Volume 27, Number 10—October 2021
Dispatch
Rapid Increase in Lymphogranuloma Venereum among HIV-Negative Men Who Have Sex with Men, England, 2019
Cite This Article
Citation for Media
Abstract
Incidence of lymphogranuloma venereum increased in England during 2018–2019, after a period of decline. Our retrospective analysis of national surveillance data identified a rapid increase in diagnoses among HIV-negative men who have sex with men. These findings indicate a need for sustained surveillance and targeted public health action.
Lymphogranuloma venereum (LGV) is an invasive form of Chlamydia trachomatis infection. In high-income countries, LGV is concentrated among gay, bisexual, and other men who have sex with men (MSM) (1). Although LGM was initially characterized as affecting predominantly MSM living with HIV who have symptomatic proctitis (2,3), recent evidence suggests considerable underestimation of the actual extent of LGV among MSM in Europe because of insufficient testing of asymptomatic persons (4). Changes to UK guidelines (5) and testing practices of several large London clinics have led to expanded testing in MSM regardless of HIV status, leading to increased diagnoses among HIV-negative MSM and those without symptoms of proctitis (6–9). Expanded testing may have precipitated a decline in incidence during 2016–2018 (9); however, 2019 saw the highest number of LGV diagnoses reported in England since routine testing began in 2004, and test positivity increased from 8.2% in 2018 to 9.0% in 2019 (10). In this study, we investigated the changing epidemiology of LGV among MSM in England during 2015–2019 and risk factors associated with recent cases.
We conducted a retrospective analysis of adult (>16 years of age) MSM in England who visited sexual health service (SHS) sites during January 1, 2015–December 31, 2019. We obtained data from the Genitourinary Medicine Clinic Activity Dataset Sexually Transmitted Infection (STI) Surveillance System, which has recorded LGV diagnoses, obtained through multiplex reverse transcription PCR (4), since 2011. We included all SHS site visits by men who self-reported as MSM in England during 2015–2019. We cleaned and deduplicated data according to a routine practice described previously (11). We described the number of annual LGV diagnoses during 2015–2019 by age group, race (White [e.g., White British, White Irish, or White other background] and non-White), place of residence (London or rest of England), region of birth (United Kingdom, Europe, Asia, Oceania, Latin America and the Caribbean [LAC], North America, and Africa), history of a bacterial STI in the previous year (defined as having a recorded diagnoses of chlamydia, gonorrhea, or syphilis in the 365 days before attendance), and HIV status at time of LGV diagnosis. We used quarterly data on LGV diagnoses stratified by HIV status to examine changes over time in the proportion of diagnoses that were made among MSM who are HIV-negative or with unknown HIV status. We used generalized linear models with logarithmic function, Poisson distribution, and robust variances to identify the changes in risk for LGV in 2019 by quarter. We included covariates in the model if they showed strong association with an LGV diagnosis in the bivariate analyses (p<0.05). We adjusted the final model for HIV status, history of a previous bacterial STI, region of birth, and age group. We performed all data analyses using Stata 15.1 (https://www.stata.com).
Public Health England collects pseudonymized, electronic data on all STI tests and diagnoses from all commissioned SHS sites in England (11). Public Health England has approval to handle data obtained by the Genitourinary Medicine Clinic Activity Dataset STI Surveillance System under Regulation 3 of the Health Service (Control of Patient Information) Regulations 2002 (https://www.gov.uk/government/publications/hiv-and-sti-data-sharing-policy).
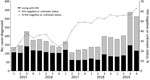
Of 2,116,345 SHS visits by MSM during 2015–2019, we identified 3,461 diagnoses of LGV (Table 1). The highest number of LGV diagnoses was recorded in 2019 (n = 1,018); this increase was mainly attributed to increases in diagnoses in the third and fourth quarter of the year (Figure 1). The proportion of diagnoses among MSM who are HIV-negative or with unknown HIV status increased from 31.4% in 2015 to 58.4% in 2019 (Table 1). In 2019, most LGV diagnoses in MSM were among White MSM (72.7%) and MSM residing in London (79.1%). A total of 614 (60.3%) LGV diagnoses in 2019 were made among those who had a bacterial STI diagnosis in the previous year (Table 1).
