Volume 19, Number 3—March 2013
CME ACTIVITY - Research
Increasing Pneumocystis Pneumonia, England, UK, 2000–2010
Introduction

Medscape, LLC is pleased to provide online continuing medical education (
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education through the joint sponsorship of Medscape, LLC and Emerging Infectious Diseases. Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit(s)TM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 70% minimum passing score and complete the evaluation at www.medscape.org/journal/eid; (4) view/print certificate.
Release date: February 19, 2012; Expiration date: February 19, 2013
Learning Objectives
Upon completion of this activity, participants will be able to:
• Describe changes in incidence of Pneumocystis jirovecii pneumonia in England from 2000–2010, based on findings of a database study
• Describe changes in risk factors associated with P. jirovecii pneumonia in England from 2000–2010, based on findings of a database study
• Describe the clinical and public health implications of the study findings.
CME Editor
P. Lynne Stockton, VMD, MS, ELS(D), Technical Writer/Editor, Emerging Infectious Diseases. Disclosure: P. Lynne Stockton, VMD, MS, ELS(D), has disclosed no relevant financial relationships.
CME Author
Laurie Barclay, MD, freelance writer and reviewer, Medscape, LLC. Disclosure: Laurie Barclay, MD, has disclosed no relevant financial relationships.
Authors
Disclosures: Rishma Maini, MBChB; Katherine L. Henderson, MSc; Elizabeth A. Sheridan, MBBS, FRCPath; Theresa Lamagni, MSc, PhD; Gordon Nichols, PhD; Valerie Delpech, MBBS, MPH, FPHM; and Nick Phin, MBChB, LLM, have disclosed no relevant financial relationships.
Abstract
After an increase in the number of reported cases of Pneumocystis jirovecii pneumonia in England, we investigated data from 2000–2010 to verify the increase. We analyzed national databases for microbiological and clinical diagnoses of P. jirovecii pneumonia and associated deaths. We found that laboratory-confirmed cases in England had increased an average of 7% per year and that death certifications and hospital admissions also increased. Hospital admissions indicated increased P. jirovecii pneumonia diagnoses among patients not infected with HIV, particularly among those who had received a transplant or had a hematologic malignancy. A new risk was identified: preexisting lung disease. Infection rates among HIV-positive adults decreased. The results confirm that diagnoses of potentially preventable P. jirovecii pneumonia among persons outside the known risk group of persons with HIV infection have increased. This finding warrants further characterization of risk groups and a review of P. jirovecii pneumonia prevention strategies.
Anecdotal reports from clinicians suggest that incidence of Pneumocystis jirovecii pneumonia, previously referred to as P. carinii pneumonia or PCP, among immunosuppressed patients, especially renal transplant recipients, has increased substantially (1). To investigate this claim, we analyzed data for January 2000 through December 2010, using several national data sources: Hospital Episode Statistics, routine laboratory reporting, death certificate data, and HIV surveillance data.
P. jirovecii pneumonia gained notoriety during the AIDS pandemic (2); however, the reservoirs, modes of transmission, and pathogenesis of this organism remain poorly understood (3). Subclinical infection is considered common because studies have shown that anti–P. jirovecii antibodies develop during early childhood (4). Reactivation of latent infection after immunosuppression of the host was thought to be the main pathogenic mechanism (3); however, recent studies indicate that person-to-person spread might cause acute infection in susceptible persons (5).
Although not fully characterized, the known risk factors for P. jirovecii infection include impaired immunity because of HIV infection, hematologic malignancies, and connective tissue disorders (6). Immunosuppressive agents used to treat or prevent graft rejection have been implicated; such agents include corticosteroids, methotrexate, cyclosporine, mycophenolate mofetil, bendamustine, cyclophosphamide (7–11), and, recently, novel immunomodulating drugs, such as tumor necrosis factor–α inhibitors (12).
Prophylactically administered oral trimethoprim–sulfamethoxazole, dapsone, or atovaquone prevent the clinical manifestation of P. jirovecii infection. Also effective for decreasing P. jirovecii infection incidence among HIV-positive patients with a CD4+ count <200/μL is routine prophylactic administration of antimicrobial drugs (13,14).
