Volume 26, Number 8—August 2020
CME ACTIVITY - Research
Sporadic Creutzfeldt-Jakob Disease among Physicians, Germany, 1993–2018
Introduction

Medscape CME ACTIVITY
In support of improving patient care, this activity has been planned and implemented by Medscape, LLC and Emerging Infectious Diseases. Medscape, LLC is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1.00 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.0 MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) program. Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider's responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 75% minimum passing score and complete the evaluation at http://www.medscape.org/journal/eid; and (4) view/print certificate.
Release date: July 15, 2020; Expiration date: July 15, 2021
Learning Objectives
Upon completion of this activity, participants will be able to:
• Assess the occurrence of sporadic Creutzfeldt-Jakob disease (sCJD) among physicians in Germany from 1993 to 2018, according to an analysis of occupational data for patients with sCJD in Germany
• Evaluate risk factors for sCJD among physicians in Germany from 1993 to 2018, according to an analysis of occupational data for patients with sCJD in Germany
• Determine the clinical implications of the occurrence of sCJD among physicians in Germany from 1993 to 2018, according to an analysis of occupational data for patients with sCJD in Germany
CME Editor
Karen L. Foster, Technical Writer/Editor, Emerging Infectious Diseases. Disclosure: Karen L. Foster has disclosed no relevant financial relationships.
CME Author
Laurie Barclay, MD, freelance writer and reviewer, Medscape, LLC. Disclosure: Laurie Barclay, MD, has disclosed no relevant financial relationships.
Authors
Disclosures: Peter Hermann, MD; Johannes Treig, MD; Steffen Unkel, PhD; Stefan Goebel, MD; Timothy Bunck, MD; Martha Jünemann, BA; Tim Friede, PhD; and Inga Zerr, MD, have disclosed no relevant financial relationships.
Abstract
We investigated sporadic Creutzfeldt-Jakob disease (sCJD) among physicians in Germany by analyzing occupational information of patients with sCJD recorded by the German CJD Surveillance Unit (1993–2005; 1,250 patients, of whom 4 [0.32%] were physicians) and the National Reference Center for Human Spongiform Encephalopathies (2006–2016; 1,491 patients, of whom 13 [0.87%] were physicians). Among the physicians, we did not identify any neurologists, neurosurgeons, psychiatrists, or pathologists. A cumulative sum test showed an increase in reported physicians over time. Data for 2017–2018 indicated an increased rate of physicians among all notified sCJD cases (5/239 [2.1%]) when we used the total population of Germany as control group. Our data suggest the possibility of an increased risk for sCJD among physicians in Germany. However, we can only speculate about the reasons, and larger multinational studies are needed to replicate the finding and to clarify whether this finding is a general or a country-specific phenomenon.
Creutzfeldt-Jakob disease (CJD) is a syndrome comprising dementia and various neurologic signs and symptoms (1) caused by the transmissible misfolded prion protein scrapie (2). Reported death rates and incidence rates differ from 1.67 (3) to >2 per million person-years (4,5). In contrast to animal prion diseases (6,7), transmitted human prion diseases are uncommon. Variant CJD (vCJD) caused by ingestion of beef is rare (231 cases worldwide) (8), and its incidence has decreased since 2000 (9). Most cases of human prion disease are sporadic CJD (sCJD; 84%–93%), followed by genetic CJD (5%–10%). Only <4% are considered to be iatrogenic (iCJD) (3,10–12). Clinical diagnostic criteria of iCJD imply the presence of an iatrogenic risk factor (13). Known cases were caused by cadaver-derived growth hormones, dura mater grafts, neurosurgical instrument contamination, and corneal grafts (12). On the other hand, iCJD might be overlooked when no classic risk factor is present. Neuropathologic characteristics can identify iCJD only in a subgroup of cases (14,15). Unrecorded cases related to surgery are likely because an increased risk for sCJD in persons with a history of surgery was reported (16); however, data on this issue remain ambiguous (17). vCJD transmitted by transfusion of blood products has been reported (8), but no confirmed case was recorded among recipients of blood from donors with sCJD (18–20).
An increased risk for iCJD among caregivers and healthcare professionals has been suggested, but its evaluation is complex (21–24). Previous studies neither unequivocally displayed nor ruled out relevant increases in risk for CJD among healthcare professionals (25,26). Furthermore, these investigations were mostly designed as case–control studies, which are prone to bias because of case selection. Therefore, we aimed to evaluate sCJD among physicians using historical epidemiologic data from 25 years of CJD surveillance in Germany and the whole population of that country as controls.
