Volume 28, Number 10—October 2022
Dispatch
Anisakiasis Annual Incidence and Causative Species, Japan, 2018–2019
Figure 2
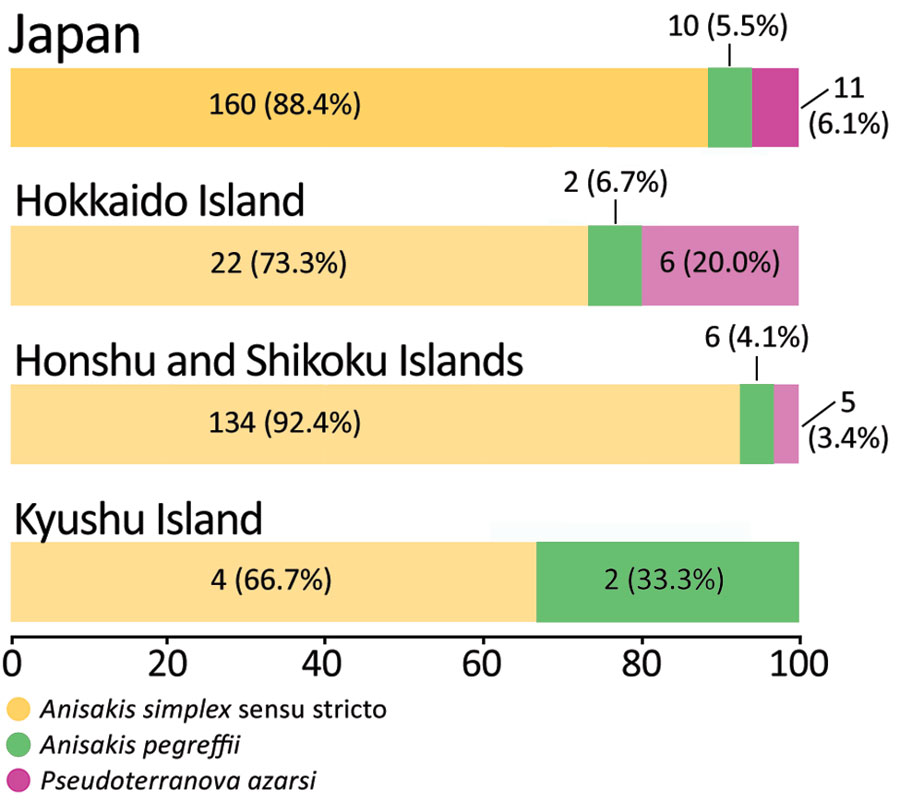
Figure 2. Analyzed number and percentage of anisakiasis patients and causative species, Japan, 2018–2019. One third (2/6) of patients in the Kyushu Island had Anisakis pegreffii infections. A. pegreffii–carrying fish are predominant in the Sea of Japan and the East China Sea, located between South Korea and Japan (11). Over 50% (6/11) of the patients with Pseudoterranova azarasi infection were from Hokkaido.
References
- Naylor RL, Kishore A, Sumaila UR, Issifu I, Hunter BP, Belton B, et al. Blue food demand across geographic and temporal scales. Nat Commun. 2021;12:5413. DOIPubMedGoogle Scholar
- Lim H, Jung BK, Cho J, Yooyen T, Shin EH, Chai JY. Molecular diagnosis of cause of anisakiasis in humans, South Korea. Emerg Infect Dis. 2015;21:342–4. DOIPubMedGoogle Scholar
- Shamsi S, Butcher AR. First report of human anisakidosis in Australia. Med J Aust. 2011;194:199–200. DOIPubMedGoogle Scholar
- Food and Agriculture Organization of the United Nations. FAO yearbook. Fishery and aquaculture statistics 2019. Rome: The Organization; 2021. DOIGoogle Scholar
- Sugiyama H. [Food and parasitic infections] [in Japanese]. Shokuhin Eiseigaku Zasshi. 2010;51:285–91. DOIPubMedGoogle Scholar
- Director-General, Department of Food Safety, Pharmaceutical and Food Safety Bureau, Ministry of Health, Labour and Welfare. Partial revision of the ordinance for enforcement of the Food Sanitation Act [in Japanese]. 2012 Dec 28; Notification shokuan no. 1228–7 [cited 2022 Apr 11]. https://www.mhlw.go.jp/topics/bukyoku/iyaku/syoku-anzen/gyousei/dl/121228_2.pdf.
- Kubota K, Kasuga F, Iwasaki E, Inagaki S, Sakurai Y, Komatsu M, et al. Estimating the burden of acute gastroenteritis and foodborne illness caused by Campylobacter, Salmonella, and Vibrio parahaemolyticus by using population-based telephone survey data, Miyagi Prefecture, Japan, 2005 to 2006. J Food Prot. 2011;74:1592–8. DOIPubMedGoogle Scholar
- Kimura S, Sato T, Ikeda S, Noda M, Nakayama T. Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol. 2010;20:413–9. DOIPubMedGoogle Scholar
- Ohisa M, Kimura Y, Matsuo J, Akita T, Sato T, Matsuoka T, et al. Estimated numbers of patients with liver disease related to hepatitis B or C virus infection based on the database reconstructed from medical claims from 2008 to 2010 in Japan. Hepatol Res. 2015;45:1228–40. DOIPubMedGoogle Scholar
- Bao M, Pierce GJ, Pascual S, González-Muñoz M, Mattiucci S, Mladineo I, et al. Assessing the risk of an emerging zoonosis of worldwide concern: anisakiasis. Sci Rep. 2017;7:43699. DOIPubMedGoogle Scholar
- Suzuki J, Murata R, Kodo Y. Current status of anisakiasis and Anisakis larvae in Tokyo, Japan. Food Saf (Tokyo). 2021;9:89–100. DOIPubMedGoogle Scholar
- Arizono N, Miura T, Yamada M, Tegoshi T, Onishi K. Human infection with Pseudoterranova azarasi roundworm. Emerg Infect Dis. 2011;17:555–6. DOIPubMedGoogle Scholar
- Torres P, Jercic MI, Weitz JC, Dobrew EK, Mercado RA. Human pseudoterranovosis, an emerging infection in Chile. J Parasitol. 2007;93:440–3. DOIPubMedGoogle Scholar
- Nakaji K, Kumamoto M, Wada Y, Nakae Y. Asymptomatic gastric and colonic anisakiasis detected simultaneously. Intern Med. 2019;58:2263–4. DOIPubMedGoogle Scholar
- Song H, Jung BK, Cho J, Chang T, Huh S, Chai JY. Molecular identification of Anisakis larvae extracted by gastrointestinal endoscopy from health check-up patients in Korea. Korean J Parasitol. 2019;57:207–11. DOIPubMedGoogle Scholar
Page created: September 15, 2022
Page updated: September 22, 2022
Page reviewed: September 22, 2022
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.