Volume 27, Number 6—June 2021
Dispatch
Molecular Characterization and Antimicrobial Resistance in Neisseria gonorrhoeae, Nunavut Region of Inuit Nunangat, Canada, 2018–2019
Abstract
We assessed antimicrobial resistance (AMR) in Neisseria gonorrhoeae in Nunavut, Canada, using remnant gonorrhea nucleic acid amplification test–positive urine specimens. This study confirms the feasibility of conducting N. gonorrhoeae AMR surveillance and highlights the diversity of gonococcal sequence types and geographic variation of AMR patterns in the territory.
In 2015, the prevalence of Neisseria gonorrhoeae reported in the territory of Nunavut, Canada, 837.6 cases/100,000 residents, was 15 times the national rate in Canada (55.4 cases/100,000 residents) (1). Gonorrhea is a notifiable disease in Nunavut, and all positive cases are reported to the department of health. Globally, reports are increasing of N. gonorrhoeae with resistance to currently recommended first-line antimicrobial treatment agents (2). These resistance rates in some global regions approach or exceed World Health Organization thresholds of 5% to warrant changes to the prescribed gonorrhea treatments (3).
The Gonococcal Antimicrobial Surveillance Program of Canada is a culture-based laboratory surveillance system monitoring antimicrobial resistance (AMR) trends and gonococcal sequence types (STs) in N. gonorrhoeae (4). Traditionally, N. gonorrhoeae AMR surveillance has required obtaining cultures from patients for phenotypic testing. In the Canadian Arctic regions, including Nunavut, no information has been available on the prevalence and distribution of N. gonorrhoeae AMR patterns because long transport times and conditions preclude transporting cultures; assessment is exclusively done by using nucleic acid amplification tests (NAATs). The National Microbiology Laboratory (Winnipeg, Manitoba, Canada) has addressed this issue by developing molecular assays to predict AMR and molecular STs from remnant NAAT specimens. We sought to assess the prevalence and distribution of AMR N. gonorrhoeae STs in Nunavut using NAAT-tested N. gonorrhoeae–positive specimens.
Nunavut, at 1,877,787 km2 the largest territory in Canada, is divided into 3 regions: Qikiqtaaluk (also called Qikiqtani) in the east, Kivalliq in the center, and Kitikmeot in the west. Nunavut’s reported 2016 population was 35,994 (5), ≈85% of whom identify as Inuit (6). Nunavut is one region in Inuit Nunangat, a Canadian Inuktitut term inclusive of the land, water, and ice of the Inuit homeland (7).
For this study we used remnant N. gonorrhoeae NAAT–positive specimens collected in Nunavut for routine gonococcal diagnostics during January 1, 2018–December 31, 2019. We submitted specimens from the Kitikmeot region to DynaLife Laboratories (https://www.dynalife.ca) and from the Qikiqtaaluk and Kivalliq regions to the Qikiqtani General Hospital Laboratory (Iqaluit, Nunavut, Canada) to the National Microbiology Laboratory for molecular antimicrobial susceptibility prediction using NAATs and N. gonorrhoeae multiantigen sequence typing (NG-MAST). Urine specimens submitted to DynaLife laboratories were tested using the Gen-Probe Aptima Combo 2 test (Hologic, https://www.hologic.com). Testing at the Qikiqtani General Hospital Laboratory was done using the Roche-Cobas test (Roche Molecular Diagnostics, https://diagnostics.roche.com). We did not submit repeat samples or test-of-cure specimens. Ethics approval was obtained from the University of Alberta’s Health Research Ethics Board and the Nunavut Research Institute.
We performed NG-MAST as described elsewhere (8,9). We then tested specimens successfully typed with NG-MAST using single-nucleotide polymorphism (SNP) assays targeting cephalosporin-DS mutations (ponA, mtrR delA, porB, penA A311V, penA A501, penA N513Y, and penA G545S), ciprofloxacin-resistance mutations (gyrA and parC), and azithromycin-resistance mutations (23S rRNA A2059G, C2611T, and mtrR) to predict antimicrobial susceptibility. We performed DNA extraction, preparation, real-time PCR, and results analysis as described elsewhere (9,10). For specimens identified with the same ST, we performed SNP assay testing for a subset of samples and for the remainder of samples within identical ST groups. We inferred AMR profiles based on STs with 4–70 samples if ≥50% of those samples had identical AMR predictions based on SNP results and STs with >70 samples if ≥30 samples were tested with identical AMR predictions. These results are molecular based and have been validated against MIC phenotypes in a previous study (9).