Given the existence of effective chemoprophylaxis, identification of new risk groups might help prevent future increases in P. jirovecii infection incidence. Therefore, we conducted a retrospective analysis of multiple national data sources to examine trends in P. jirovecii infection.
The Health Protection Agency has approval from the National Information Governance Board for Health and Social Care for the collation of surveillance data in accordance with section 251 of the National Health Service Act 2006. No additional ethical approval was required for this study.
Hospital Episode Statistics
The Hospital Episode Statistics (HES) database contains details of all inpatient admissions to National Health Service hospitals in England. We identified all patients for whom an International Classification of Diseases, 10th Revision (ICD-10), code B59, which corresponds with P. jirovecii infection, was recorded in any of the first 10 diagnosis fields from January 2000 through December 2010. By using ICD-10 and Operating Procedure Code Supplement 4 codes, we then subdivided cases into non–mutually exclusive, condition-specific categories that are frequently cited in the literature in association with P. jirovecii (7–13,15–19). The categories covered were renal failure, hematologic malignancy, other hematologic disorders, systemic connective tissue disorders, inflammatory diseases (such as rheumatoid or psoriatic arthritis), and receipt of immunosuppressive agents or an organ transplant. Patients with chronic lung conditions, such as pulmonary fibrosis, were categorized as a single group, given the observed frequency in this study of concurrence of this condition with P. jirovecii infection. Patients who did not fit into any risk category were also included in the analysis.
We cross-checked for duplicate records and selected the record of first admission for each patient. We examined information about sex, age, and geographic distribution of patients. HIV-infected patients were excluded from analysis because the clinical records for these patients did not contain patient-identifiable information (unlike the other clinical records in the HES database), thereby making identification and exclusion of duplicate records not possible for this group.
Routine Laboratory Reporting
LabBase2 is the Health Protection Agency’s national communicable diseases database for England, Wales, and Northern Ireland; it receives semiautomated downloads of results from 99% of microbiology diagnostic laboratories (Health Protection Agency, unpub. data). Laboratory-confirmed cases of P. jirovecii infection in England during 2000–2010 were extracted from LabBase2, and duplicate laboratory samples were excluded.
Death Certificate Data
For the study period, deaths in England with an ICD-10 clinical code indicating P. jirovecii as the cause or contributory cause of death were extracted from Office for National Statistics data. Deaths from P. jirovecii infection linked to a diagnosis of HIV or AIDS were also analyzed.
HIV Surveillance Data
Data from the Health Protection Agency’s HIV and AIDS New Diagnoses and Deaths database were analyzed (20). Because HIV surveillance data are available for adults only, epidemiologic information in this study was restricted to patients >15 years of age. P. jirovecii infections were reported as co-infections at the time of HIV diagnosis, as subsequent AIDS diagnoses, or as the cause of death.
Statistical Analyses
We used the statistical software STATA/SE 11.2 (21) for all analyses. Poisson regression with an offset for resident population, which used Office for National Statistics midyear estimates, was used to calculate the annual incidence rate ratio with 95% CIs. The Pearson χ2 test was used to examine changes in the proportion of cases by risk category over time (2000–2005 vs. 2006–2010).
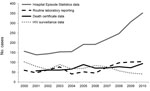
The absolute numbers of cases of P. jirovecii pneumonia in England during 2000–2010, reported by each national surveillance system, are shown in Figure 1 and Table 1. We describe data from each system separately.
Hospital Episode Statistics
During the study period, HES recorded 2,258 cases of P. jirovecii pneumonia. The number of cases increased from 157 in 2000 to 352 in 2010, an average annual increase of 9% (p<0.001).
Cases reported to HES were not restricted to a particular geographic area, and the data showed no obvious seasonal trends. Because the increase in cases began in the latter half of the decade (Figure 1), we compared data from 2000–2005 with that from 2006–2010. This comparison showed a marked change in the age distribution of patients hospitalized for P. jirovecii infection during 2006–2010; relatively more patients were 60–69 years of age (Figure 2). Among all age groups, there was a higher proportion of male than female patients with P. jirovecii infection.
