Volume 22, Number 4—April 2016
Research
Quantifying Transmission of Clostridium difficile within and outside Healthcare Settings
Figure 2
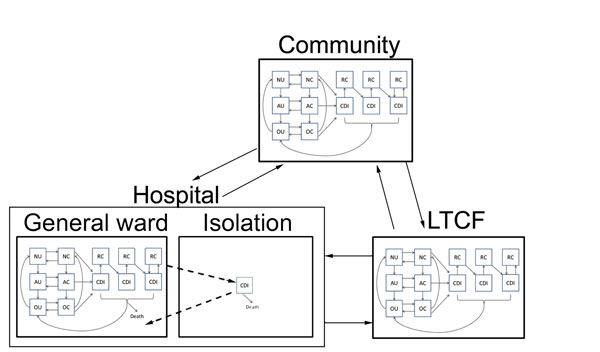
Figure 2. Transitions between settings (hospital, LTCF, and the non–healthcare community) for model structure of Clostridium difficile infection (CDI). Transitions were parameterized at demographically calibrated, age-specific rates. Hospitalized patients with CDI who were given a diagnosis are subject to enhanced isolation protocols that reduce transmission. All hospitalized CDI patients are discharged at a slower rate than non–CDI patients, which reflects longer hospitalization attributable to CDI. N, patients not receiving antimicrobial drugs; A, patients receiving antimicrobial drugs; O, patients with a recent history of receiving antimicrobial drugs; U, uncolonized patients; C, asymptomatically colonized patients; RC, symptomatically infected patients or colonized patients and subject to recurrence; LTCF, long-term care facility. Solid arrows indicate changes in individual epidemiologic status and patient movement between the hospital, community, and LTCF. Dashed arrows indicate isolation of CDI patients.