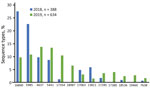
All NAAT-tested N. gonorrhoeae–positive specimens (n = 1,128) from Nunavut collected between January 1, 2018–December 31, 2019, were included in the study (Table 1). Of these, 106 (9.4%) samples were nontypeable for NG-MAST because of low concentrations of DNA and therefore excluded from further testing. We identified a total of 75 different STs among the remaining 1,022 NAAT-identified isolates from samples submitted from Nunavut (Figure 1). The most prevalent was ST16840 (16.5%), followed by ST5985 (15.3%).
SNP assay results for predicting AMR were successfully determined for cephalosporin (687 samples), ciprofloxacin (541 samples), and azithromycin (435 samples). We predicted AMR for an additional 289 cephalosporin results, 436 ciprofloxacin results, and 533 azithromycin results on the basis of expected results of prevalent STs tested (Table 2). Within Nunavut, the Qikiqtaaluk region had the highest prevalence of intermediate cephalosporin MICs (51.3%) and resistance to azithromycin (11.3%). The Kivalliq region had the only sample (0.3%) with predicted decreased susceptibility to cephalosporins. We inferred the genetic relationships between the NG-MAST STs by using the maximum-likelihood method and Tamura-Nei model (Figure 2) (11,12). We predicted most samples in clusters A, B, and D would have elevated MICs to cephalosporins but that most samples in cluster C would have azithromycin resistance. We also found that STs were clustered based on geography: in Qikiqtaaluk, we primarily identified STs from clusters A, B and C, but we identified STs from cluster D in all 3 jurisdictions.
Our analysis of routinely collected diagnostic specimens for gonorrhea from Nunavut highlights the usefulness of SNP assays and NG-MAST typing in identifying population-level N. gonorrhoeae AMR and delineating transmission patterns (9). Current Nunavut treatment guidelines for gonorrhea recommend dual ceftriaxone/azithromycin therapy (13). Although decreased susceptibility to cephalosporins was identified in only 1 sample, the rate of predicted intermediate cephalosporin MICs in Nunavut at 36.9% is >2 times as high as the national rate of 16% in 2018, potentially limiting the long-term use of this agent (4). In addition, the 7.0% rate of predicted azithromycin resistance exceeds the World Health Organization threshold of 5% above which a drug is not routinely recommended for treatment (3). We also noted substantial geographic variation; the highest prevalence of predicted intermediate cephalosporin MICs (51.3%) and predicted resistance to azithromycin (11.3%) were in the Qikiqtaaluk region. In the adjacent province of Quebec, the reported rate of intermediate cephalosporin MICs was 22% and azithromycin resistance was 11.8% (4). NG-MAST typing detected a large number of STs, reflecting the genetic diversity of N. gonorrhoeae and suggesting the introduction of multiple strains into the territory.
The first limitation of our study was that no gonococcal cultures were available and cases were compared to national gonococcal cultures, which may not be representative of gonorrhea in all regions. In addition, only urine specimens were collected for gonorrhea in Nunavut. Previous research has highlighted the variability in ST from extragenital sites (14,15). There are limitations to using culture-independent techniques to predict AMR because specimens often contain low concentrations of DNA, which can limit SNP detection. Gonococcus is also known to mutate easily, which may lead to false-negative results in the SNP assays because of sequence variations in DNA (9). A molecular-based approach may overestimate AMR because mutations associated with resistance do not always correlate phenotypically. Finally, we acknowledge the biomedical and technical laboratory approach of this work and the limited partnerships with the Inuit people.
Because research across Inuit Nunangat has historically often been done in an exploitative way that has not respected Inuit self-determination, meaningful partnerships are required to prioritize research activities and develop approaches that add value for and are accepted by communities. Our findings highlight the feasibility of conducting molecular surveillance for N. gonorrhoeae AMR using remnant N. gonorrhoeae–positive NAAT specimens Data based on these findings can be used to provide Nunavut with up-to-date information about the best choices to treat gonorrhea.
Dr. Singh is a clinical professor with the Division of Infectious Diseases at the University of Alberta in Edmonton. Her primary research interests are clinical and epidemiologic aspects of bacterial STIs, HIV biomedical prevention, and the use of rapid diagnostic tests for diagnosing syphilis and HIV.
