Volume 27, Number 5—May 2021
Synopsis
Coccidioidomycosis and COVID-19 Co-Infection, United States, 2020
Figure 1
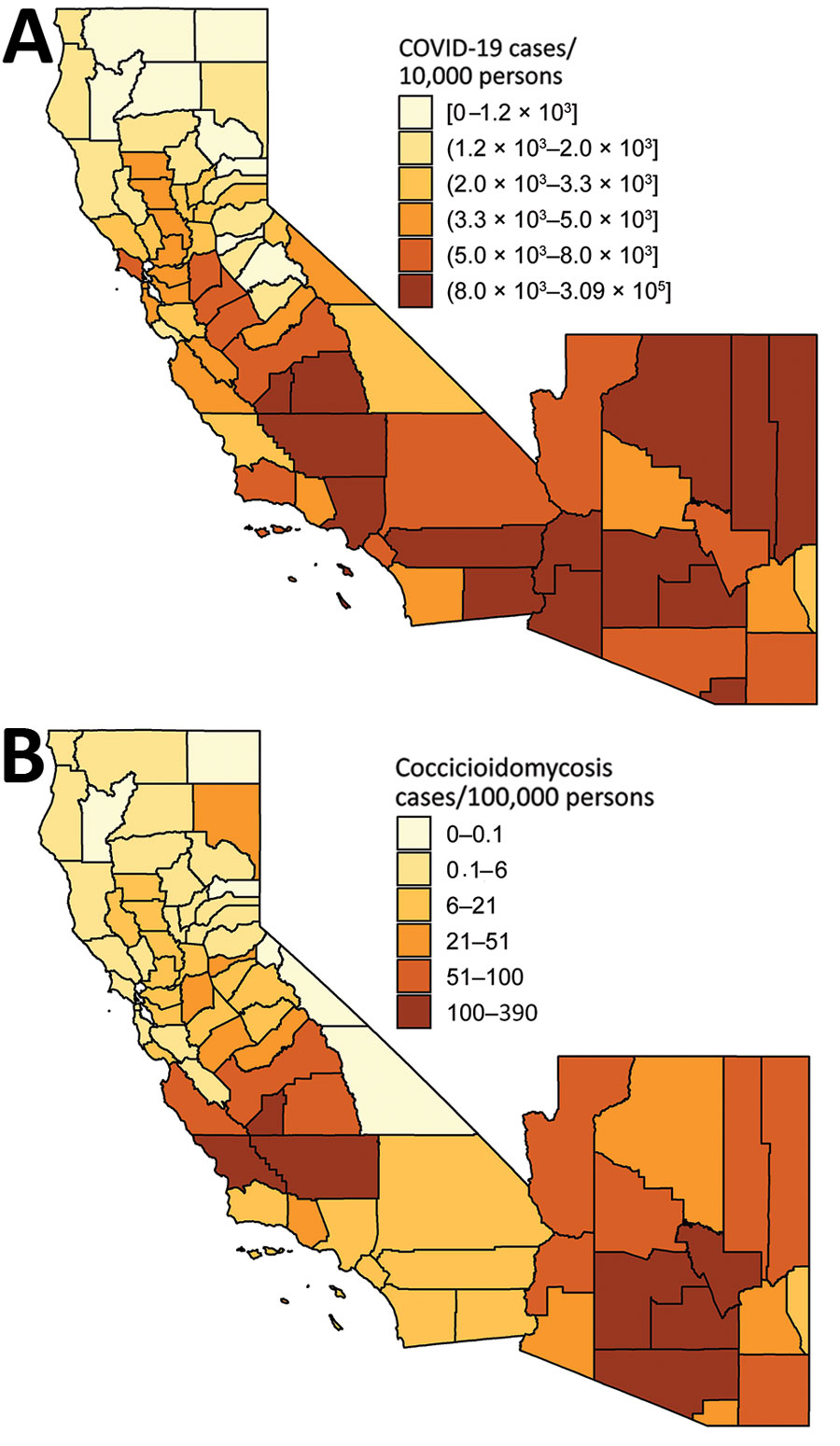
Figure 1. County-level incidence of (A) coronavirus disease (COVID-19) in 2020 and (B) coccidioidomycosis in 2019, California and Arizona. COVID-19 incidence reflects cumulative case count as of August 14, 2020 (5). Coccidioidomycosis incidence reflects annual incidence in 2019 (6,7). Shading indicates levels of incidence. Brackets indicate inclusive bounds; parentheses indicate exclusive bounds.