Study Design and Data Acquisition
In the framework of a retrospective cohort study, we evaluated 4,645 patient files representing all suspected CJD cases reported to the German surveillance group during June 1993–December 2016 about the patient’s occupational history to identify physicians of all specialties. In addition and as negative controls, we collected information about other professions.
The centralized assessment of suspected human prion diseases in Germany started in June 1993 and was conducted by the CJD Surveillance Unit of the University Medical Center Goettingen. Since January 2006, health authorities have officially charged this center with CJD surveillance and named it the National Reference Center for Human Transmissible Spongiform Encephalopathies (NRZ-TSE). In Germany, notification of sCJD is required. Health authorities advise clinical institutions to contact the NRZ-TSE for clinical classifications of notified cases. The NRZ-TSE counsels physicians with respect to differential diagnosis and hygienic issues and records clinical data, including the patient’s professional background. Specifically, until 2006, physicians from the CJD Surveillance Unit visited and interviewed patients and caregivers using a standardized questionnaire.
Patient Cohorts
We considered all patients in the database for this study. Inclusion criteria for further analyses were diagnosis of probable or definite sCJD according to World Health Organization criteria (2) and age >35 years. We reviewed all available questionnaires (evaluated by the NRZ-TSE) and medical reports (sent to the NRZ-TSE by treating institution) since 1993 for patient’s professions to identify physicians. During 1993–2005, the research group of the University Medical Center Goettingen had to actively search for suspected CJD cases (e.g., through regular newsletters to all neurologic and psychiatric centers in Germany). Most reported patients had been visited by physicians from the research group, and epidemiologic questionnaires were available for analyses. In 2006, the group was assigned as National Reference Center, leading to a substantial increase in reported cases and resulted in a decrease in the proportion of visitations and interviews. Because of these structural differences, we divided the study cohort into cohort A (reported 1993–2005; 1,250 persons) and cohort B (reported 2006–2016; 1,491 persons) and analyzed them separately.
Population-Based Cohorts
We used publicly available data on the population of Germany to create control groups in each time frame (matching cohorts A and B). Numbers of working and retired physicians were sourced from the database of the German Federal Medical Association (Bundesärztekammer [BÄK], Berlin, Germany), which provides the number of physicians and information about age, sex, specialty, and location. Membership is required for, but is not restricted to, all working physicians and does not expire with retirement. To analyze the entire population, we obtained numbers from the German Federal Office of Statistics.
Data Analyses and Statistical Methods
BÄK data give numbers of physicians in Germany in different age categories. The youngest category was <35 years of age (without further differentiation). Only 10 patients in the sCJD cohort were <35 years of age, and none were physicians. We included only patients and controls >35 years of age to achieve approximate age matching between the German physicians and the sCJD cohort. We did not further stratify for age (and sex) because of the low case count among physicians with sCJD. We pooled all data from our sources using Excel 2016 (Microsoft, https://www.microsoft.com). We used Statistica (https://www.statsoft.de) for descriptive analyses and performed further statistical analyses using the statistical software R version 3.4.2 (https://www.r-project.org). We considered results with p<0.05 to be significant.
The aims of the study were to evaluate the rate of physicians in the cohort of CJD patients and to investigate a potential risk modification using population-based data. The aims had been framed before data collection. We used Fisher exact test to compare the number of physicians in the cohort of CJD patients and the number of physicians in the population of Germany.
Analyses were performed as follows. To define the number of nonphysicians in the CJD cohort, we considered only patients with known occupation. These analyses were based on the assumption of a corresponding number of physicians in the group of patients with unknown occupation. We further considered all CJD patients assuming that no additional physicians were in the group of patients with unknown occupation. We used the results to perform sensitivity analyses to evaluate the number of physicians in the group of patients with unknown occupation that would be necessary to reach statistical significance using Fisher exact test. We conducted a CUSUM (cumulative sum)–based test for a change point in a time series (27) to investigate alterations of the number of reported physicians with CJD over time (per year). Finally, in an additional step, we collected data from 2017 and 2018 and analyzed them to validate results of the previous analyses on the basis of the historical cohorts (1993–2016).