During the study period, 81% of patients within the HES database who had a diagnosis of P. jirovecii pneumonia could be classified according to a defined risk category (Table 2). Most (40.6%) had a hematologic malignancy, and 17.5% had preexisting lung disease. Relative distribution of risk groups differed significantly between 2000–2005 and 2006–2010 for all risk categories (χ2 28.2, 7 degrees of freedom, p<0.001). The numbers of patients with P. jirovecii pneumonia increased significantly in all risk groups, but the difference in rates between the 2 periods was most marked among patients who had undergone transplantation, 47% of whom had undergone kidney transplantation during 2000–2010. The number of patients who were not in any of the risk groups described above dropped by 19% between the 2 periods. This test was conservative because there was some overlap between the risk categories.
Routine Laboratory Reporting
During the study period, LabBase2 recorded 765 laboratory-confirmed cases. Reported cases of P. jirovecii pneumonia remained relatively unchanged during 2000–2006 (range 41–77 cases/year, mean 55 cases/year) but increased from 76 cases in 2007 to 98–104 cases during 2008–2010 (Figure 1), particularly in older patients. The male-to-female ratio of P. jirovecii pneumonia patients during 2000–2010 was 2.5 to 1.0.
Death Certificate Data
Deaths for which P. jirovecii pneumonia was recorded as a cause or contributing factor rose from 57 in 2001 to 94 in 2010 (p<0.001). For several years, the numbers of P. jirovecii infections reported on death certificates as a contributory cause of death were greater than those captured by laboratory reports (Figure 1).
HIV Surveillance Data
The numbers of patients with P. jirovecii pneumonia and HIV infection decreased 7% per year during 2000–2010 (p<0.001) (Figure 3). Most P. jirovecii infection diagnoses were made at the time of HIV diagnosis. Within this group of HIV-infected patients, death from P. jirovecii infection remained relatively stable over this period.
In this study, we found an increasing trend in rates for clinical cases recorded in HES and microbiologically confirmed and reported cases in England during 2000–2010. This finding suggests a real increase in the numbers of cases of P. jirovecii pneumonia diagnosed. We also found an association between P. jirovecii infection and a variety of chronic lung diseases not described in the literature as being associated with P. jirovecii infection. On the basis of these data, we propose preexisting lung disease as a new P. jirovecii pneumonia risk category.
The HES database yielded 2,258 cases of P. jirovecii pneumonia during 2000–2010, but LabBase2 found only 765. The differences in number of cases suggests substantial underreporting by laboratories, although most cases might be diagnosed on the basis of clinical or radiologic findings or by immunofluorescence in the cytology department without being microbiologically confirmed.
An analysis of the Health Protection Agency database of HIV-infected persons shows clear evidence of a substantial reduction in P. jirovecii infections during 2000–2010, consistent with an earlier diagnosis of HIV and receipt of effective antiretroviral therapy (14). P. jirovecii infections among HIV-infected persons declined, whereas P. jirovecii infections among non–HIV-infected persons increased, suggesting that other risk factors must be responsible for the increased numbers of cases.
Given the substantial illness and death associated with P. jirovecii infection and the resources needed to manage these cases, the increase in cases is of serious concern. Many patients need treatment in intensive care units. However, prophylactic use of antimicrobial drugs is highly effective for preventing the disease. A study in the United States suggested that almost $5 million a year could be saved in the state of Maryland alone if prophylaxis were instituted for all HIV-positive patients at risk for P. jirovecii infection (22).
Potential Causes of the Observed Increase
The increased number of cases might reflect changes in ascertainment of cases and increased infections in immunosuppressed patients who have received chemotherapy. It is possible that ascertainment increased over the study period because of improved diagnostic methods; immunofluorescence staining is being replaced by more sensitive PCR methods (23). We were not able to test the hypothesis that the increased number of cases is the result of increased testing for P. jirovecii because the laboratory surveillance system captures positive samples only, not the total number of samples submitted. However, the change in age distribution of patients toward a much older age group suggests that increased testing is not the main reason for increased case detection.
