Volume 22, Number 1—January 2016
Dispatch
Outbreak of Panton-Valentine Leukocidin–Associated Methicillin-Susceptible Staphylococcus aureus Infection in a Rugby Team, France, 2010–2011
Cite This Article
Citation for Media
Abstract
Staphylococcus aureus strains that produce Panton-Valentine leukocidin are known to cause community infections. We describe an outbreak of skin abscesses caused by Panton-Valentine leukocidin–producing methicillin-susceptible S. aureus (clonal complex 121) in a professional rugby team in France during July 2010–February 2011. Eight team members were carriers; 7 had skin abscesses.
Staphylococcus aureus is a leading cause of community and healthcare-associated infections, notably skin and soft-tissue infections (1). A strong epidemiologic link exists between community-associated S. aureus and Panton-Valentine leukocidin (PVL), a cytotoxin found particularly in deep primary skin infections (2). The prevalence of community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) cases seems to be low but increasing in Europe; however, heterogeneity in prevalence rates among countries occurs (3). Many sporadic cases and outbreaks of CA-MRSA infection have been reported in sports teams (4), especially among players having regular skin-to-skin contact. We describe an outbreak of recurrent PVL-positive community-associated methicillin-susceptible Staphylococcus aureus (MSSA) skin abscesses in a professional rugby team in France.
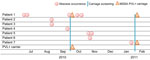
On September 22, 2010, a player (patient 4) was hospitalized for a calf abscess that had spontaneously drained to the skin. Bacterial culture grew PVL-positive MSSA. Investigations identified 3 previous case-patients among the team members during the previous month (Figure). A case-patient was defined as a player on the team who developed a skin abscess. The abscesses began occurring after recruitment of a new player from Fiji (patient 1), who had untreated axillary and back abscesses when he arrived on the team in July 2010. All other case-patients had contact with him during scrimmages, suggesting that cross-transmission occurred by close physical contact. In August 2010, abscesses developed on the left wrist of patient 2 and on the arm of patient 3 (Figure).
On September 28, 2010, we screened all team members for PVL-positive S. aureus carriage. The team had 51 men, including 30 permanent team members; mean age was 23.6 (range 17–42) years. Screening consisted of nasal, throat, and skin-lesion swabbing. S. aureus was detected by bacterial culture. Gene-encoding PVL was tested by real-time PCR (5). DNA microarray analysis was performed by the French National Reference Center for Staphylococcal Infections (Lyon, France) and enabled detection of the mecA gene and genes encoding various toxins and also assisted in agr typing and multilocus sequence typing.
The first round of screening showed that 35 (68.6%) of the 51 team members were colonized with MSSA, and 2 (patient 1 and a player who never developed an abscess) harbored PVL-encoding genes (Figure). During the screening process, patient 1 was found to have a PVL-positive MSSA left knee abscess that spontaneously drained to the skin but was not covered.
To reduce risk of transmission, we implemented a 5-day course of S. aureus decontamination for all team members; decontamination consisted of mupirocin 2% nasal ointment twice daily and showering with chlorhexidine soap. We also provided information about standard hygiene measures: showering and handwashing; washing jerseys after play; regularly cleaning and disinfecting showers and shared sports equipment; avoiding sharing of personal items; protecting and disinfecting skin lesions; and treating abscesses early and appropriately. Team staff regularly checked players’ adherence to the control measures. Despite these measures, 3 new skin abscesses developed in October 2010 on the chest and nape of patient 1 (Figure; isolates not available). In early November 2010, abscesses developed on the axillary and thigh of patient 5 and on the right wrist (sample not obtained) of patient 6. In January 2011, a thigh abscess developed on patient 7. On February 2, 2011, we conducted a second round of S. aureus carriage screening and a 10-day course of S. aureus decontamination for 8 players, focusing on previous PVL-positive MSSA carriers and those with abscesses. The screening showed that patients 1 and 7 carried PVL-positive MSSA. All team members were again reminded of basic hygiene measures. These infection control measures were successful: no further person-to-person transmission occurred.
Overall, 8 (15.6%) of the 51 players carried PVL-positive MSSA (n = 3) or had abscesses (n = 7); 2 players had both. All strains isolated in patients 1–7 belonged to clonal complex (CC) 121 and harbored agr4 allele. One player who never had an abscess carried a different PVL-positive MSSA strain in his throat (agr1, sequence type 152). All isolated PVL-positive MSSA strains were susceptible to all antimicrobial drugs tested except penicillin G. Except for the first 2 abscesses in patient 1, all abscesses were treated with synergistin A and B (2 grams/day for 7 days) and local disinfection.