Descriptive Data Analyses: CJD Cohort
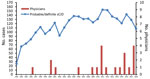
Of 4,645 suspected CJD cases during June 1993–December 2016, we classified 2,754 as probable sCJD (1,543) or definite sCJD (1,211). We classified other cases as possible sCJD (2) (156 cases), non-CJD (1,188), genetic prion disease (197), and iCJD (12). A total of 338 reported cases remained unclassified because of incomplete clinical information. We reduced the number of probable and definite sCJD cases to 2,741 after excluding patients <35 years of age. We determined occupation for 1,532 (55.9%) patients, of whom 17 (1.1%) were physicians (Figures 1, 2).
In cohort A (June 1993–December 2005), we classified 539 (43%) of the 1,250 cases as probable sCJD and 711 (57%) as definite sCJD. In cohort B (January 2006–December 2016), we classified 1,000 (67%) of the 1,491 cases as probable sCJD and 491 (33%) as definite sCJD. The mean age of cohort A patients was 66 years (range 35–90 years) and of cohort B patients was 68 years (range 37–93 years). In cohort A, 58% of patients were women; in cohort B, 52%. Information about codon 129 polymorphism was available for 1,039 (83%) cohort A cases and 581 (39%) for cohort B cases (Table 1). For 1,532 (56% in cohorts A and B combined) patients, we were able to evaluate history of occupation before illness (cohort A, 1,093 patients; cohort B, 439). For some patients, >2 different professions were recorded (up to 7). We considered occupation as a physician at any point in time. Occupation as a physician was known for 4 cohort A patients (0.3% of all patients; 0.4% of cohort A patients) and 13 cohort B patients (0.9% of all patients; 3% of cohort B patients).
Physicians with sCJD (including patients from the validation cohort 2017–2018) had a broad spectrum of medical specialties. Surgical specialties were present for 14 patients (surgery without information about further specialty, 3 patients; trauma/orthopedic surgery, 5; gynecology and otolangyrology, 2 each; urology and visceral surgery, 1 each). The others had nonsurgical specialties (internal medicine, 5; anesthesiology, podiatry, and general practice, 1 each). Of all physicians with sCJD (1993–2018), 64% had a surgical specialty (Table 2); in 2018, only 31% of all physicians in German had a surgical specialty (28). Very long duration of disease occurred only among physicians with surgical specialties (mean 205 days vs. 109 days for nonsurgical specialties; overall 175 days [range 49–809 days]). We identified no hospital in Germany that had employed >1 physician with sCJD, but a complete occupational history was not available for all patients, especially in cohort B. We found no link between a physician and another known sCJD patient, but only limited information was available (Appendix Table). Most patients were not able to give detailed information about this issue because of progressed cognitive impairment. The rate of autopsy-confirmed cases was 55%. Prion typing was performed in only 4 cases.
Descriptive Data Analyses: Population-Based Cohort
The number of physicians in Germany increased from 297,803 in 1993 to 496,240 in 2016 (29), a factor of 1.67. For each period corresponding to cohort A (1993–2005) and cohort B (2006–2016), mean values of yearly numbers were calculated that excluded physicians <35 years of age. Mean numbers were 295,556 (range 240,709–345,599) during 1993–2005 and 382,558 (range 349,878–416,311) during 2006–2016. We performed the same calculations considering the entire population of the same age in Germany (30): mean 47,907,927 (range 44,336,444–51,243,273) during 1993–2005 and 51,601,356 (range 51,553,192–51,961,175) during 2006–2016.
Rate of Physicians in sCJD Cohorts and in the Total Population of Germany
We based contingency tables on the numbers of all patients in the study cohort for whom occupation was known (cohort A, 1,093 patients; cohort B, 439 patients), all physicians in the sCJD cohort (cohort A, 4 patients; cohort B, 13 patients), the population of Germany, and all physicians in that population (Table 3). Fisher exact test yielded an odds ratio (OR) of 0.59 (95% CI 0.16–1.52; p = 0.44) for cohort A and OR 4.09 (95% CI 2.16–7.06; p<0.001) for cohort B (Table 3). These results indicate a significantly higher rate of physicians in cohort B than in the total population of Germany.
We based this approach on the assumption of a corresponding proportion of physicians and nonphysicians in the group of sCJD patients without known occupational history. In a second step, we included the entire study cohort, assuming there were no additional physicians in the group of sCJD patients for whom occupational history was not known. Cohort A did not differ significantly from the total population of Germany (OR 0.52 [95% CI 0.14–1.33]; p = 0.27); likewise, cohort B did not differ significantly from the total population of Germany (OR 1.18 [95% CI 0.63–2.02]; p = 0.54). Subsequently, we conducted a sensitivity analysis to determine the number of physicians in the group without known occupation who would be required for a statistically significant difference between the study cohort and the total German population: 9 for cohort A (p = 0.03) and 5 for cohort B (p = 0.047). In a forth step, we investigated the change of the rate of reported physicians in the study cohort over time: 0.32% for cohort A (1993–2005) and 0.87% for cohort B. Results of our CUSUM test showed an increase of reported cases (p = 0.04) and identified a change point from 2008 to 2009.