With regard to immunosuppression, an area that has seen an increase in the use of potent immunosuppressant agents is transplant surgery. Recipients who are not well matched to donor human leukocyte antigens now receive more powerful drugs. That said, the proportion of patients receiving renal transplants with a moderate degree of human leukocyte antigen mismatch has remained stable, represented by 43.9% of patients during financial year 2009–10 (National Health Service Blood and Transplant Authority, pers. comm.). Similarly, data from the National Health Service Blood and Transplant Authority indicate that the number of renal transplantations increased by 25% during 2006–2010. Again, this increase was not proportional to that observed for P. jirovecii infections reported for renal transplant recipients, which was ≈388% over the same period (National Health Service Blood and Transplant Authority, pers. comm.), so the increase cannot be explained simply by an increase in the number of patients in this risk group.
The largest group of persons affected by P. jirovecii pneumonia is those with hematologic malignancies. This finding might reflect the 30% increase in diagnoses of these malignancies during 2000–2010 (24). However, the increase in patients in this risk group with P. jirovecii pneumonia was 209% over the same period.
A possible explanation for the increase in P. jirovecii pneumonia cases is an increase in the number of potentially vulnerable patients who did not receive appropriate prophylactic therapy. Guidelines recommend the use of antimicrobial drug prophylaxis for kidney transplant recipients and for patients with hematologic malignancies who are receiving certain chemotherapy (25–28). A Cochrane review recommends prophylaxis for patients with hematologic malignancies and for recipients of bone marrow and solid organ transplants (29). Our study identified a new group at risk for P. jirovecii infection: patients with preexisting lung disease. To determine whether any preventative measures would be advisable for these patients will require further detailed characterization and quantification of risk within this group.
Another possible explanation for the increase in P. jirovecii pneumonia cases is increased transmission of the P. jirovecii organism between susceptible persons. Levels of exposure of susceptible persons to infectious persons might be increased as a result of changes in the delivery of health care. New, more transmissible strains could be emerging and leading to increased spread in the health care environment. Further investigation into the contribution of outbreaks—and, thus, increased person-to-person transmission—to the increase is warranted.
As a result of increased awareness of P. jirovecii infection, other infections might be clinically misdiagnosed as P. jirovecii infection. In the HES database, some patients might have been incorrectly coded as having P. jirovecii pneumonia, thereby resulting in a misclassification bias, but we have no reason to suspect that this coding would have changed over time. The death statistics should also be interpreted with caution because the cause of death and contributory causes are probably not recorded consistently. The analyses did not differentiate between outbreaks and sporadic cases of disease because this information could not be reliably determined from the data sources used. Although the most recent data might be subject to reporting delays, such delays would result in underestimation rather than overestimation of recent cases.
Next Steps
Incidence of P. jirovecii pneumonia has increased across all groups of immunosuppressed patients known to be at risk for this infection (excluding HIV patients) and in new groups not previously known to be at risk. To determine whether current indications for prophylaxis need to be widened, enhanced surveillance should be introduced to help characterize any additional groups of patients for whom prophylaxis is not currently recommended but who might be at risk. Particular focus should be given to patients with chronic lung disease, systemic inflammatory diseases, and solid tumors and to transplant recipients who do not currently fulfill the criteria for prophylaxis. When introducing new immunosuppressive agents and regimens, consideration should be given as to whether these agents might increase the patients’ risk for P. jirovecii pneumonia.
More studies involving sequencing of P. jirovecii clinical isolates identified by PCR, coupled with national surveillance, should be used to better understand transmission dynamics and thereby inform infection control policies and clarify the role of any environmental factors (1,30–32). More basic knowledge of the biology, pathogenesis, virulence factors, and the contribution of different strains will be crucial for explaining observed changes in P. jirovecii epidemiology.
To ensure adherence to current guidelines and to ensure that preventive prophylaxis is optimal for all groups at risk for this potentially life-threatening infection, auditing of prescribing practices for patients known to be at risk is warranted. Raising awareness among clinicians could also help ensure that prophylaxis is correctly used.
In conclusion, data from a variety of national sources demonstrate an increase in the number of cases of P. jirovecii in non–HIV-infected persons. P. jirovecii infections are largely preventable by use of inexpensive drugs. The current case numbers are taking a substantial toll on health care costs and human health. Further investigation leading to improved preventive strategies for this largely preventable infection is warranted.
Dr Maini is a specialist registrar in public health and works at the Health Protection Agency, London, UK. Her research interests are focused on communicable diseases, especially respiratory infections.