Using a standardized questionnaire to interview the 51 rugby players, a member of the Hygiene unit at the Limoges Teaching Hospital collected epidemiologic data on demographics, sport practices, sport hygiene, and occurrence of hospitalization or abscess during the previous year. The interviews highlighted poor hygiene practices: 49% of players shared personal items, and fewer than half disinfected or protected skin lesions (Table). Occurrence of abscess during the previous year was the only significant (p = 0.00028, Fisher exact test) risk factor found for a PVL-positive MSSA carriage or abscess; however, given the context of this abscess outbreak, this factor was considered a bias, not a general characteristic.
Skin and soft-tissue infections are common in athletes, and the most common bacterial pathogen responsible for outbreaks is CA-MRSA, particularly the USA300 clone. The strain in the outbreak we investigated was unrelated to USA300 but belonged to CC121. Outbreaks of PVL-positive MSSA skin infections have been described in families in Italy (6), schoolchildren in Switzerland (7), French soldiers in Côte d'Ivoire (8), and prison inmates in France (9) . As in this outbreak among rugby players, infection control measures and S. aureus decontamination successfully interrupted transmission in most published outbreaks.
In our study, abscess occurred in 4 players despite a round of decontamination strategies. This failure was likely because of an uncovered, untreated knee abscess in the index case-patient (patient 1) during the decontamination period. The continued occurrence of infections highlights the necessity of strict application of hygiene measures.
Nasal carriage of PVL-positive MSSA was not systematically linked to infection (e.g., 1 team member carried a PVL-positive strain in his throat but had no active skin infection). Concordance of skin and soft-tissue infection and nasal carriage is reportedly lower in MSSA than MRSA strains (10). Following France’s guidelines for grouped cases of community-associated S. aureus infections (http://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=453), we decontaminated all athletes, even those team members not carrying PVL-positive MSSA. Decontamination temporarily reduces risk of colonization of noncarriers. Along with reinforcement of simple personal hygiene measures, our decontamination regimen sufficiently halted transmission without needing to exclude players with abscesses from the team, an important factor in professional sports.
The outbreak strain was agr4, PVL positive, and CC121. It belonged to a PVL-positive MSSA lineage that predominated in France during 1981–1990 (11). The CC121 agr4 lineage was also linked to furunculosis in a study in Poland (12). Like the strain in our study, this lineage carried no exfoliative toxin genes and expressed the seb superantigen. However, the strain circulating among the rugby team players was positive for seg, sei, sem, sen, seo, and seu. Superficial, deep-skin, and soft-tissue infections linked to CC121, PVL-positive MSSA strains have been reported worldwide (13). Similar strains have also been reported in highly lethal community-acquired pneumonia and in severe sepsis with progressive and metastatic soft-tissue infections (14,15).
We investigated an outbreak of skin abscesses caused by a PVL-producing MSSA strain and cross-transmitted through physical contact among players of a professional rugby team. A 10-day period of S. aureus decontamination combined with reinforcement of hygiene education and practices successfully interrupted person-to-person transmission and enabled control of the outbreak.
Dr. Couvé-Deacon is a physician and microbiologist who works in the Hygiene Unit of the Microbiology-Virology-Hygiene Laboratory of Limoges Teaching Hospital. Her research interests include multidrug-resistant bacteria and understanding the transmission of antibiotic resistance.
Acknowledgment
We thank Michèle Bes and François Vandenesch for their contribution in strain analysis.
