Volume 24, Number 5—May 2018
Research Letter
Fatal Tick-Borne Encephalitis Virus Infections Caused by Siberian and European Subtypes, Finland, 2015
Figure
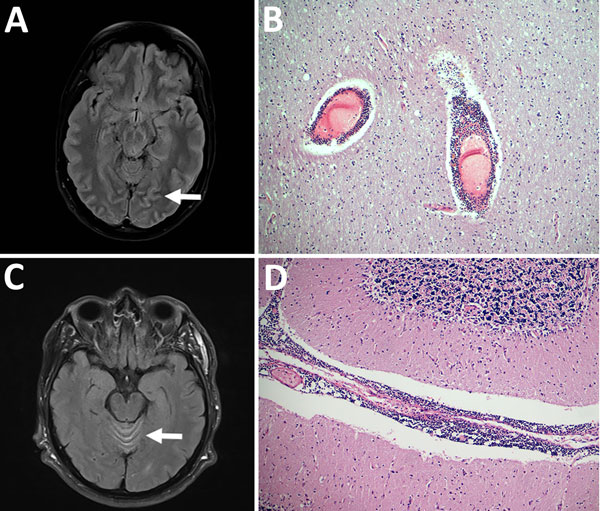
Figure. Pathologic and virologic findings for 2 patients with tick-borne encephalitis, Finland, 2015. A) Magnetic resonance images of 36-year-old woman (patient 1) with pathologically increased signal in cortical sulcus regions indicative of viral meningeal process (arrow). B) Hematoxylin and eosin staining of the frontal cortex of patient 1 showed inflammation throughout the central nervous system from the spinal cord to the cortex and cerebellum; original magnification ×100. C) Magnetic resonance image of 66-year-old man (patient 2), showing increased signal in facial nerves, cortical sulci, radicular regions, and cerebellar vermis (arrow). D) Hematoxylin and eosin staining showed microscopically abundant perivascular lymphocytosis in the cerebellum of patient 2; original magnification ×100.