Acknowledgments
We thank Nick Andrews and Phil Pocock for their statistical advice. We also thank the Office for National Statistics for access to death registrations and note that they bear no responsibility for our analysis or interpretation of data supplied by them.
HES data, copyright 2012, were reused with permission from The Health and Social Care Information Centre. All rights are reserved.
References
- Thomas S, Vivancos R, Corless C, Wood G, Beeching NJ, Beadsworth MB. Increasing frequency of Pneumocystis jirovecii pneumonia in renal transplant recipients in the United Kingdom: clonal variability, clusters, and geographic location. Clin Infect Dis. 2011;53:307–8. DOIPubMedGoogle Scholar
- Haverkos HW, Curran JW. The current outbreak of Kaposi's sarcoma and opportunistic infections. CA Cancer J Clin. 1982;32:330–9. DOIPubMedGoogle Scholar
- Morris A, Beard CB, Huang L. Update on the epidemiology and transmission of Pneumocystis carinii. Microbes Infect. 2002;4:95–103. DOIPubMedGoogle Scholar
- Vargas SL, Hughes WT, Santolaya ME, Ulloa AV, Ponce CA, Cabrera CE, Search for primary infection by Pneumocystis carinii in a cohort of normal, healthy infants. Clin Infect Dis. 2001;32:855–61. DOIPubMedGoogle Scholar
- Wakefield AE. Detection of DNA sequences identical to Pneumocystis carinii in samples of ambient air. J Eukaryot Microbiol. 1994;41:116S .PubMedGoogle Scholar
- Roblot F, Godet C, Le Moal G, Garo B, Faouzi Souala M, Dary M, Analysis of underlying diseases and prognosis factors associated with Pneumocystis carinii pneumonia in immunocompromised HIV-negative patients. Eur J Clin Microbiol Infect Dis. 2002;21:523–31. DOIPubMedGoogle Scholar
- Yale SH, Limper AH. Pneumocystis pneumonia in patients without acquired immunodeficiency syndrome: associated illness and prior corticosteroid therapy. Mayo Clin Proc. 1996;71:5–13. DOIPubMedGoogle Scholar
- Kovacs JA, Hiemenz JW, Macher AM. Pneumocystis carinii pneumonia: a comparison between patients with the acquired immunodeficiency syndrome and patients with other immunodeficiencies. Ann Intern Med. 1984;100:663–71 .PubMedGoogle Scholar
- Klippstein A, Schneider CP, Sayer HG, Höffken K. Pneumocystis carinii pneumonia as a complication of bendamustine monotherapy in a patient with advanced progressive breast cancer. J Cancer Res Clin Oncol. 2003;129:316–9 .PubMedGoogle Scholar
- Eitner F, Hauser IA, Rettkowski O, Rath T, Lopau K, Pliquett RU, Risk factors for Pneumocystis jiroveci pneumonia (PCP) in renal transplant recipients. Nephrol Dial Transplant. 2011;26:2013–7. DOIPubMedGoogle Scholar
- Radisic M, Lattes R, Chapman JF, del Carmen Rial M, Guardia O, Seu F, Risk factors for Pneumocystis carinii pneumonia in kidney transplant recipients: a case–control study. Transpl Infect Dis. 2003;5:84–93. DOIPubMedGoogle Scholar
- Lahiff C, Khiaron OB, Nolan N, Chadwick GA. Pneumocystis carinii pneumonia in a patient on etanercept for psoriatic arthritis. Ir J Med Sci. 2007;176:309–11. DOIPubMedGoogle Scholar
- Nelson M, Dockrell D, Edwards S; BHIVA Guidelines Subcommittee. Angus B, Barton S, et al. British HIV Association and British Infection Association guidelines for the treatment of opportunistic infection in HIV-seropositive individuals. HIV Med. 2011;12:1–140.