Postanalytic Evaluation of 2017 and 2018
In 2017 and 2018, a total of 239 sCJD patients were reported (129 in 2017, 110 in 2018). We identified 5 physicians (1 in 2017, 4 in 2018) (Figure 2). Including the entire postanalytic cohort (sCJD patients 2017–2018), regardless of known occupational history and using population data from 2017 (29,30), excluding patients <35 years of age, we found a significantly elevated rate of physicians among sCJD patients (OR 2.61 [95% CI 1.08–6.34]; p = 0.05 by Fisher exact test) (Table 3).
Although prion diseases are transmissible, homozygosity for methionine at codon 129 (an intrinsic factor) is the only established risk factor for sCJD (11,31). Case–control studies have shown slightly elevated ORs for several features; for example, work at an animal laboratory, ophthalmologic surgery (32), ingestion of raw meat and brain (24), and history of brain surgery (33) (Table 4). Being employed as health professionals was a risk in a meta-analysis of case–control studies (34) but was not confirmed in a later prospective study (23). Because of the methodologic approaches used, most results were nonsignificant or prone to biases (17,43). Only 1 study used large population-based data from a US death registry (6 million cases screened, 636 CJD cases and 3,180 controls selected) and identified working as a butcher and work in physicians’ offices as occupational risk factors (35). Other investigations of occupational risk factors for sCJD are not available, but the presence of unpublished data that might show inconclusive or null results cannot be excluded. Data on the development of reported cases over time with respect to occupational history are not available.
In addition to selection bias, the lack of studies that could validate occupational risk factors for sCJD might be caused by multiple comparisons of too many variables causing insignificant results. For this study, we focused on the evaluation of employment as physician as potential risk factor for sCJD. We used data from a prospective epidemiologic surveillance database in Germany and population-based data as controls.
Our first analysis showed a significantly elevated rate of physicians in the study cohort (OR 4.09; p<0.001) during 2006–2016 (cohort B), the years in which structured epidemiologic surveillance had been conducted. The exclusion of patients with unknown occupational history represents a case–control design limited by the possibility of selection bias. An occupation as physician may be more likely to be reported than others; on the other hand, only clinical data relevant for case classification were available for many patients from cohort B. The study design for cohort A was more precise because most suspected patients were examined in person in notifying hospitals, whereas for cohort B, only a proportion of sCJD patients (27%) were examined.
Nonetheless, our second analysis of the entire CJD population and found no significant results (OR 0.53 [p = 0.27] for cohort A; OR 1.18 [p = 0.543] for cohort B). Therefore, we performed a sensitivity analysis indicating 5 additional physicians in the group with unknown occupational history (1,052 [71%]) in cohort B who would be necessary for a significant result. This number was higher in cohort A (9 patients), although the number of patients in cohort A with unknown occupation was much smaller (157 [13%]). These findings suggest that the number of reported physicians with sCJD increased in later years, whereas the reported number of sCJD cases was stable. We validated this finding with a CUSUM test (p = 0.04, change point from 2008 to 2009). During 2017–2018, the increased rate of sCJD in physicians was significant, even when we included all 239 reported cases in the analysis (OR 2.61; p = 0.05).
Fourteen of the 22 physicians were surgeons, but none had worked in neurosurgery and only 1 had worked in a neuropathology department for 1 year. This finding is remarkable because the high proportion of surgeons (64%) versus nonsurgeons (36%) in the sCJD group differs from the population control (39% vs. 61%). The apparent differences of clinical characteristics (age of onset, disease duration) might be explained by slightly different distribution of codon 129 genotypes in the 2 groups. Because of the low number of cases, we could not investigate these observations further. In most cases, information about genotype, prion type, and neuropathologic characteristics was insufficient to identify or exclude iCJD. No neurologists or psychiatrists were reported. We could not find regional links within the group of physicians or with other sCJD patients who had received surgical interventions and might have been index patients for obscure iCJD. Thus, we were not able to establish a causal relation between the statistical risk factor (occupation as a physician) and the disease. Nonetheless, this finding must be interpreted with regard to potential incubation times of up to 30 years (10) and incomplete information about residence history in most patients from cohort B.
