Volume 22, Number 2—February 2016
Dispatch
Ebola Virus RNA Stability in Human Blood and Urine in West Africa’s Environmental Conditions
Cite This Article
Citation for Media
Abstract
We evaluated RNA stability of Ebola virus in EDTA blood and urine samples collected from infected patients and stored in West Africa’s environmental conditions. In blood, RNA was stable for at least 18 days when initial cycle threshold values were <30, but in urine, RNA degradation occurred more quickly.
Real-time reverse transcription PCR (rRT-PCR) has become the standard diagnostic tool for patients infected by Ebola virus (EBOV) (1,2). Control of the current outbreak and proper management of patients cannot be achieved without laboratory testing. In the field in West Africa and notably in Guinea, most Ebola treatment units are located near (often in the same compound) a laboratory that can process collected samples within hours. However, most healthcare centers or dispensaries lack this diagnostic capability and cannot ensure rapid testing of samples from patients suspected of having Ebola.
Few laboratory studies have investigated Ebola virus RNA stability over time in collected samples. The period of stability has been estimated to be 5–14 days for virus suspensions on solid surfaces kept in darkness or for virus-spiked human blood or naturally infected, nonhuman primate blood stored under simulated tropical conditions (3–5). A recently published study found that viral RNA was consistently detectable in blood of cynomolgus macaques until 3 weeks after euthanasia (6). According to an anecdotal report, Ebola virus was isolated in blood samples stored for a month at room temperature (P.E. Rollin, pers. comm.). Such reports of sample stability must be considered for organizing collection and movement of samples in the field. In addition, quantification (copies/mL) or cycle threshold (Ct) determination of EBOV RNA for estimating viral load has been shown to be a major prognosis marker in affected patients (1,7,8). Ct value, which can be used to perform RNA semiquantification, is not an absolute quantification, which necessitates use of a calibration curve. Moreover, Ct value does not reflect viral viability but only presence of RNA in samples. By using Ct determination, we attempted to assess the stability of EBOV RNA in EDTA plasma (widely used in the field) and in urine from infected patients in the environmental conditions (i.e., air temperature and humidity) of West Africa.
Our study was conducted in the Laboratory of the Centre de Traitement des Soignants in Conakry, Guinea, during the Ebola outbreak in Guinea during January–March 2015. Establishing a Biosafety Level 4 (BSL-4) laboratory in Guinea was not possible. To enable biologists to work safely, a BSL-3 laboratory with a class-3 biologic-safety cabinet and single-use personal protective equipment were used (9).
We measured EBOV RNA stability in blood and urine samples from 7 case-patients with laboratory-confirmed Ebola. Twelve blood samples from the 7 case-patients were obtained by venipuncture by using Vacutainer tubes containing EDTA (BD Vacutainer; Becton Dickinson, Franklin Lakes, NJ, USA). Thirteen urine samples from the 7 case-patients were collected in individual sterile receptacles (BD Vacutainer Urine Collection Cup; Becton Dickinson).
Samples were immediately transferred to the laboratory. Upon arrival, samples were processed by centrifugation (at 4,000 rpm for 15 min) and stored at room temperature (22°C–29°C; 50%–80% humidity) for 18–30 days in a BSL-3 laboratory. At regular intervals (i.e., generally every other day), viral RNA was extracted from 100 μL of undiluted initial plasma or urine (QIAmp Viral RNA Mini Kit; QIAGEN, Valencia, CA, USA). To manage the limited volume of initial sample, our protocol used 100 μL of sample, less than manufacturer’s recommendations of 140 μL. We therefore modified the volume of lysis buffer (Buffer AVL; QIAGEN) to 400 μL to maintain the manufacturer’s recommended ratio of 1:4. We performed 40 cycles of rRT-PCR tests for detecting EBOV by using a commercially available kit (RealStar Filovirus Screen RT-PCR Kit 1.0; Altona Diagnostic GmbHh, Hamburg, Germany) (10). Results were expressed as Ct values, which are inversely proportional to the quantity of viral RNA in samples.