- Palella FJ Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853–60. DOIPubMedGoogle Scholar
- Sepkowitz KA, Brown AE, Armstrong D. Pneumocystis carinii pneumonia without acquired immunodeficiency syndrome: more patients, same risk. Arch Intern Med. 1995;155:1125–8. DOIPubMedGoogle Scholar
- Hughes WT, Price RA, Kim HK, Coburn TP, Grigsby D, Feldman S. Pneumocystis carinii pneumonitis in children with malignancies. J Pediatr. 1973;82:404–15. DOIPubMedGoogle Scholar
- Pagano L, Caira M, Fianchi L. Pulmonary fungal infection with yeasts and pneumocystis in patients with hematological malignancy. Ann Med. 2005;37:259–69. DOIPubMedGoogle Scholar
- Godeau B, Coutant-Perronne V, Le Thi Huong D, Guillevin L, Magadur G, De Bandt M, Pneumocystis carinii pneumonia in the course of connective tissue disease: report of 34 cases. J Rheumatol. 1994;21:246–51 .PubMedGoogle Scholar
- Wollner A, Mohle-Boetani J, Lambert ER, Perruquet JL, Thomas A. Pneumocystis carinii pneumonia complicating low dose methotrexate treatment for rheumatoid arthritis. Thorax. 1991;46:205–7. DOIPubMedGoogle Scholar
- Health Protection Agency. United Kingdom new HIV diagnoses to end of June 2011 [cited 2012 Feb 2]. http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1237970242135
- StataCorp. Stata Statistical Software: release 11. College Station, TX: StataCorp LP; 2009.
- Gallant JE, McAvinue SM, Moore RD, Bartlett JG, Stanton DL, Chaisson RE. The impact of prophylaxis on outcome and resource utilization in Pneumocystis carinii pneumonia. Chest. 1995;107:1018–23. DOIPubMedGoogle Scholar
- Leigh TR, Gazzard B, Rowbottom A, Collins J. Quantitative and qualitative comparison of DNA amplification by PCR with immunofluorescence staining for diagnosis of Pneumocystis carinii pneumonia. J Clin Pathol. 1993;46:140–4. DOIPubMedGoogle Scholar
- Office for National Statistics. Cancer statistics registrations, England (Series MB1) No. 41, 2010 [cited 2011 Aug 26]. http://www.ons.gov.uk/ons/dcp171778_267154.pdf
- European Best Practices Guidelines Expert Group on Renal Transplantation. European best practice guidelines for renal transplantation. Section IV: long-term management of the transplant recipient. IV.7.1 Late infections. Pneumocystis carinii pneumonia. Nephrol Dial Transplant. 2002;17:36–9. DOIPubMedGoogle Scholar
- Kidney Disease; Improving Global Outcomes (KDIGO) Transplant Work Group. KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant. 2009;9(Suppl 3):S1–155. DOIPubMedGoogle Scholar
- Worth LJ, Dooley MJ, Seymour JF, Mileshkin L, Slavin MA, Thursky KA. An analysis of the utilization of chemoprophylaxis against Pneumocystis jirovecii pneumonia in patients with malignancy receiving corticosteroid therapy at a cancer hospital. Br J Cancer. 2005;92:867–72. DOIPubMedGoogle Scholar
- Central South Coast Cancer Network. Guidelines for the management of haematological malignancies. March 2010 [cited 2011 Aug 26]. http://www.csccn.nhs.uk/uploads/networkgrp/20101102104803-Network-Haematological-Malignancy-Guidelines-2010.pdf
- Green H, Paul M, Vidal L, Leibovici L. Prophylaxis for Pneumocystis pneumonia (PCP) in non-HIV immunocompromised patients (review) [cited 2013 Jan 7]. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD005590.pub2/pdf/standard
- Wynckel A, Toubas D, Noël N, Toupance O, Rieu P. Outbreak of Pneumocystis pneumonia occurring in late post-transplantation period. Nephrol Dial Transplant. 2011;26:2417. DOIPubMedGoogle Scholar
- Phipps LM, Chen SC, Kable K, Halliday CL, Firacative C, Meyer W, Nosocomial Pneumocystis jirovecii pneumonia: lessons from a cluster in kidney transplant recipients. Transplantation. 2011;92:1327–34. DOIPubMedGoogle Scholar
- de Boer MG, de Fijter JW, Kroon FP. Outbreaks and clustering of Pneumocystis pneumonia in kidney transplant recipients: a systematic review. Med Mycol. 2011;49:673–80 .PubMedGoogle Scholar
Figures
Tables
Follow Up
Earning CME Credit