Although the use of a very large cohort of patients with sCJD and a population-based control group is a strength of our investigation, the study has several limitations. Because of the low number of physicians with sCJD, every bias in the case group would cause an immense effect on statistical analyses (e.g., unrecorded cases, misdiagnosed cases). Thus, we must interpret our results cautiously. Definite (neuropathologic) diagnosis was available only for some cases in our study, but the high accuracy of clinical diagnoses performed by our center has been reported previously (5). The altered status of the surveillance group after it was named a National Reference Center in 2006 might be a source of bias. We cannot exclude that the surveillance system in Germany has improved over the years, but the available data of patients’ occupations has decreased in recent years (Table 1), which makes an underestimation of the number of physicians before 2006 highly unlikely. An increased awareness for CJD among German physicians resulting in more reported cases in recent years is also unlikely regarding the decreasing worldwide incidence of vCJD since 2000.
Another limitation of our study is the lack of further and more detailed statistical analyses. We could not calculate individual ORs for certain medical specialties. Only an extremely large-scale study pooling data from multiple national reference centers would be capable of doing that. In addition, we were not able to stratify ORs by age and sex. The age cutoff of >35 years was an attempt only to achieve an approximate matching of age in the case and the control groups. On the other hand, recorded physicians with sCJD showed a strong tendency to be male and have an age at onset of 60–75 years. In this context, unstratified analyses might underestimate ORs. Another limitation of the study is that we analyzed only 1 occupational risk factor. Other professionals, such as laboratory scientists or nurses, should be carefully considered, but the lack of data (especially population-based figures) prevented from further analyses.
The high proportion of physicians among patients with sCJD and its increase over the last years were displayed in a statistical model based on data from the population of Germany. We showed that sCJD patients were significantly more likely than the general population to be physicians, suggesting that it might be an occupational risk factor. Previous epidemiologic studies have not clearly identified an elevated risk for sCJD among physicians (Table 4), but the most recent available data are from 2010. Our study yielded significant results only after 2005, and the CUSUM test identified an increased number of physicians with sCJD after 2008. No specialties involved specifically in treating patients with CJD have been reported. Nonetheless, we found that a high proportion of physicians with sCJD were surgeons, although we can only speculate about the reasons. A larger study comprising new data from other countries is needed to clarify whether this finding is a general or a country-specific phenomenon.
Dr. Hermann is is a study physician in the NRZ-TSE at the University Medical Center Göttingen. His research interests are diagnostic testing and epidemiology of prion diseases as well as biomarkers of atypical dementia.
Acknowledgments
We thank physicians throughout Germany for case notification and provision of clinical data to the NRZ-TSE and CJD Surveillance Unit.
This study was funded by the Robert Koch Institute through funds from the Federal Ministry of Health (grant no. 1369–341).
References
- Prusiner SB. Novel proteinaceous infectious particles cause scrapie. Science. 1982;216:136–44. DOIPubMedGoogle Scholar
- Zerr I, Kallenberg K, Summers DM, Romero C, Taratuto A, Heinemann U, et al. Updated clinical diagnostic criteria for sporadic Creutzfeldt-Jakob disease. [Erratum in: Brain. 2012;135] [Pt 4]. Brain. 2009;132:2659–68. DOIPubMedGoogle Scholar