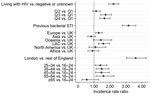
Our regression analyses included 526,102 visits and 1,018 LGV diagnoses among MSM in England in 2019 (Table 2). Compared with quarter 1 of 2019, the risk for having LGV diagnosed was 73% higher in quarter 3 and 66% higher in quarter 4. Living with HIV, residing in London, and having a previous bacterial STI were strongly associated with an LGV diagnosis in the crude and adjusted models (Table 2). Being born in LAC or in Europe outside of the UK were also associated with increased risk for LGV (Figure 2).
We show that a rapid increase occurred in LGV diagnoses in England in 2019, particularly affecting MSM who are HIV-negative or with unknown HIV status, such that nearly 60% of all LGV diagnoses are now in this group. This trend represents a major shift in the epidemiology of LGV; infection was previously associated with MSM living with HIV (2). However, having LGV diagnosed continues to be associated with living with HIV, as well as having a previous STI diagnosis, residing in London, and being born in LAC or Europe outside the United Kingdom.
An earlier decline in LGV diagnoses (9) has been attributed to revisions to LGV testing guidelines that led to expanded testing (5,12). However, because no revisions have been made since 2015, changes to testing practice are unlikely to explain the recent increase, which is concurrent with increases in test positivity (10). Of note, use of HIV preexposure prophylaxis (PrEP) in England may have contributed to increased testing for C. trachomatis and subsequent detection of LGV. Increased access to HIV prevention, including PrEP, in HIV-negative MSM engaging in high-risk sexual activities may have facilitated the change in the epidemiology of LGV and led to the observed increase in incidence among this group (13); the association with previous STI diagnosis further supports this hypothesis. Further investigation will be needed to understand the impact of HIV prevention on transmission of bacterial STIs. However, the increasing proportion of LGV diagnoses among HIV-negative MSM during 2017–2019 is in line with reports from other countries in Europe (6,8,14,15).
The first limitation of this study is that unmeasured behavioral covariates (e.g., number of partners, PrEP use, drug use, group sex, and venue-based activities) were not available. Inclusion of behavioral covariates in routine STI surveillance in England is underway and will be examined in future iterations of these analyses. Second, the risk among some groups, such as those not born in the United Kingdom, could be overestimated because of differing patterns of healthcare access and barriers to access.
In summary, we report a steep increase in the number of LGV diagnoses identified in SHS sites after a period of decline, which indicates the need for sustained surveillance and public health action. Our findings indicate that the epidemiology of LGV has changed, and an increased number of diagnoses are occurring among MSM who are HIV-negative or with unknown HIV status, highlighting the need to integrate health promotion and increase LGV testing within HIV prevention delivery. In addition, increased LGV risk among MSM born in LAC and in countries in Europe that are outside the United Kingdom indicates the need for increased accessibility of health promotion materials and wider engagement with these communities.
Dr. Prochazka is a medical doctor and epidemiologist focused on control of infectious diseases. He is a consultant epidemiology scientist supporting STI and COVID-19 surveillance at Public Health England.