Acknowledgments
We thank Pam Sawatzky, Norman Barairo, and Shelley Peterson for technical assistance.
This project was supported by internal funding from the Public Health Agency of Canada and Indigenous Services Canada.
References
- Choudhri Y, Miller J, Sandhu J, Leon A, Aho J. Gonorrhea in Canada, 2010-2015. Can Commun Dis Rep. 2018;44:37–42. DOIPubMedGoogle Scholar
- Unemo M, Seifert HS, Hook EW III, Hawkes S, Ndowa F, Dillon JR. Gonorrhoea. Nat Rev Dis Primers. 2019;5:79. DOIPubMedGoogle Scholar
- World Health Organization, Department of Reproductive Health and Research. Global action plan to control the spread and impact of antimicrobial resistance in Neisseria gonorrhoeae. 2012 [cited 2021 Apr 21]. https://www.who.int/reproductivehealth/publications/rtis/9789241503501/en
- Public Health Agency of Canada, National Microbiology Laboratory. 2020. National surveillance of antimicrobial susceptibilities of Neisseria gonorrhoeae annual summary 2018 [cited 2021 Apr 21]. https://www.canada.ca/en/public-health/services/publications/drugs-health-products/national-surveillance-antimicrobial-susceptibilities-neisseria-gonorrhoeae-annual-summary-2018.html
- Statistics Canada. Population and dwelling count highlight tables, 2016 census [cited 2021 Apr 21]. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/hlt-fst/pd-pl/Table.cfm?Lang=Eng&T=101&SR=1&S=3&O=D#tPopDwell
- Nunavut Tunngavik Incorporated. Annual report on the state of Inuit culture and society, 2007–8 [cited 2021 Apr 21]. https://www.tunngavik.com/publications/annual-report-on-the-state-of-inuit-culture-and-society-2007-2008
- Kanatami IT. National Inuit strategy on research, 2018 [cited 2021 Apr 21]. https://www.itk.ca/wp-content/uploads/2018/04/ITK_NISR-Report_English_low_res.pdf
- Martin IM, Ison CA, Aanensen DM, Fenton KA, Spratt BG. Rapid sequence-based identification of gonococcal transmission clusters in a large metropolitan area. J Infect Dis. 2004;189:1497–505. DOIPubMedGoogle Scholar
- Peterson S, Martin I, Demczuk W, Barairo N, Naidu P, Lefebvre B, et al. Multiplex real-time polymerase chain reaction assays for the prediction of cephalosporin, ciprofloxacin, and azithromycin antimicrobial susceptibility of positive Neisseria gonorrhoeae nucleic acid amplification test samples. J Antimicrob Chemother. 2020;75:3485–90. DOIPubMedGoogle Scholar
- Trembizki E, Buckley C, Donovan B, Chen M, Guy R, Kaldor J, et al. Direct real-time PCR-based detection of Neisseria gonorrhoeae 23S rRNA mutations associated with azithromycin resistance. J Antimicrob Chemother. 2015;70:3244–9.PubMedGoogle Scholar
- Tamura K, Nei M. Estimation of the number of nucleotide substitutions in the control region of mitochondrial DNA in humans and chimpanzees. Mol Biol Evol. 1993;10:512–26.PubMedGoogle Scholar
- Kumar S, Stecher G, Li M, Knyaz C, Tamura K. MEGA X: molecular evolutionary genetics analysis across computing platforms. Mol Biol Evol. 2018;35:1547–9. DOIPubMedGoogle Scholar
- Gonorrhea public health protocol. Nunavut communicable disease and surveillance manual. Iqaluit (Canada): Nunavut Department of Health. 2018.
- Didelot X, Dordel J, Whittles LK, Collins C, Bilek N, Bishop CJ, et al. Genomic analysis and comparison of two gonorrhea outbreaks. MBio. 2016;7:e00525–16. DOIPubMedGoogle Scholar
- Ota KV, Fisman DN, Tamari IE, Smieja M, Ng L-K, Jones KE, et al. Incidence and treatment outcomes of pharyngeal Neisseria gonorrhoeae and Chlamydia trachomatis infections in men who have sex with men: a 13-year retrospective cohort study. Clin Infect Dis. 2009;48:1237–43. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: May 10, 2021
Table of Contents – Volume 27, Number 6—June 2021
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Ameeta Singh, University of Alberta, Edmonton, 3B20-111 Jasper Ave, Edmonton, AB T5K 0L4, Canada
Top