- Ladogana A, Puopolo M, Croes EA, Budka H, Jarius C, Collins S, et al. Mortality from Creutzfeldt-Jakob disease and related disorders in Europe, Australia, and Canada. Neurology. 2005;64:1586–91. DOIPubMedGoogle Scholar
- Glatzel M, Rogivue C, Ghani A, Streffer JR, Amsler L, Aguzzi A. Incidence of Creutzfeldt-Jakob disease in Switzerland. Lancet. 2002;360:139–41. DOIPubMedGoogle Scholar
- Hermann P, Laux M, Glatzel M, Matschke J, Knipper T, Goebel S, et al. Validation and utilization of amended diagnostic criteria in Creutzfeldt-Jakob disease surveillance. Neurology. 2018;91:e331–8. DOIPubMedGoogle Scholar
- Colby DW, Prusiner SB. Prions. Cold Spring Harb Perspect Biol. 2011;3:
a006833 . DOIPubMedGoogle Scholar - Imran M, Mahmood S. An overview of animal prion diseases. Virol J. 2011;8:493. DOIPubMedGoogle Scholar
- The National CJD Research & Surveillance Unit. Current data on variant CJD cases worldwide [cited 2019 Aug 8]. http://www.cjd.ed.ac.uk/sites/default/files/worldfigs.pdf
- Andrews NJ, Farrington CP, Ward HJT, Cousens SN, Smith PG, Molesworth AM, et al. Deaths from variant Creutzfeldt-Jakob disease in the UK. Lancet. 2003;361:751–2. DOIPubMedGoogle Scholar
- Brown P, Preece M, Brandel JP, Sato T, McShane L, Zerr I, et al. Iatrogenic Creutzfeldt-Jakob disease at the millennium. Neurology. 2000;55:1075–81. DOIPubMedGoogle Scholar
- Heinemann U, Krasnianski A, Meissner B, Varges D, Kallenberg K, Schulz-Schaeffer WJ, et al. Creutzfeldt-Jakob disease in Germany: a prospective 12-year surveillance. Brain. 2007;130:1350–9. DOIPubMedGoogle Scholar
- Brown P, Brandel J-P, Sato T, Nakamura Y, MacKenzie J, Will RG, et al. Iatrogenic Creutzfeldt-Jakob disease, final assessment. Emerg Infect Dis. 2012;18:901–7. DOIPubMedGoogle Scholar
- World Health Organization. Global surveillance, diagnosis and therapy of human transmissible spongiform encephalopathies: report of a WHO consultation, Geneva, Switzerland. 1998 Feb 9–11 [cited 2019 Aug 8]. https://apps.who.int/iris/handle/10665/65516
- Kobayashi A, Parchi P, Yamada M, Mohri S, Kitamoto T. Neuropathological and biochemical criteria to identify acquired Creutzfeldt-Jakob disease among presumed sporadic cases. Neuropathology. 2016;36:305–10. DOIPubMedGoogle Scholar
- Takeuchi A, Kobayashi A, Parchi P, Yamada M, Morita M, Uno S, et al. Distinctive properties of plaque-type dura mater graft-associated Creutzfeldt-Jakob disease in cell-protein misfolding cyclic amplification. Lab Invest. 2016;96:581–7. DOIPubMedGoogle Scholar
- Ward HJ, Everington D, Cousens SN, Smith-Bathgate B, Gillies M, Murray K, et al. Risk factors for sporadic Creutzfeldt-Jakob disease. Ann Neurol. 2008;63:347–54. DOIPubMedGoogle Scholar
- López FJG, Ruiz-Tovar M, Almazán-Isla J, Alcalde-Cabero E, Calero M, de Pedro-Cuesta J. Risk of transmission of sporadic Creutzfeldt-Jakob disease by surgical procedures: systematic reviews and quality of evidence. Euro Surveill. 2017;22:16–00806. DOIPubMedGoogle Scholar
- Puopolo M, Ladogana A, Vetrugno V, Pocchiari M. Transmission of sporadic Creutzfeldt-Jakob disease by blood transfusion: risk factor or possible biases. Transfusion. 2011;51:1556–66. DOIPubMedGoogle Scholar
- Urwin PJ, Mackenzie JM, Llewelyn CA, Will RG, Hewitt PE. Creutzfeldt-Jakob disease and blood transfusion: updated results of the UK Transfusion Medicine Epidemiology Review Study. Vox Sang. 2016;110:310–6. DOIPubMedGoogle Scholar
- Crowder LA, Schonberger LB, Dodd RY, Steele WR. Creutzfeldt-Jakob disease lookback study: 21 years of surveillance for transfusion transmission risk. Transfusion. 2017;57:1875–8. DOIPubMedGoogle Scholar
- Brown P, Cervenáková L, McShane L, Goldfarb LG, Bishop K, Bastian F, et al. Creutzfeldt-Jakob disease in a husband and wife. Neurology. 1998;50:684–8. DOIPubMedGoogle Scholar
- Rudge P, Jaunmuktane Z, Adlard P, Bjurstrom N, Caine D, Lowe J, et al. Iatrogenic CJD due to pituitary-derived growth hormone with genetically determined incubation times of up to 40 years. Brain. 2015;138(Pt 11):3386–99, 20, 21, 22.