References
- Childs T, Simms I, Alexander S, Eastick K, Hughes G, Field N. Rapid increase in lymphogranuloma venereum in men who have sex with men, United Kingdom, 2003 to September 2015. Euro Surveill. 2015;20:30076. DOIPubMedGoogle Scholar
- Hughes G, Alexander S, Simms I, Conti S, Ward H, Powers C, et al.; LGV Incident Group. Lymphogranuloma venereum diagnoses among men who have sex with men in the U.K.: interpreting a cross-sectional study using an epidemic phase-specific framework. Sex Transm Infect. 2013;89:542–7. DOIPubMedGoogle Scholar
- Saxon C, Hughes G, Ison C; UK LGV Case-Finding Group. Asymptomatic lymphogranuloma venereum in men who have sex with men, United Kingdom. Emerg Infect Dis. 2016;22:112–6. DOIPubMedGoogle Scholar
- Cole MJ, Field N, Pitt R, Amato-Gauci AJ, Begovac J, French PD, et al. Substantial underdiagnosis of lymphogranuloma venereum in men who have sex with men in Europe: preliminary findings from a multicentre surveillance pilot. Sex Transm Infect. 2020;96:137–42. DOIPubMedGoogle Scholar
- Nwokolo NC, Dragovic B, Patel S, Tong CY, Barker G, Radcliffe K. 2015 UK national guideline for the management of infection with Chlamydia trachomatis. Int J STD AIDS. 2016;27:251–67. DOIPubMedGoogle Scholar
- van Aar F, Kroone MM, de Vries HJ, Götz HM, van Benthem BH. Increasing trends of lymphogranuloma venereum among HIV-negative and asymptomatic men who have sex with men, the Netherlands, 2011 to 2017. Euro Surveill. 2020;25:25. DOIPubMedGoogle Scholar
- Peuchant O, Touati A, Laurier-Nadalié C, Hénin N, Cazanave C, Bébéar C, et al. Prevalence of lymphogranuloma venereum among anorectal Chlamydia trachomatis-positive MSM using pre-exposure prophylaxis for HIV. Sex Transm Infect. 2020;96:615–7. DOIPubMedGoogle Scholar
- De Baetselier I, Tsoumanis A, Verbrugge R, De Deken B, Smet H, Abdellati S, et al. Lymphogranuloma venereum is on the rise in Belgium among HIV negative men who have sex with men: surveillance data from 2011 until the end of June 2017. BMC Infect Dis. 2018;18:689. DOIPubMedGoogle Scholar
- Allen H, Pitt R, Bardsley M, Smolarchuk C, Sullivan A, Mohammed H, et al. Investigating the decline in Lymphogranuloma venereum diagnoses in men who have sex with men in the United Kingdom since 2016: an analysis of surveillance data. Sex Health. 2020;17:344–51. DOIPubMedGoogle Scholar
- Charles H, Prochazka M, Sinka K. Trends of lymphogranuloma venereum in England: 2019. Health Protection Report. 2020;14 [cited 2021 Feb 9]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/942751/hpr2320_LGV-10.pdf
- Public Health England. GUMCAD STI Surveillance System: data specification and technical guidance. 2020 Apr [cited 2021 Feb 9]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/879785/GUMCAD_Data_Specification_and_Technical_Guidance.pdf
- White J, O’Farrell N, Daniels D; British Association for Sexual Health and HIV. 2013 UK national guideline for the management of lymphogranuloma venereum. Int J STD AIDS. 2013;24:593–601. DOIPubMedGoogle Scholar
- Gafos M, Horne R, Nutland W, Bell G, Rae C, Wayal S, et al. The context of sexual risk behaviour among men who have sex with men seeking PrEP, and the impact of PrEP on sexual behaviour. AIDS Behav. 2019;23:1708–20. DOIPubMedGoogle Scholar
- Marangoni A, Foschi C, Tartari F, Gaspari V, Re MC. Lymphogranuloma venereum genovariants in men having sex with men in Italy. Sex Transm Infect. Sex Transm Infect. 2020 Oct 26 [Epub ahead of print].
- Martínez-García L, Rodríguez-Domínguez M, Lejarraga C, Rodríguez-Jiménez MC, González-Alba JM, Puerta T, et al. The silent epidemic of lymphogranuloma venereum inside the COVID-19 pandemic in Madrid, Spain, March 2020 to February 2021. Euro Surveill. 2021;26:
2100422 . DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: August 27, 2021
Table of Contents – Volume 27, Number 10—October 2021
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Address for corresponding: Hannah Charles, Public Health England, 61 Colindale Ave, London, NW9 5EQ, UK; emailhannah.charles@phe.gov.uk
Top