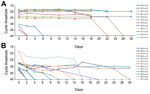
For each sample, extraction control and amplification of the positive control gave expected values; no inhibition of amplification occurred. At admission, all 7 case-patients had blood Ct values <30.0 (mean 21.0, 95% CI 19.5–22.5). For the 12 blood samples studied (Figure, panel A), Ct values ranged from 18.3 to 35.0. When the initial Ct value was <30.0, Ct values were stable for up to 18 days after collection (day 0 mean 20.95, 95% CI 19.1–22.7; day 18 mean 21.9, 95% CI 19.9–23.8). For 2 samples with initial Ct values of 24.0 and 25.0, RNA was undetectable by days 28 and 22, respectively. For 3 samples collected from convalescent patients with Ct values ranging from 30.0 to 32.0, RNA was detected until day 4. For samples with Ct >32.0, RNA was detected on the initial test only.
In the 13 urine samples (Figure, panel B), initial Ct values had a range of 18.2–35.5 (mean 28.6, 95% CI 25.7–31.5). RNA in urine was undetectable by days 10 and 14 for initial Ct counts of 19.0 and 18.0, respectively. For equivalent Ct values for blood, RNA was detectable for at least 18 days.
For urine samples with initial Ct values >30.0, rRT-PCR results were negative within 2–4 days. However, urine results were inconsistent; 3 urine samples from the same patient had initial Ct values of 27.0–28.0 and were detectable for 24–30 days.
These results from human samples taken during the Ebola outbreak in Guinea are similar to reported data for postmortem samples from cynomolgus macaques; for those samples, RNA was detectable for a few weeks after death (6). Our results indicate that EBOV RNA is stable in EDTA plasma samples collected and tested in the environmental conditions of West Africa. In the early phase of Ebola disease, blood sampling is probably more sensitive and reliable than oral swabbing and should be used whenever possible (11,12). Plasma samples can be tested for up to 18 days after collection, even if stored at ambient temperature, and positive results can still be reported. However, negative results may be false negative (in case of samples with low viral load) and should be reported as invalid; retesting should be performed on a new blood sample.
Urine does not seem useful for initial diagnosis of Ebola disease. Even if collection is easy, detectable viral RNA appears in the urine of infected patients at a later stage of the disease than in blood, and Ct values are higher (13,14). The presence of protease, RNase, or bacteria and the absence of proteins that stabilize the virus and RNA in urine may explain the rapid degradation of viral RNA and thus the limited usefulness of this type of biologic sample.
This study is subject to limitations. First, our analysis was performed with samples that were centrifuged (i.e., plasma), according to manufacturer’s instructions and our laboratory protocol. No analysis was performed with noncentrifuged blood. For samples collected in facilities with no laboratory nearby, centrifugation before transport would not be possible and stability of viral RNA in these samples could have slightly different results than those found in this study. In such scenarios, for accurate comparisons of the stability of viral RNA over time, all tests would need to be performed on noncentrifuged blood, not on plasma. Second, the limited volume of collected samples did not enable us to perform tests in duplicate or at a frequency of every other day for 30 days for every sample.
Our study was performed in real conditions (i.e., with samples from infected patients during the Ebola outbreak in Guinea in an Ebola treatment center laboratory there) and shows that EBOV RNA is stable in EDTA plasma. The development of practices for safe collection in the field and transport within a few hours or days to a local or national reference laboratory equipped with rRT-PCR capabilities seems feasible and will offer a more sustainable strategy for laboratory diagnosis and surveillance during and after the current outbreak.
Dr. Janvier is a physician and clinical biologist with a master’s degree in molecular microbiology. He works at the Hôpital d’Instruction des Armées Sainte-Anne, Toulon, France, and was in charge of the molecular laboratory at the Centre de Traitement des Soignants, Conakry, Guinea, for 3 months during the Ebola virus outbreak. His research interests include medical virology and bacteriology.
Acknowledgments
We thank Julie Top, Lucie Queval, Cécile Vigier, and Sophie Gorbatch for laboratory support.
This study was supported by the French Military Health Service.