- de Pedro-Cuesta J, Glatzel M, Almazán J, Stoeck K, Mellina V, Puopolo M, et al. Human transmissible spongiform encephalopathies in eleven countries: diagnostic pattern across time, 1993-2002. BMC Public Health. 2006;6:278. DOIPubMedGoogle Scholar
- van Duijn CM, Delasnerie-Lauprêtre N, Masullo C, Zerr I, de Silva R, Wientjens DP, et al. Case-control study of risk factors of Creutzfeldt-Jakob disease in Europe during 1993-95. European Union (EU) Collaborative Study Group of Creutzfeldt-Jakob disease (CJD). Lancet. 1998;351:1081–5. DOIPubMedGoogle Scholar
- Alcalde-Cabero E, Almazan-Isla J, Brandel JP, Breithaupt M, Catarino J, Collins S, et al. Health professions and risk of sporadic Creutzfeldt-Jakob disease, 1965 to 2010. Euro Surveill. 2012;17:20144.PubMedGoogle Scholar
- Bradford BM, Piccardo P, Ironside JW, Mabbott NA. Human prion diseases and the risk of their transmission during anatomical dissection. Clin Anat. 2014;27:821–32. DOIPubMedGoogle Scholar
- Worsley KJ. The power of likelihood ratio and cumulative sum tests for a change in a binomial probability. Biometrika. 1983;70:455–64. DOIGoogle Scholar
- Bundesärztekammer (BÄK). Ärztinnen und Ärzte mit Schwerpunktbezeichnung, BÄK. 2019 [cited 2019 Dec 2]. http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=3&p_aid=66737473&nummer=614&p_sprache=D&p_indsp=99999999&p_aid=29100768
- Bundesärztekammer (BÄK). Ärztinnen und Ärzte mit Gebiets- und Facharztbezeichnung, BÄK. 2019 [cited 2019 Feb 27]. http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=i&p_aid=7768273&nummer=656&p_sprache=D&p_indsp=99999999&p_aid=70341618
- Statistisches Bundesamt (DESTATIS). Bevölkerung: Deutschland, Stichtag, Altersjahre. 2019 [cited 2019 Feb 27]. http://www-genesis.destatis.de/genesis/online/link/tabellen/12411*
- Parchi P, Giese A, Capellari S, Brown P, Schulz-Schaeffer W, Windl O, et al. Classification of sporadic Creutzfeldt-Jakob disease based on molecular and phenotypic analysis of 300 subjects. Ann Neurol. 1999;46:224–33. DOIPubMedGoogle Scholar
- Ruegger J, Stoeck K, Amsler L, Blaettler T, Zwahlen M, Aguzzi A, et al. A case-control study of sporadic Creutzfeldt-Jakob disease in Switzerland: analysis of potential risk factors with regard to an increased CJD incidence in the years 2001-2004. BMC Public Health. 2009;9:18. DOIPubMedGoogle Scholar
- Zerr I, Brandel JP, Masullo C, Wientjens D, de Silva R, Zeidler M, et al. European surveillance on Creutzfeldt-Jakob disease: a case-control study for medical risk factors. J Clin Epidemiol. 2000;53:747–54. DOIPubMedGoogle Scholar
- Wientjens DP, Davanipour Z, Hofman A, Kondo K, Matthews WB, Will RG, et al. Risk factors for Creutzfeldt-Jakob disease: a reanalysis of case-control studies. Neurology. 1996;46:1287–91. DOIPubMedGoogle Scholar
- Cocco PL, Caperna A, Vinci F. Occupational risk factors for the sporadic form of Creutzfeldt-Jakob disease. Med Lav. 2003;94:353–63.PubMedGoogle Scholar
- Schoene WC, Masters CL, Gibbs CJ Jr, Gajdusek DC, Tyler HR, Moore FD, et al. Transmissible spongiform encephalopathy (Creutzfeldt-Jakob disease). Atypical clinical and pathological findings. Arch Neurol. 1981;38:473–7. DOIPubMedGoogle Scholar
- Creutzfeldt-Jakob disease in histopathology technicians. N Engl J Med. 1988;318:853–4. DOIPubMedGoogle Scholar
- Creutzfeldt-Jakob disease in histopathology technicians. N Engl J Med. 1988;318:853–4. DOIPubMedGoogle Scholar
- Gorman DG, Benson DF, Vogel DG, Vinters HV. Creutzfeldt-Jakob disease in a pathologist. Neurology. 1992;42:463. DOIPubMedGoogle Scholar
- Berger JR, David NJ. Creutzfeldt-Jakob disease in a physician: a review of the disorder in health care workers. Neurology. 1993;43:205–6. DOIPubMedGoogle Scholar
- Weber T, Tumani H, Holdorff B, Collinge J, Palmer M, Kretzschmar HA, et al. Transmission of Creutzfeldt-Jakob disease by handling of dura mater. Lancet. 1993;341:123–4. DOIPubMedGoogle Scholar
- Mitrová E, Belay G. Creutzfeldt-Jakob disease in health professionals in Slovakia. Eur J Epidemiol. 2000;16:353–5. DOIPubMedGoogle Scholar
- de Pedro Cuesta J, Ruiz Tovar M, Ward H, Calero M, Smith A, Verduras CA, et al. Sensitivity to biases of case-control studies on medical procedures, particularly surgery and blood transfusion, and risk of Creutzfeldt-Jakob disease. Neuroepidemiology. 2012;39:1–18. DOIPubMedGoogle Scholar
Figures
Tables
Follow Up
Earning CME Credit
To obtain credit, you should first read the journal article. After reading the article, you should be able to answer the following, related, multiple-choice questions. To complete the questions (with a minimum 75% passing score) and earn continuing medical education (CME) credit, please go to http://www.medscape.org/journal/eid. Credit cannot be obtained for tests completed on paper, although you may use the worksheet below to keep a record of your answers.