To obtain credit, you should first read the journal article. After reading the article, you should be able to answer the following, related, multiple-choice questions. To complete the questions (with a minimum 70% passing score) and earn continuing medical education (CME) credit, please go to www.medscape.org/journal/eid. Credit cannot be obtained for tests completed on paper, although you may use the worksheet below to keep a record of your answers. You must be a registered user on Medscape.org. If you are not registered on Medscape.org, please click on the New Users: Free Registration link on the left hand side of the website to register. Only one answer is correct for each question. Once you successfully answer all post-test questions you will be able to view and/or print your certificate. For questions regarding the content of this activity, contact the accredited provider, CME@medscape.net. For technical assistance, contact CME@webmd.net. American Medical Association’s Physician’s Recognition Award (AMA PRA) credits are accepted in the US as evidence of participation in CME activities. For further information on this award, please refer to http://www.ama-assn.org/ama/pub/category/2922.html. The AMA has determined that physicians not licensed in the US who participate in this CME activity are eligible for AMA PRA Category 1 Credits™. Through agreements that the AMA has made with agencies in some countries, AMA PRA credit may be acceptable as evidence of participation in CME activities. If you are not licensed in the US, please complete the questions online, print the certificate and present it to your national medical association for review.
Article Title:
Increasing Pneumocystis Pneumonia, England, UK, 2000–2010
CME Questions
1. You are a public health official consulting with the World Health Organization regarding trends in Pneumocystis jirovecii pneumonia in England over the past decade. Based on findings from the database study by Dr. Maini and colleagues, which of the following statements about changes in incidence of P. jirovecii pneumonia in England from 2000–2010 would be most likely to appear in your report?
A. Between 2000 and 2010, laboratory-confirmed cases increased by an average of 3% per year
B. Between 2000 and 2010, death registrations increased by an average of 2% per year
C. Between 2000 and 2010, Hospital Episode Statistics (HES) cases increased by an average of 9% per year
D. Most of the increase in HES cases occurred in the first half of the decade
2. Based on findings from the database study by Dr. Maini and colleagues, which of the following statements about changes in risk factors associated with P. jirovecii pneumonia in England from 2000–2010 is most likely correct?
A. Rates of P. jirovecii pneumonia in adults with diagnosed HIV infection increased from 2000-2010
B. Patients with pre-existing renal disease were identified as a new risk group
C. The largest proportion of cases was patients who had undergone transplantation
D. A total of 17.5% of cases were associated with pre-existing lung disease
3. Which of the following statements about the clinical and public health implications of findings from the database study by Dr. Maini and colleagues is most likely correct?
A. The diagnosis of potentially preventable P. jirovecii pneumonia in non-HIV infected persons did not increase during the study period.
B. Earlier diagnosis of HIV was the only potential explanation for the significant reduction during the study period in P. jirovecii pneumonia infection among HIV-infected persons
C. There is no reason to suspect that P. jirovecii pneumonia ascertainment increased over the study period
D. The findings support enhanced P. jirovecii pneumonia surveillance for patients with chronic lung disease, systemic inflammatory diseases, and solid tumors
Activity Evaluation
|
1. The activity supported the learning objectives. |
||||
|
Strongly Disagree |
|
|
|
Strongly Agree |
|
1 |
2 |
3 |
4 |
5 |
|
2. The material was organized clearly for learning to occur. |
||||
|
Strongly Disagree |
|
|
|
Strongly Agree |
|
1 |
2 |
3 |
4 |
5 |
|
3. The content learned from this activity will impact my practice. |
||||
|
Strongly Disagree |
|
|
|
Strongly Agree |
|
1 |
2 |
3 |
4 |
5 |
|
4. The activity was presented objectively and free of commercial bias. |
||||
|
Strongly Disagree |
|
|
|
Strongly Agree |
|
1 |
2 |
3 |
4 |
5 |
Related Links
Table of Contents – Volume 19, Number 3—March 2013
| EID Search Options |
|---|
|
|
|
|
|
|


Please use the form below to submit correspondence to the authors or contact them at the following address:
Katherine L. Henderson, Health Protection Agency, 61 Colindale Ave, London, NW9 5EQ, UK
Top