References
- Iwatsuki K, Yamasaki O, Morizane S, Oono T. Staphylococcal cutaneous infections: invasion, evasion and aggression. J Dermatol Sci. 2006;42:203–14. DOIPubMedGoogle Scholar
- Lina G, Piémont Y, Godail-Gamot F, Bes M, Peter MO, Gauduchon V, Involvement of Panton-Valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin Infect Dis. 1999;29:1128–32. DOIPubMedGoogle Scholar
- Otter JA, French GL. Molecular epidemiology of community-associated methicillin-resistant Staphylococcus aureus in Europe. Lancet Infect Dis. 2010;10:227–39. DOIPubMedGoogle Scholar
- Cohen PR. The skin in the gym: a comprehensive review of the cutaneous manifestations of community-acquired methicillin-resistant Staphylococcus aureus infection in athletes. Clin Dermatol. 2008;26:16–26. DOIPubMedGoogle Scholar
- Jarraud S, Mougel C, Thioulouse J, Lina G, Meugnier H, Forey F, Relationships between Staphylococcus aureus genetic background, virulence factors, agr groups (alleles), and human disease. Infect Immun. 2002;70:631–41. DOIPubMedGoogle Scholar
- Tinelli M, Monaco M, Vimercati M, Ceraminiello A, Pantosti A. Methicillin-susceptible Staphylococcus aureus in skin and soft tissue infections, Northern Italy. Emerg Infect Dis. 2009;15:250–7. DOIPubMedGoogle Scholar
- Boubaker K, Diebold P, Blanc DS, Vandenesch F, Praz G, Dupuis G, Panton-Valentine leukocidin and Staphyloccoccal skin infections in schoolchildren. Emerg Infect Dis. 2004;10:121–4. DOIPubMedGoogle Scholar
- Lesens O, Haus-Cheymol R, Dubrous P, Verret C, Spiegel A, Bonnet R, Methicillin-susceptible, doxycycline-resistant Staphylococcus aureus, Côte d’Ivoire. Emerg Infect Dis. 2007;13:488–90. DOIPubMedGoogle Scholar
- Bourigault C, Corvec S, Brulet V, Robert P-Y, Mounoury O, Goubin C, Outbreak of skin infections due to Panton-Valentine leukocidin–positive methicillin-susceptible Staphylococcus aureus in a French prison in 2010–2011. PLoS Curr. 2014;6. file:///\\\\\\\\Cdc.gov\\\\project\\\\CCID_NCPDCID_DEISS_EIDJ\\\\EID%20Production\\\\Editorial\\\\Vol22No01\\\\%20PubMedGoogle Scholar
- Ellis MW, Schlett CD, Millar EV, Crawford KB, Cui T, Lanier JB, Prevalence of nasal colonization and strain concordance in patients with community-associated Staphylococcus aureus skin and soft-tissue infections. Infect Control Hosp Epidemiol. 2014;35:1251–6.DOIPubMedGoogle Scholar
- Rasigade J-P, Laurent F, Lina G, Meugnier H, Bes M, Vandenesch F, Global distribution and evolution of Panton-Valentine leukocidin–positive methicillin-susceptible Staphylococcus aureus, 1981–2007. J Infect Dis. 2010;201:1589–97. DOIPubMedGoogle Scholar
- Masiuk H, Kopron K, Grumann D, Goerke C, Kolata J, Jursa-Kulesza J, Association of recurrent furunculosis with Panton-Valentine leukocidin and the genetic background of Staphylococcus aureus. J Clin Microbiol. 2010;48:1527–35. DOIPubMedGoogle Scholar
- Kurt K, Rasigade J-P, Laurent F, Goering RV, Žemličková H, Machova I, Subpopulations of Staphylococcus aureus clonal complex 121 are associated with distinct clinical entities. PLoS ONE. 2013;8:e58155. DOIPubMedGoogle Scholar
- Baranovich T, Zaraket H, Shabana II, Nevzorova V, Turcutyuicov V, Suzuki H. Molecular characterization and susceptibility of methicillin-resistant and methicillin-susceptible Staphylococcus aureus isolates from hospitals and the community in Vladivostok, Russia. Clin Microbiol Infect. 2010;16:575–82. DOIPubMedGoogle Scholar
- Schefold JC, Esposito F, Storm C, Heuck D, Krüger A, Jörres A, Therapy-refractory Panton Valentine leukocidin–positive community-acquired methicillin-sensitive Staphylococcus aureus sepsis with progressive metastatic soft tissue infection: a case report. J Med Case Rep. 2007;1:165. DOIPubMedGoogle Scholar
Figure
Table
Cite This ArticleTable of Contents – Volume 22, Number 1—January 2016
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Marie-Cécile Ploy, Laboratoire de Bactériologie-Virologie–Hygiène, Centre Hospitalier Universitaire Dupuytren, 2 Avenue Martin Luther King, 87042 Limoges CEDEX, France
Top