You must be a registered user on http://www.medscape.org. If you are not registered on http://www.medscape.org, please click on the “Register” link on the right hand side of the website.
Only one answer is correct for each question. Once you successfully answer all post-test questions, you will be able to view and/or print your certificate. For questions regarding this activity, contact the accredited provider, CME@medscape.net. For technical assistance, contact CME@medscape.net. American Medical Association’s Physician’s Recognition Award (AMA PRA) credits are accepted in the US as evidence of participation in CME activities. For further information on this award, please go to https://www.ama-assn.org. The AMA has determined that physicians not licensed in the US who participate in this CME activity are eligible for AMA PRA Category 1 Credits™. Through agreements that the AMA has made with agencies in some countries, AMA PRA credit may be acceptable as evidence of participation in CME activities. If you are not licensed in the US, please complete the questions online, print the AMA PRA CME credit certificate, and present it to your national medical association for review.
Article Title:
Sporadic Creutzfeldt-Jakob Disease among Physicians, Germany, 1993–2018
CME Questions
1. Your patient is a 65-year-old male retired surgeon with early signs of dementia and ataxic gait. On the basis of the analysis of occupational data of patients with sporadic Creutzfeldt-Jakob disease (sCJD) in Germany by Hermann and colleagues, which one of the following statements about the occurrence of sCJD among physicians in Germany from 1993 to 2016 is correct?
A. The number of reported physicians with sCJD was 0.26% from 1993 to 2016
B. The rate of reported physicians with sCJD remained stable over time
C. In 2017 to 2018, physicians had a 2.6-fold increase for reported sCJD, using the total German population as a control group
D. Of probable/definite sCJD cases aged at least 35 years from June 1993 to December 2016 with occupational data, 0.5% were physicians
2. According to the analysis of occupational data of patients with sCJD in Germany by Hermann and colleagues, which one of the following statements about risk factors for sCJD among physicians in Germany from 1993 to 2018 is correct?
A. The rate of sCJD in 2017 to 2018 was higher among neurosurgeons than among other physicians
B. Of all physicians with sCJD from 1993 to 2018, 64% were surgeons, but in 2018, only 31% of physicians with sCJD were surgeons
C. Surgeons with sCJD were more likely to have short disease duration than nonsurgeon physicians with sCJD
D. A single hospital in Germany had a disproportionately high number of physicians with sCJD
3. On the basis of the analysis of occupational data of patients with sCJD in Germany by Hermann and colleagues, which one of the following statements about clinical implications of the occurrence of sCJD among physicians in Germany from 1993 to 2016 is correct?
A. Larger multinational studies are needed to confirm greater sCJD risk in German physicians in recent years and to clarify whether this is a general or a country-specific phenomenon
B. No risk factors for sCJD have previously been established
C. Results of previous studies all showed increased risk for sCJD in health professionals
D. Case-control studies have shown that orthopedic surgeons had slightly elevated risk for sCJD
Original Publication Date: July 15, 2020
1These authors contributed equally to this article.
Related Links
Table of Contents – Volume 26, Number 8—August 2020
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Peter Hermann, National Reference Center for TSE, Department of Neurology, University Medical Center Göttingen, Robert-Koch Strasse 40, 37075 Göttingen, Germany
Top