Volume 26, Number 11—November 2020
Dispatch
Two New Cases of Pulmonary Infection by Mycobacterium shigaense, Japan
Figure 1
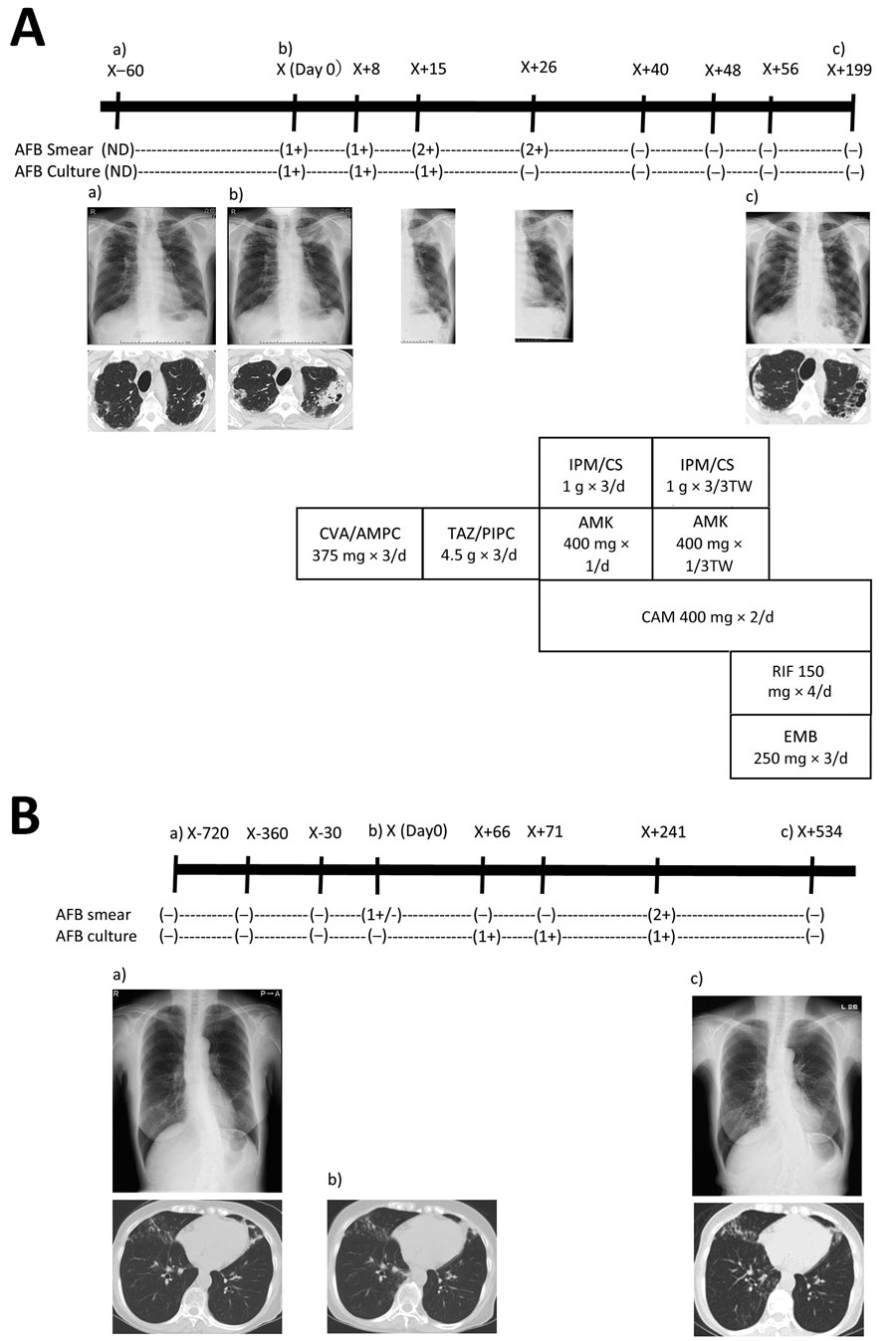
Figure 1. Radiographic and therapeutic drug monitoring for 2 patients with pulmonary disease caused by Mycobacterium shigaense. Each panel shows the timeline at the top (X, initial hospitalization period for M. shigaense disease) with smear results and chest radiograph (top) and chest CT (bottom) images below. The chemotherapy regimen is provided (Appendix). A) Case 1, patient with FC-type disease. a) Chest radiograph shows abnormal nodular shadows and a small calcification in the right upper and middle lung fields on day 60 before initial hospitalization. b) Chest radiograph taken 2 months later showed a more indistinct bilateral contour of the lung; there was increased consolidation of a cavitary lesion in the right upper lobe and a centrilobular nodule with branching in the left upper lobe on transverse chest CT. Lesions including progressive cavities are shown in the right upper and middle lung fields. c) Chest CT shows reduction in cavities and consolidation in the left lobe on day 199. B) Case 2, patient with NB-type disease. a) Chest CT showed a small nodular shadow in the right lower lung field. Image showed bronchiectasis in the left middle lobe and the lingular segment of the right upper lobe. There was peribronchiectasic consolidation and multiple small nodules suggesting bronchiolitis in both lungs. b) After 24 months, chest CT showed a stable extent of scattered small nodules including bronchiectasis just beneath the pleura and pleural thickening in the right middle lobe. c) Chest CT showed bronchiectasis in the right middle lobe. According to the number of AFB seen by Ziehl-Neelsen method for acid-fast staining, smear results were classified as 3+, 2+, 1+, or ±. –, negative; +, positive. AFB, acid-fast bacilli; AFB culture result –, culture negative; +, culture positive. AMK, amikacin; CAM, clarithromycin; CVA/AMPC, clavulanic acid/amoxicillin; CT, computed tomography; EMB, ethambutol; FC, fibrocavitary; IPM/CS, imipenem/cilastatin; NB, nodular bronchiectasis; ND, no data; RIF, rifampin; TAZ/PIPC, tazobactam/piperacillin.
1These authors contributed equally to this article.