References
- Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of Covid-19 in New York City. N Engl J Med. 2020;382:2372–4. DOIPubMedGoogle Scholar
- Blair JE, Chang YHH, Cheng MR, Vaszar LT, Vikram HR, Orenstein R, et al. Characteristics of patients with mild to moderate primary pulmonary coccidioidomycosis. Emerg Infect Dis. 2014;20:983–90. DOIPubMedGoogle Scholar
- California Department of Public Health. Epidemiological summary of coccidioidomycosis in California, 2018. 2019 [cited 2020 May 18]. https://www.cdph.ca.gov/Programs/CID/DCDC/CDPH%20Document%20Library/CocciEpiSummary2018.pdf
- Centers for Disease Control and Prevention. Valley fever (coccidiomycosis) statistics. 2020 [cited 2020 May 14]. https://www.cdc.gov/fungal/diseases/coccidioidomycosis/statistics.html
- USAFacts. US coronavirus cases and deaths by state. 2020 [cited 2020 May 21]. https://usafacts.org/visualizations/coronavirus-covid-19-spread-map
- California Department of Public Health. Coccidioidomycosis in California provisional monthly report: January–April 2020. 2020 [cited 2020 May 28]. https://www.cdph.ca.gov/Programs/CID/DCDC/CDPH%20Document%20Library/CocciinCAProvisionalMonthlyReport.pdf
- Arizona Department of Health Services. Valley fever 2019 annual report. 2021 [cited 2021 Feb 24]. https://www.azdhs.gov/documents/preparedness/epidemiology-disease-control/valley-fever/reports/valley-fever-2019.pdf
- Levan NE, Huntington RW. Primary cutaneous coccidioidomycosis in agricultural workers. Arch Dermatol. 1965;92:215–20.
- Schmelzer LL, Tabershaw IR. Exposure factors in occupational coccidioidomycosis. Am J Public Health Nations Health. 1968;58:107–13.
- Johnson WM. Occupational factors in coccidioidomycosis. J Occup Med. 1981;23:367–74.
- Freedman M, Jackson BR, McCotter O, Benedict K. Coccidioidomycosis outbreaks, United States and worldwide, 1940–2015. Emerg Infect Dis. 2018;24:417–23. DOIPubMedGoogle Scholar
- Das R, McNary J, Fitzsimmons K, Dobraca D, Cummings K, Mohle-Boetani J, et al. Occupational coccidioidomycosis in California: outbreak investigation, respirator recommendations, and surveillance findings. J Occup Environ Med. 2012;54:564–71. DOIPubMedGoogle Scholar
- Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: A key factor in containing risk of COVID-19 infection. PLoS One. 2020;15:
e0232452 . DOIPubMedGoogle Scholar - Brown S, Brooks R, Dong XS. Coronavirus and health disparities in construction. The Center for Construction Research and Training. 2020 [cited 2020 Oct 16]. https://www.cpwr.com/wp-content/uploads/publications/DataBulletin-May2020.pdf
- Acs G, Loprest PJ. Job differences by race and ethnicity in the low-skill job market. The Urban Institute. 2009 [cited 2020 Jun 15]. https://www.urban.org/sites/default/files/publication/30146/411841-Job-Differences-by-Race-and-Ethnicity-in-the-Low-Skill-Job-Market.PDF
- Murray CJL, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med. 2006;3:
e260 . DOIPubMedGoogle Scholar - Centers for Disease Control and Prevention. Communities, schools, workplaces, and events. 2020 [cited 2020 Oct 16]. https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-agricultural-workers.html
- Arcury TA, Weir M, Chen H, Summers P, Pelletier LE, Galván L, et al. Migrant farmworker housing regulation violations in North Carolina. Am J Ind Med. 2012;55:191–204.