References
- Towner JS, Rollin PE, Bausch DG, Sanchez A, Crary SM, Vincent M, Rapid diagnosis of Ebola haemorrhagic fever by reverse transcription-PCR in an outbreak setting and assessment of patient viral load as a predictor of outcome. J Virol. 2004;78:4330–41. DOIPubMedGoogle Scholar
- Leroy EM, Baize S, Lu CY, McCormick JB, Georges AJ, Georges-Courbot MC, Diagnosis of Ebola haemorrhagic fever by RT-PCR in an epidemic setting. J Med Virol. 2000;60:463–7. DOIPubMedGoogle Scholar
- Sagripanti JL, Rom AM, Holland LE. Persistence in darkness of virulent alphaviruses, Ebola virus, and Lassa virus deposited on solid surfaces. Arch Virol. 2010;155:2035–9. DOIPubMedGoogle Scholar
- Sagripanti JL, Lytle CD. Sensitivity to ultraviolet radiation of Lassa, vaccinia, and Ebola viruses dried on surfaces. Arch Virol. 2011;156:489–94. DOIPubMedGoogle Scholar
- Fischer R, Judson S, Miazgowicz K, Bushmaker T, Prescott J, Munster VJ. Ebola virus stability on surfaces and in fluids in simulated outbreak environments. Emerg Infect Dis. 2015;21:1243–6. DOIPubMedGoogle Scholar
- Prescott J, Bushmaker T, Fischer R, Miazgowicz K, Judson S, Munster VJ. Postmortem stability of Ebola virus. Emerg Infect Dis. 2015;21:856–9. DOIPubMedGoogle Scholar
- Schieffelin JS, Shaffer JG, Goba A, Gbakie M, Gire SK, Colubri A, Clinical illness and outcomes in patients with Ebola in Sierra Leone. N Engl J Med. 2014;371:2092–100. DOIPubMedGoogle Scholar
- Hunt L, Gupta-Wright A, Simms V, Tamba F, Knott V, Tamba K, Clinical presentation, biochemical, and hematological parameters and their association with outcome in patients with Ebola virus disease: an observational cohort study. Lancet Infect Dis. 2015;15:1292–9. DOIPubMedGoogle Scholar
- Janvier F, Foissaud V, Delaune D, Flusin O, Dubrous P, Mac Nab C, Deployment of the French military laboratory dedicated to Ebola virus infected patients in Guinea, January 2015 to July 2015. J Infect Dis. In press 2015.
- Janvier F, Gorbatch S, Queval L, Top J, Vigier C, Foissaud V. Difficulties of interpretation of Zaire Ebola virus PCR results and implication in the field. J Clin Virol. 2015;67:36–7. DOIPubMedGoogle Scholar
- Grolla A, Jones SM, Fernando L, Strong JE, Ströher U, Möller P, The use of a mobile laboratory unit in support of patient management and epidemiological surveillance during the 2005 Marburg outbreak in Angola. PLoS Negl Trop Dis. 2011;5:e1183. DOIPubMedGoogle Scholar
- Spengler JR, Chakrabarti AK, Coleman-McCray JD, Martin BE, Nichol ST, Spiropoulou CF, Utility of oral sampling for Ebola virus detection in guinea pig model. Emerg Infect Dis. 2015;21:1816–9. DOIPubMedGoogle Scholar
- Kreuels B. Wichmann D, Emmerich P, Schmidt-Chanasit J, de Heer G, Kluge S, et al. A case of severe Ebola virus infection complicated by gram-negative septicemia. N Engl J Med. 2014;371:2394–401. DOIPubMedGoogle Scholar
- Lyon GM, Mehta AK, Varkey JB, Brantly K, Plyler L, McElroy AK, Emory Serious Communicable Diseases Unit. Clinical care of two patients with Ebola virus disease in the United States. N Engl J Med. 2014;371:2402–9. DOIPubMedGoogle Scholar
Figure
Cite This ArticleTable of Contents – Volume 22, Number 2—February 2016
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Frédéric Janvier, Sainte Anne Military Teaching Hospital Laboratory, 2 Blvd Sainte-Anne, BP 20545, 83041 Toulon CEDEX 09, France
Top