
- Global Polio Eradication Initiative. Strategy. 2010 [cited 2010 Nov 22]. http://www.polioeradication.org/Aboutus/Strategy.aspx
- World Health Organization. Immunization surveillance, assessment and monitoring. 2011 [cited 2011 Jan 12]. http://www.who.int/immunization_monitoring/en/
- Heraut L, Rousseau E, Aubry P. Poliomyelitis epidemic at Pointe-Noire [in French]. Med Trop (Mars). 1969;29:362–4.PubMedGoogle Scholar
- Gawne AC, Halstead LS. Post-polio syndrome: pathophysiology and clinical management. Crit Rev Phys Rehabil Med. 1995;7:147–88.
- Weinstein L. Influence of age and sex on susceptibility and clinical manifestations in poliomyelitis. N Engl J Med. 1957;257:47–52. DOIPubMedGoogle Scholar
- Weinstein L, Shelokov A, Seltser R, Winchell GD. A comparison of the clinical features of poliomyelitis in adults and in children. N Engl J Med. 1952;246:297–302. DOIPubMedGoogle Scholar
- Froeschle JE, Feorino PM, Gelfand HM. A continuing surveillance of enterovirus infection in healthy children in six United States cities. II. Surveillance enterovirus isolates 1960–1963 and comparison with enterovirus isolates from cases of acute central nervous system disease. Am J Epidemiol. 1966;83:455–69.PubMedGoogle Scholar
- Alexander JP Jr, Gary HE Jr, Pallansch MA. Duration of poliovirus excretion and its implications for acute flaccid paralysis surveillance: a review of the literature. J Infect Dis. 1997;175(Suppl 1):S176–82. DOIPubMedGoogle Scholar
- Nathanson N, Kew OM. From emergence to eradication: the epidemiology of poliomyelitis deconstructed. Am J Epidemiol. 2010;172:1213–29. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleTable of Contents – Volume 17, Number 8—August 2011
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Arnaud Le Menach, Health Protection Agency, 151 Buckingham Palace Rd, London SW1W 9SZ, UK
Top