- Quandt SA, Brooke C, Fagan K, Howe A, Thornburg TK, McCurdy SA. Farmworker housing in the United States and its impact on health. New Solut. 2015;25:263–86.
- Simpson PL, Simpson M, Adily A, Grant L, Butler T. Prison cell spatial density and infectious and communicable diseases: a systematic review. [Erratum in: BMJ Open. 2020;10: e026806corr1]. BMJ Open. 2019;9:
e026806 . DOIPubMedGoogle Scholar - Sabalow R, Pohl J. California severely short on firefighting crews after COVID-19 lockdown at prison camps. The Sacramento Bee. 2020 [cited 2020 Aug 18]. https://www.sacbee.com/news/california/fires/article243977827.html
- Lucas KD, Wheeler C, Mohle-Boetani JC. Coccidioidomycosis outbreaks among inmate wildland firefighters in California. Proceedings of the 63rd Coccidioidomycosis Study Group Annual Meeting; 2019 Apr 5–6. Sacramento, CA, USA.
- MacLean M. Epidemiology of coccidioidomycosis—15 California counties, 2007–2011. 2014 [cited 2020 May 28]. https://www.vfce.arizona.edu/sites/vfce/files/the_epidemiology_of_coccidioidomycosis_collaborative_county_report.pdf
- The New York Times. Coronavirus in the U.S.: latest map and case count. 2020 [cited 2020 May 28]. https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html?auth=login-email&login=email
- Prison Law Office. Valley fever and CDCR housing. 2019 [cited 2020 May 28]. https://prisonlaw.com/wp-content/uploads/2019/04/Valley-Fever-info-April-2019.pdf
- Wallace M, Hagan L, Curran KG, Williams SP, Handanagic S, Bjork A, et al. COVID-19 in correctional and detention facilities—United States, February–April 2020. MMWR Morb Mortal Wkly Rep. 2020;69:587–90. DOIPubMedGoogle Scholar
- California Department of Public Health. COVID-19 race and ethnicity data. 2020 [cited 2020 Jun 15]. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/Race-Ethnicity.aspx
- Moore JT, Ricaldi JN, Rose CE, Fuld J, Parise M, Kang GJ, et al.; COVID-19 State, Tribal, Local, and Territorial Response Team. Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5–18, 2020—22 states, February–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1122–6. DOIPubMedGoogle Scholar
- Zelner J, Trangucci R, Naraharisetti R, Cao A, Malosh R, Broen K, et al. Racial disparities in COVID-19 mortality are driven by unequal infection risks. Clin Infect Dis. 2020;72:e88–95.
- Thomason S, Bernhardt A. Front-line essential jobs in California: a profile of job and worker characteristics. UC Berkeley Labor Center. 2020 [cited 2020 Aug 18]. https://laborcenter.berkeley.edu/front-line-essential-jobs-in-california-a-profile-of-job-and-worker-characteristics/
- United States Department of Agriculture. Farm labor. 2020 [cited 2020 Jun 15]. https://www.ers.usda.gov/topics/farm-economy/farm-labor/#demographic
- United States Census Bureau. Five-year public use microdata sample (PUMS), 2014–2018. 2020 [cited 2020 Jun 15]. https://www.census.gov/programs-surveys/acs/technical-documentation/pums/documentation.html
- United States Census Bureau. 2010 census summary file 1. 2016 [cited 2020 Jun 5]. https://www.census.gov/data/datasets/2010/dec/summary-file-1.html<eref[REMOVED IF= FIELD]></eref>
- Chow NA, Griffin DW, Barker BM, Loparev VN, Litvintseva AP. Molecular detection of airborne Coccidioides in Tucson, Arizona. Med Mycol. 2016;54:584–92.
- Pappagianis D, Einstein H. Tempest from Tehachapi takes toll or Coccidioides conveyed aloft and afar. West J Med. 1978;129:527–30.
- Das R, McNary J, Fitzsimmons K, Dobraca D, Cummings K, Mohle-Boetani J, et al. Occupational coccidioidomycosis in California: outbreak investigation, respirator recommendations, and surveillance findings. J Occup Environ Med. 2012;54:564–71. PubMedGoogle Scholar
- Cummings KC, McDowell A, Wheeler C, McNary J, Das R, Vugia DJ, et al. Point-source outbreak of coccidioidomycosis in construction workers. Epidemiol Infect. 2010;138:507–11.
- Petersen LR, Marshall SL, Barton C, Hajjeh RA, Lindsley MD, Warnock DW, et al. Coccidioidomycosis among workers at an archeological site, northeastern Utah. Emerg Infect Dis. 2004;10:637–42.
- Standaert SM, Schaffner W, Galgiani JN, Pinner RW, Kaufman L, Durry E, et al. Coccidioidomycosis among visitors to a Coccidioides immitis–endemic area: an outbreak in a military reserve unit. J Infect Dis. 1995;171:1672–5.
- Wilken JA, Sondermeyer G, Shusterman D, McNary J, Vugia DJ, McDowell A, et al. Coccidioidomycosis among workers constructing solar power farms, California, USA, 2011–2014. Emerg Infect Dis. 2015;21:1997–2005.
- de Perio MA, Materna BL, Sondermeyer Cooksey GL, Vugia DJ, Su CP, Luckhaupt SE, et al. Occupational coccidioidomycosis surveillance and recent outbreaks in California. Med Mycol. 2019;57:S41–5.
- Gorris ME, Cat LA, Zender CS, Treseder KK, Randerson JT. Coccidioidomycosis dynamics in relation to climate in the southwestern United States. Geohealth. 2018;2:6–24.
- Schneider E, Hajjeh RA, Spiegel RA, Jibson RW, Harp EL, Marshall GA, et al. A coccidioidomycosis outbreak following the Northridge, Calif, earthquake. JAMA. 1997;277:904–8.
- Sondermeyer Cooksey GL, Wilken JA, McNary J, Gilliss D, Shusterman D, Materna BL, et al. Dust exposure and coccidioidomycosis prevention among solar power farm construction workers in California. Am J Public Health. 2017;107:1296–303. DOIPubMedGoogle Scholar
- Galgiani JN, Ampel NM, Blair JE, Catanzaro A, Johnson RH, Stevens DA, et al.; Infectious Diseases Society of America. Coccidioidomycosis. Clin Infect Dis. 2005;41:1217–23. DOIPubMedGoogle Scholar
- Galgiani JN, Blair JE, Ampel NM, Thompson GR. Treatment for early, uncomplicated coccidioidomycosis: what is success? Clin Infect Dis. 2020;70:2008–12. DOIPubMedGoogle Scholar
- Valdivia L, Nix D, Wright M, Lindberg E, Fagan T, Lieberman D, et al. Coccidioidomycosis as a common cause of community-acquired pneumonia. Emerg Infect Dis. 2006;12:958–62. DOIPubMedGoogle Scholar
- Chang DC, Anderson S, Wannemuehler K, Engelthaler DM, Erhart L, Sunenshine RH, et al. Testing for coccidioidomycosis among patients with community-acquired pneumonia. Emerg Infect Dis. 2008;14:1053–9. DOIPubMedGoogle Scholar
- Tsang CA, Anderson SM, Imholte SB, Erhart LM, Chen S, Park BJ, et al. Enhanced surveillance of coccidioidomycosis, Arizona, USA, 2007-2008. Emerg Infect Dis. 2010;16:1738–44. DOIPubMedGoogle Scholar
- Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect. 2020;80:656–65.
- Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of Covid-19 in New York City. N Engl J Med. 2020;382:2372–4.
Page created: March 02, 2021
Page updated: April 20, 2021
Page reviewed: April 20, 2021
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.